In the recent years, new humanized anti-CD20 monoclonal antibodies have been developed to optimize B-cell depletion. Our objective is to describe the experience at our center with the use of new anti-CD20 drugs in glomerular diseases. We included patients from our center treated with second-generation anti-CD20 monoclonal antibodies for glomerular diseases between January 2017 and January 2024. Patients were followed for one year after the initiation of treatment. Six patients were included, 2 (33%) men, with a median age of 59.5 (49–75) years. Diagnoses were 2 (33%) minimal change disease, 1 (16.7%) mixed cryoglobulinemia type-II, 1 (16.7%) membranous nephropathy, 1 (16.7%) fibrillary glomerulonephritis (FGN), and 1 (16.7%) focal segmental glomerulosclerosis. The indications for the new anti-CD20 therapy were 4 (66%) for refractory disease, 1 (16.7%) recurrent flares, and 1 (16.7%) due to an anaphylactic reaction to rituximab. The new anti-CD20 used were obinutuzumab in 4 (66%) and ofatumumab in 2 patients (33%). Before the start of the treatment median creatinine was 1.39mg/dL (0.91–2.38) median serum albumin 2.7g/dL [2.5–3.9g/dL] and urine protein–creatinine ratio (UPCR) 5.75g/g [2.38–4.85g/g]. A total of 5 (83%) patients achieved partial/complete remission within the first 6 months of follow-up. By month twelve of the follow-up 4 (66.67%) patients remained with partial/complete remission. None of the patients had serious side effects. In conclusion, the use of new anti-CD20 therapies for the treatment of immune-mediated glomerular diseases is a safe and effective alternative for its treatment. Further research and clinical trials should be conducted to confirm these positive results.
En los últimos años, se han desarrollado nuevos anticuerpos monoclonales anti-CD20 humanizados para optimizar la depleción de células B. Nuestro objetivo es describir la experiencia en nuestro centro con el uso de nuevos fármacos anti-CD20 en enfermedades glomerulares. Incluimos pacientes de nuestro centro tratados con anti-CD20 de segunda generación para enfermedades glomerulares entre enero de 2017 y enero de 2024. Los pacientes fueron seguidos durante un año. Se incluyeron seis pacientes, 2(33%) hombres, edad media 59,5(49-75) años. Los diagnósticos fueron: 2(33%) enfermedad de cambios mínimos, 1(16,7%) c crioglobulinemia mixta tipo II, 1(16,7%) nefropatía membranosa, 1(16,7%) glomerulonefritis fibrilar (GNF) y 1(16,7%) glomeruloesclerosis segmentaria y focal. Las indicaciones para la nueva terapia anti-CD20 fueron 4(66%) enfermedad refractaria, 1 (16,7%) recurrencias frecuentes, y 1 (16,7%) reacción anafiláctica a rituximab. Los nuevos anti-CD20 utilizados fueron obinutuzumab en 4 (66%) y ofatumumab en 2 pacientes (33%). Antes del inicio del tratamiento, creatinina media 1,39mg/dL (0,91-2,38), albúmina sérica mediana 2,7g/dL [2,5-3,9g/dL] y cociente proteína/creatinina urinaria 5,75g/g [2,38-4,85g/g]. Un total de 5 (83%) pacientes lograron remisión parcial/completa dentro de los primeros 6 meses de seguimiento. A los doce meses, 4 (66,67%) pacientes se mantenían en remisión parcial/completa. Ninguno de los pacientes presentó efectos adversos graves. En conclusión, el uso de nuevas terapias anti-CD20 para el tratamiento de enfermedades glomerulares inmunomediadas es una alternativa segura y eficaz. Se deben realizar más investigaciones y ensayos clínicos para confirmar estos resultados positivos.
B-lymphocyte depletion with anti-CD20 monoclonal antibodies (mAbs) was initially developed for the treatment of B-cell lymphoma.1 Afterwards, treatment with mAbs was extended to immune-related diseases. Indeed, rituximab has long been the principal monoclonal antibody used to treat immune-mediated glomerulopathies.2 It is a human/murine chimeric antibody, which activates natural killer cells, macrophages and neutrophils resulting in antibody-dependent cellular cytotoxicity (ADCC), phagocytosis and induces complement-mediated cell lysis (CDC)3,4 of CD20+ expressing B cells.
In the setting of glomerular diseases, rituximab was firstly used for the treatment of membranous nephropathy with a better safety profile relative to conventional immunosuppressive treatments.2 This led to a broader use in immune-mediated glomerular diseases such as minimal change disease, ANCA-associated vasculitis or focal and segmental glomeruloesclerosis. However, unresponsiveness to rituximab therapy remains a significant clinical challenge.1,3
One of the proposed mechanisms for secondary resistance derives from chimeric nature of rituximab, which makes it highly immunogenic and induces the production of antibodies against its variable region.3 This are the so-called “human antichimeric antibodies” (HACAs) and are reported to be produced in over 20% of patients treated with rituximab.3,5 Another mechanism that has been postulated is the absence of complete B-cell depletion6 due to the poor penetration of the drug, and of MAbs in general, into secondary lymphoid tissues.
The clinical impact of HACAs remains a topic of debate, but some studies have found that it can be associated with higher relapse rates and the need for additional doses of rituximab.1,7 To overcome this limitation, newer generations of anti-CD20 have been developed. These new antibodies have a humanized (ocrelizumab, veltuzumab and obinutuzumab) or fully human (ofatumumab) variable regions.4,7 This new construction of mAb results in reduced immunogenicity and improved effector functions such as CDC and ADCC.4 In glomerular diseases, new mAbs such as obinutuzumab and ocrelizumab have been evaluated in the NOBILITY and BELONG trials, respectively, showed improved renal response as compared with standard of care.4 Beyond clinical trials, case series and single center case reports also suggest new mAbs may be effective alternatives for rituximab in cases without or poor biological and/or clinical responses.8 With this new evidence, we set out to describe the results in our center with the use of new anti-CD20 mAb for immune-mediated glomerulopathies.
Material and methodsStudy design and patientsThis is a retrospective and observational study of patients with immune-mediated glomerulopathies aged at least 18 years old, followed in the Nephrology Department of Vall d’Hebron Hospital. We recruited 6 patients (2 males) that had received treatment with any anti-CD20 mAb other than rituximab as from January 2017. Only patients with native kidneys were accepted. All the patients had a biopsy that confirmed an immune-mediated glomerulopathy. All patients had serum creatinine and urine protein-to-creatinine ratio (UPCR) at the time of the start of the treatment and follow-up analytics at least every three months. The studies involving human participants were reviewed and approved by (AG) 252/2018. The patients/participants provided their written informed consent to participate in this study.
TreatmentAll patients received treatment with a new anti-CD20 and continued this treatment during the follow-up period. The indication for treatment with an anti-CD20 mAb other than rituximab was decided by a committee of experts after treatment failure with rituximab. The new anti-CD20 used were obinutuzumab and ofatumumab which in the case of obinutuzumab is a humanized type II mAb and ofatumumab is a fully human type I mAb. Both are part of the new-anti-CD20 mAb, which are less immunogenic and have a greater cytotoxic effect than rituximab.1 The decision to start obinutuzumab or ofatumumab was solely based on the availability on our center.
Study follow-up and data collectionThe study follow-up period started when the new Anti-CD20 was initiated and continued for a minimum of 3 months. At baseline the following data were collected: age, sex, diagnosis, renal function assessed by serum creatinine and eGFR (calculated with CKD-EPI), serum albumin, 24-h proteinuria or UPCR, CD19+ cells, previous treatments, date of new anti-CD20 initiation. Same data were collected during the next 3 months, 6 months and 1 year. Additionally, we revaluated all the patients for the occurrence of any adverse effects related to the new anti-CD20.
Statistical analysisData was first tested for normal distribution using the Shapiro–Wilk test. Variants with normal distribution were expressed as mean±SD. Nonparametric variables such as proteinuria were expressed as median (interquartile range – IQR: 25th–75th percentiles) and categorical variables as percentages as percentages. Statistical analyses were performed using the SPSS program (SPSS version 20, Chicago, IL).
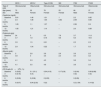
ResultsDemographics and indications for treatmentFrom January 2017 until January 2024, six patients with a diagnosis of an immune-mediated glomerulopathy were treated with obinutuzumab or ofatumumab at our center. Baseline characteristics are shown in Table 1. Two patients (33%) were men, with a median age of 59.5 years (49–75 years). The median creatinine was 1.39mg/dL (0.91–2.38) with a median eGFR of 52.6ml/min/1.73m2. Median serum albumin was 2.7g/dL (2.5–3.63g/dL) and median UPCR was 5.75g/g (2.38–14.85g/g). Diagnoses included minimal change disease (MCD) in 2 patients (33%); 1 (16.7%) type-II mixed cryoglobulinemia; 1 (16.7%) membranous nephropathy (MN); 1 (16.7%) fibrillary glomerulonephritis (FGN) and 1 (16.7%) focal segmental glomerulosclerosis (FSGS). The patient with MN was lost to follow-up, and her clinical status is unknown. All patients had previously received rituximab, the new anti-CD20 mAbs used were obinutuzumab in 4 (66%) patients and ofatumumab in 2 (33%) patients. The indications for switching to a second generation anti-CD20 mAb were the lack of clinical response to rituximab in 4 (66%) patients, an anaphylactic reaction during rituximab infusion in the patient with type-II mixed cryoglobulinemia and frequent relapses in one of the patients with MCD.
Demographics and analytical characteristics.
| MCD-1 | MCD-2 | Type-II CGN | MN | FGN | FSGS | |
|---|---|---|---|---|---|---|
| Type of mAb | Obinutuzumab | Ofatumumab | Obinutuzumab | Obinutuzumab | Obinutuzumab | Ofatumumab |
| Age (years) | 75 | 53 | 76 | 53 | 66 | 37 |
| Sex | Male | Female | Female | Female | Male | Female |
| Creatinine (mg/dL) | ||||||
| Baseline | 5.81 | 1.46 | 1.31 | 1 | 2.2 | 0.65 |
| 3 months | 2.4 | 1.08 | 1.35 | 0.92 | 2.09 | 0.69 |
| 6 months | 1.65 | 1.1 | 1.37 | – | 2.56 | 0.9 |
| 12 months | 1.65 | 1.21 | 1.14 | – | 2.6 | 0.69 |
| Proteinuria (g/g) | ||||||
| Baseline | 24 | 3 | 0.5 | 7.8 | 3.7 | 11.8 |
| 3 months | 3.7 | 1.8 | 0.18 | 9.6 | 5.6 | 10.6 |
| 6 months | 3.5 | 1.5 | 0.01 | – | 2.5 | 2.3 |
| 12 months | 2.9 | 1.04 | 0.22 | – | 1.7 | 5.5 |
| Albumin (g/dL) | ||||||
| Baseline | 2 | 2.8 | 3.9 | 2.6 | 3.9 | 2.5 |
| 3 months | 3.6 | 3 | 4.5 | 2.4 | 3.5 | 3.2 |
| 6 months | 4.1 | 3.3 | 4.3 | – | 3.8 | 3.4 |
| 12 months | 4.1 | 3.5 | 4.6 | – | 3.8 | 3.3 |
| CD19 cells (N×109/L, %) | ||||||
| Baseline | 0 (0.62) | 0.1 (10.1) | 0.04 (4.16) | 0.17 (6.8) | 0 (0.04) | 0.08 (6.68) |
| 3 months | 0 (0.16) | 0 (0) | – | – | 0 (0) | 0 (0) |
| 6 months | 0 (0.09) | 0 (0.08) | 0 (0.03) | – | 0 (0.29) | – |
| 12 months | 0 (0.07) | 0.04 (2.03) | 0 (0) | – | 0.2 (1.54) | 0.14 (9) |
Abbreviations: MCD, minimal change disease; Type-II CGN, mixed cryoglobulinemia type II; MN, membranous nephropathy; FGN, fibrillary glomerulonephritis; FSGS, focal and segmental glomeruloesclerosis.
Baseline Cr had a median of 1.39mg/dL (0.91–2.38) with a median eGFR of 52.6ml/min/1.73m2 and it remained stable during the follow-up. At six months the median creatinine was 1.10mg/dL with a median eGFR 77ml/min/1.73m2. And at 12 months was 1.14mg/dL with a median estimated glomerular filtration rate (eGFR) of 74ml/min/1.73m2. None of the patients presented renal function deterioration during the study.
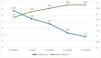
Effects on proteinuriaProteinuria followed a downwards trend during follow-up. At three months the median UPCR had decreased to 3.7g/g (2.28–8.6) from 5.75g/g (2.38–14.85) and it continued a downwards trend until 12 months of follow-up with a median of 1.7g/g (1.04–2.9). Serum albumin increased from a median of 2.7g/dL (2.5–3.63g/dL) to a median of 3.5g/dL (3.05–3.58) after three months of treatment and it remained stable at a median of 3.8g/dL. At six months, 5 (83%) of the 6 patients had achieved partial or complete remission (Table 1). By month twelve, four of the five patients who remained under follow-up were still in remission, the patient with FSGS experienced a relapse, but proteinuria and albumin were still lower than at baseline.
CD19+ B-cell depletionWe also assessed the immunological response to treatment. While on rituximab, only the patient with FGN and one of the patients with MCD had achieved CD19+ B cell depletion. Following initiation of therapy with the new anti-CD20 monoclonal antibody, CD19+ B cell depletion was observed in three patients by month one, and in all patients after three and six months.
Safety and tolerabilityNo serious adverse events were reported. Two patients developed severe hypogammaglobulinemia (<300mg/dL), two had lymphopenia (<1200×109/L), and two had mild infusion-related reactions, which resolved after reducing the infusion rate (Table 2). No infectious complications were observed during follow-up.
DiscussionIn this case series, we describe the clinical and analytical evolution of six patients with immune-mediated glomerular diseases who had been previously exposed to rituximab and were switched to second-generation anti-CD20 mABs. Our findings align with the existing reports of successful treatment of immune mediated glomerulopathies with new anti-CD20 mAbs with an adequate safety profile.9,10 While our findings are promising, they should be interpreted cautiously, as we have a small sample with a short time of follow-up.
The new anti-CD20 mABs are increasingly recognized as a safe and effective alternative in the treatment of glomerular diseases.2,10 The effectiveness of obinutuzumab for lupus nephritis has been recently published in the REGENCY trial,10 and case-series reports of successful treatment with new anti-CD20 mABs for treatment of membranous nephropathy8,9 and vasculitis11 are evermore increasing.
Rituximab resistance is increasingly recognized as a clinical challenge in the treatment of immune-mediated glomerular diseases. It has already been stated that the second generation anti-CD20 mAbs have a less immunogenic configuration structure, making them less likely elicit anti-drugs antibodies.12 Another mechanism worth considering is the activity the second-generation anti-CD20 mAbs have on B cells located in secondary lymphoid organs and tissues. While rituximab infusion is effective at peripheral B-cells depletion, in secondary lymphoid organs, such as the spleen or lymphoid nodules, persistence of B cells may occur after rituximab treatment.13 In contrast, obinutuzumab has demonstrated a greater effectiveness in reducing the B-cell population in peripheral blood and tissues.14 In our population of patients, some of them showed residual peripheral B-cell depletion after rituximab, yet clinical disease activity still persisted. These patients only achieved remission after start of treatment with obinutuzumab or ofatumumab. This observation supports the hypothesis that the new anti-CD20 mAb have a better clinical effectiveness at least in part due to their improved B-cell depletion (Fig. 1).
To summarize, in this case series of six patients with distinct immune-mediated glomerulopathies treated with novel anti-CD20 mAb, we showed that the new anti-CD20 mAbs seem to be less immunogenic1 and therefore patients might be more likely to both clinically and biologically respond as compared with rituximab.3 Furthermore, we cannot exclude the hypothesis if the better tissue penetration of these agents that could also contribute to the improved outcomes observed in our patients. Further research and clinical trials should be conducted to confirm these positive results.
CRediT authorship contribution statementML-M and MJS elaborated the original idea and study design; JIZ contributed to the development of the database; ML-M and JIZ elaborated the statistical analysis; JIZ, ML-M, and MJS wrote the manuscript; ML-M, MP, JCL, SB, IA, NR, MAA, NT contributed to the inclusion of patients in the cohort. All authors have read and agreed to the published version of the manuscript.
Patient consentThe Ethical Committee of Vall d’Hebron University Hospital approved the study protocol (AG) 252/2018). The authors declare that they have obtained consent from the patients discussed in the report.
FundingThis research was funded by ISCIIII-FEDER and ISCIII RETICS REDinREN, grant number PI21/01292, PI24/01510, ERA PerMed JTC2022 grant number AC22/00029, Río HortegaCM23/00213, Marató TV3421/C/2020, Marató TV3 215/C/2021, RICORSRD21/0005/0016, and RD24/0004/0031. Enfermedad Glomerular Compleja del Sistema Nacional de Salud (CSUR), enfermedades glomerulares complejas, PI23/01209 Proyectos de I+D+I en Salud AES2023.
Conflicts of interestM.J.S. reports personal fees from NovoNordisk, Jansen, Mundipharma, AstraZeneca, Esteve, Fresenius, Ingelheim Lilly, Vifor, ICU, Pfizer, Bayer, Travere Therapeutics, GE Healthcare, MEDICE and grants and personal fees from Boehringer Ingelheim, outside the current study.
Data availabilityData is available at a reasonable request.