To minimize our peritoneal dialysis (PD) population exposure to coronavirus disease (COVID-19), in April 2020 we developed and implemented a telemedicine program. In this investigation, we aimed to compare the hospitalization rates and metabolic disorders in patients undergoing PD 6 months before and after the COVID-19 pandemic and telemedicine implementation.
Materials and methodsThis single-center retrospective analysis included all active prevalent patients undergoing PD from April 2020. Dialysis records were reviewed to obtain clinical, demographic, laboratory, appointment, and hospitalization data. We compared hospitalization rates (total, non-PD-related, and PD-related), hospitalization-associated factors, and metabolic disorders (hemoglobin, serum potassium, and serum phosphate) 6 months before and after the pandemic.
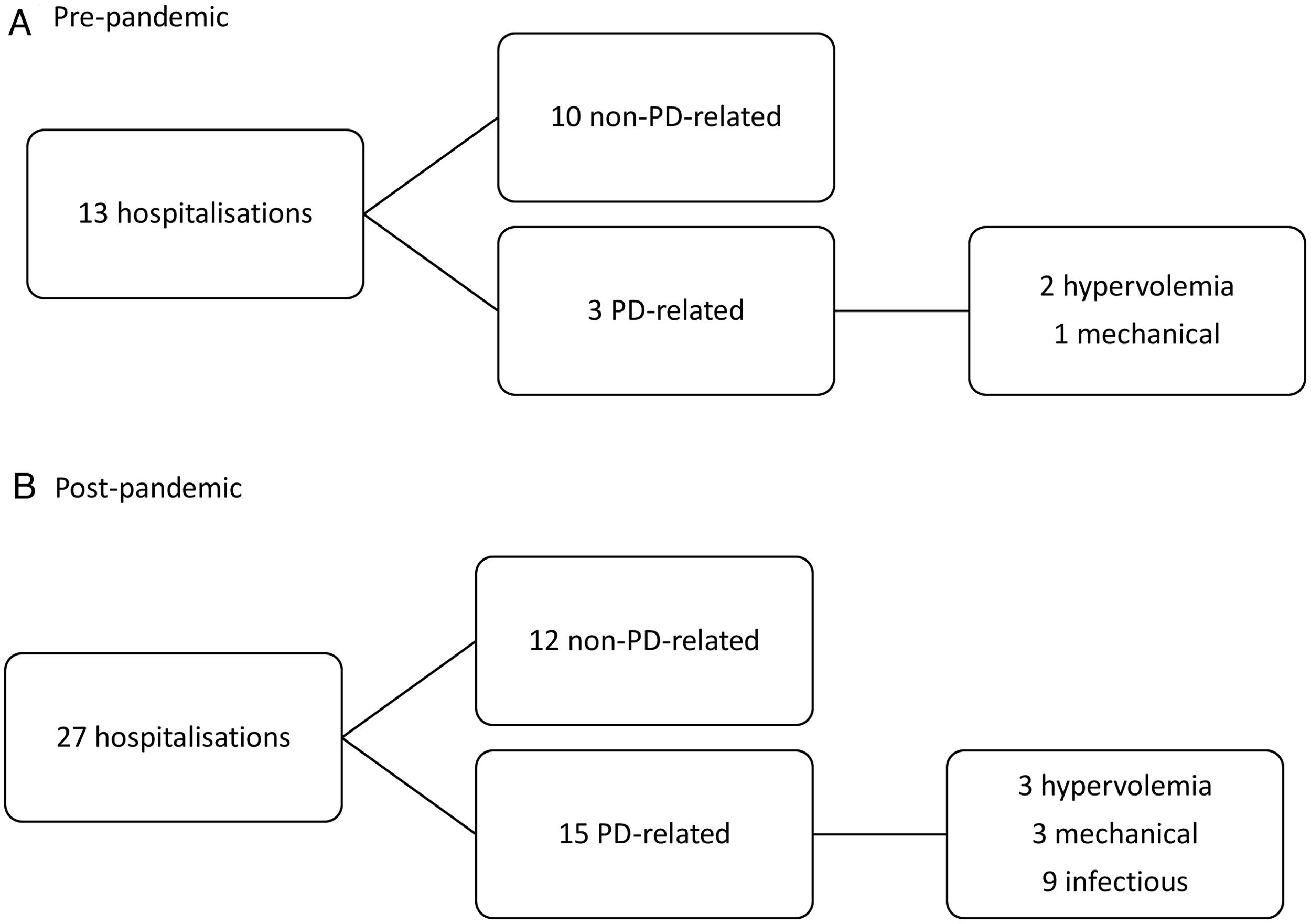
ResultsOur sample comprised 103 participants. During the pre-pandemic and post-pandemic periods, there were 13 and 27 hospital admissions, respectively. The total hospitalization incident rate ratio (IRR) was 2.48 (95% confidence interval [CI], 1.29–4.75). PD-related hospitalizations increased from 3 to 15 episodes (IRR=7.25 [95% CI, 2.11–24.78]). In the pre-pandemic period, the educational level was lower in participants hospitalised due to PD-related issues than in participants not hospitalised. In the post-pandemic period, only sex distribution differed between patients not hospitalised and those hospitalised due to non-PD-related issues. Only serum potassium levels changed significantly in the post-pandemic period (4.79±0.48 vs. 4.93±0.54mg/dL; P<0.01).
ConclusionThis study showed a significant increase in hospitalization rates after the COVID-19 pandemic period and telemedicine implementation, mainly due to PD-related infectious causes. Strategies to improve distance monitoring assistance are needed for the PD population.
Para minimizar la exposición de nuestra población de diálisis peritoneal (DP) a la enfermedad por coronavirus (COVID-19), en abril del 2020 desarrollamos e implementamos un programa de telemedicina. En esta investigación, nuestro objetivo fue comparar las tasas de hospitalización y los trastornos metabólicos en pacientes sometidos a DP 6 meses antes y después de la pandemia de COVID-19 y la implementación de la telemedicina.
Materiales y métodosEste análisis retrospectivo de un solo centro incluyó a todos los pacientes prevalentes activos sometidos a DP desde abril del 2020. Se revisaron los registros de diálisis para obtener datos clínicos, demográficos, de laboratorio, de citas y de hospitalización. Comparamos las tasas de hospitalización (total, no relacionada con la DP y relacionada con la DP), los factores asociados a la hospitalización y los trastornos metabólicos (hemoglobina, potasio sérico y fosfato sérico) 6 meses antes y después de la pandemia.
ResultadosNuestra muestra fue compuesta por 103 participantes. Durante los períodos prepandémico y pospandémico, hubo 13 y 27 ingresos hospitalarios, respectivamente. La razón de la tasa de incidentes de hospitalización (TIR) total fue de 2,48 (intervalo de confianza [IC] del 95%, 1,29-4,75). Las hospitalizaciones relacionadas con la DP aumentaron de 3 a 15 episodios (TIR=7,25 [IC del 95%, 2,11-24,78]). En el período prepandémico, el nivel educativo fue más bajo en los participantes hospitalizados debido a problemas relacionados con la DP que en los participantes no hospitalizados. En el período posterior a la pandemia, solo la distribución por sexo difirió entre los pacientes no hospitalizados y los hospitalizados debido a problemas no relacionados con la DP. Solo los niveles de potasio sérico cambiaron significativamente en el período pospandémico (4.79±0.48 frente a 4.93±0.54 mg/dL; P<0.01).
ConclusiónEste estudio mostró un aumento significativo en las tasas de hospitalización después del período pandémico de COVID-19 y la implementación de la telemedicina, principalmente debido a causas infecciosas relacionadas con la DP. Se necesitan estrategias para mejorar la asistencia de monitoreo a distancia para la población con DP.
In March 2020, the government of Santa Catarina State, southern Brazil, declared an state of emergency to prevent and combat coronavirus disease (COVID-19).1 Simultaneously, the Federal Board of Medicine authorized telemedicine for distance monitoring,2 and the International Society of Peritoneal Dialysis stated that ‘people on peritoneal dialysis (PD) should stay at home. Hospital visits should be minimized only for urgent indications. Consultations should otherwise be conducted by telemedicine’.3
Following the authorities’ recommendations to minimize the PD population's exposure to COVID-19, who are more likely to develop severe disease4 our dialysis center immediately developed and implemented a telemedicine program.5 Therefore, our healthcare team started monitoring our patients undergoing PD via telephone calls; prior to this, all patients were consulted via face-to-face appointments every month.
Before the pandemic, many PD centers worldwide had already implemented telemedicine for monitoring patients undergoing PD. Most teleconference tools have shown successful results in terms of patient satisfaction, time-saving, economic advantages, and PD outcomes.6–10 Videoconference is the preferred tool for telemedicine consultations for patients undergoing PD. In addition to allowing a closer interaction between the healthcare personnel and patients, it enables a visual inspection of the catheter exit site and effluent bag for signs of peritonitis.11 However, it demands a good quality and stable internet connection, adequate hardware and software access, and training skills for patients and workers. These requirements are challenging for low- and middle-income countries even in a non-pandemic scenario and inviable in an emergency when migration for distance monitoring needs to be fast. During the pandemic, patient's behavior in seeking healthcare assistance may also be impacted due to the fear of contamination in healthcare sites; the quality of hospital assistance may also be impacted in this troublesome period.
To evaluate the impact of the pandemic and telemedicine implementation on health outcomes, in this single-center retrospective analysis, we aimed to compare the hospitalization rates and metabolic disorders 6 months before and after the COVID-19 pandemic in patients undergoing PD.
MethodsThis retrospective study included participants from a single center located in southern Brazil. The 6-month pre-pandemic period was considered from September 2019 to February 2020 and the 6-month post-pandemic period was considered from April to September 2020.
Patients monitoringBefore the pandemic, all patients (N=117) were monitored via presential PD clinic visits by a multidisciplinary team. They had monthly appointments with nephrologists and renal nurses. Whenever necessary, they were referred to psychologists, dietitians, and social workers. As we previously described,5 in April 2020, the nursing team at our center started contacting patients every month via telephone calls before the scheduled appointment with nephrologists.
Distance monitoring was accomplished whenever they reported being clinically well, their laboratory tests within normal values, and they provided telemedicine consent. The medical team used a telephone call as a telemedicine tool because most patients were elderly and had deprived social conditions; hence, videoconference was not feasible for everyone. Telephone calls were done monthly, according to pre-scheduled date and time, by the nurse and nephrologist from a specific number linked to the dialysis unit. Calls were recorded after patients’ verbal authorization was requested at the begging of the call.
During these calls, nurses and nephrologists applied a minimum questionnaire with questions to address the main aspects of the clinical evaluation, such as bowel functioning, stool aspects, urine output, blood pressure values, weight, and glycemic control. In addition, other aspects related to the dialysis were evaluated: mean daily ultrafiltration; the presence of signs and symptoms of hypervolemia such as edema, shortness of breath, cough; catheter exit site aspect and catheter and cycler performance.
Blood samples were also collected monthly in satellite laboratory facilities to whom the requisition was sent, and patients could go directly to the closest unit to have their blood draw. Lab results were analyzed before the doctor's calls, and the modifications in treatment and medications were done during the calls. During COVID-19, no essential measurements such as KT/V, peritoneal equilibrium test and others, were post-pone to avoid the need for the patients to come to the facility and expose themselves to infection, which was recommended by the International Society of Peritoneal Dialysis (ISPD)3 and by the Brazilian Society of Nephrology.12
ParticipantsWe included adult patients who had started PD treatment at least 4 months before the isolation period (March 2020) and were active in the program in April 2020.
Data collectionDialysis records were reviewed to obtain clinical, demographic, laboratory, appointment, and hospitalization data. We considered hypervolemia, catheter mechanical issues, and technique-related infections such as peritonitis and tunnel infection as PD-related hospitalization causes. In our center, all peritonitis cases begin the treatment hospitalized, regardless of its severity and independent of germ type. After culture results, according to clinical evaluation and control cell counts patients can be discharged to complete the treatment at home. All other causes were considered non-PD related. For demographic comparisons between participants according to hospitalization status, patients with more than one hospitalization event that included a PD-related, were allocated to the PD-related hospitalization group (one patient pre-pandemic and one patient post-pandemic). For metabolic results, we calculated the mean hemoglobin, serum phosphate, and potassium levels from all available results. The percentage of participants with the mean values within the target was calculated.
Data analysisWe calculated the incidence rate (IR) for total hospitalizations and PD-related hospitalization episodes in both periods to obtain the incidence rate ratio (IRR) and 95% confidence interval (95% CI). We also calculated the total mortality IR and IRR for all patients who underwent PD and were followed up at our center during both periods.
Statistical analysis was performed using SPSS software version 21.0 for Windows (SPSS, Inc., Chicago, IL, USA). Results are expressed as mean and standard deviation or median and interquartile range according to variable distribution. For group comparisons, we used Student's t-test for variables with normal distribution or the Mann–Whitney U test for skewed variables. The chi-square test and Fisher's exact tests were used for categorical variables, and P values<0.05 were considered statistically significant.
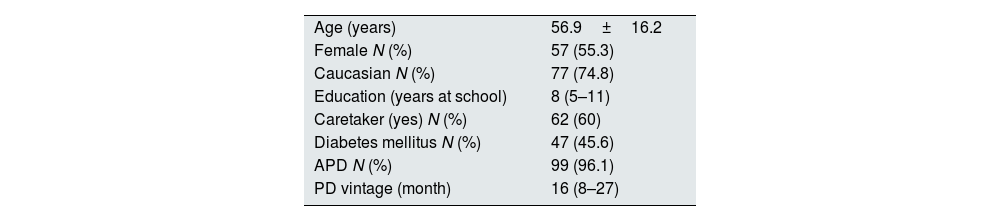
ResultsOne hundred and three patients undergoing PD were included in this analysis, and their main characteristics are presented in Table 1. Most patients were female, Caucasian, and had a caretaker. Only four patients were on continuous ambulatory peritoneal dialysis (CAPD), and almost half of the patients had diabetes.
Demographical characteristics of the participants (N=103).
| Age (years) | 56.9±16.2 |
| Female N (%) | 57 (55.3) |
| Caucasian N (%) | 77 (74.8) |
| Education (years at school) | 8 (5–11) |
| Caretaker (yes) N (%) | 62 (60) |
| Diabetes mellitus N (%) | 47 (45.6) |
| APD N (%) | 99 (96.1) |
| PD vintage (month) | 16 (8–27) |
APD: automated peritoneal dialysis; PD: peritoneal dialysis.
During the 6-month post-pandemic period, there were a total of 539 medical appointments, 444 (82%) via telemedicine and 95 (18%) face-to-face visits. All patients had at least one telemedicine appointment, and 47 (46%) did not have a face-to-face visit during the follow-up period. We did not find any statistical difference regarding the demographical characteristics of patients followed exclusively by telemedicine compared to others.
Fig. 1 shows hospitalization episodes. Before the pandemic, there were 13 hospital admissions in 12 patients (1 patient was admitted twice), resulting in an IR of 21 per 1000 patient-months. During the post-pandemic period, there were 27 admissions (4 patients were admitted due to COVID-19) in 23 patients (2 patients were admitted twice and 2 patients were admitted three times), resulting in an IR of 52 per 1000 patient-months. The IRR for total hospitalization was 2.48 (95% CI, 1.29–4.75).
The total number of PD-related hospitalizations increased from 3 (IR=4 per 1000 patient-month) to 15 (IR=29 per 1000 patient-month), representing 23% to 55% of the total hospitalizations, respectively. The IRR for PD-related hospitalization was 7.25 (95% CI, 2.11–24.78).
We also calculated the total mortality rates for all patients undergoing PD who were followed up at our center. The total mortality rate was 13.2/1000 patient-months and 17.1/1000 patient-months before and after the pandemic, resulting in an IRR of 1.29 (95% CI, 0.62–2.64). The main pre-pandemic mortality causes were: sepsis (n=5); multiple organ failure (n=2); respiratory failure (n=2); others/unknown (n=4). Post-pandemic were: COVID-19 (n=4), cardiovascular (n=3); metabolic (n=3); sepsis (n=2); others/unknown (n=3).
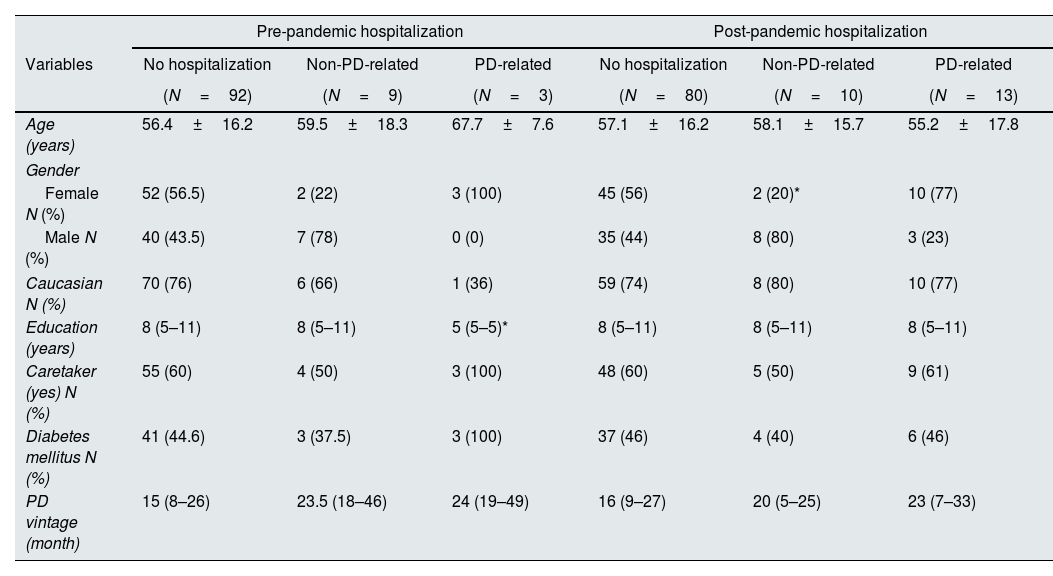
We analyzed the participants’ demographic characteristics according to hospitalization status before and after the pandemic (Table 2). Compared to patients not hospitalised, patients hospitalised due to PD-related issues had a lower education level during the pre-pandemic period. In the post-pandemic period, only sex distribution differed between patients not hospitalised and those hospitalised due non-PD-related issues.
Comparison of participants demographical characteristics according to hospitalization status before and after the pandemic (N=103).
| Pre-pandemic hospitalization | Post-pandemic hospitalization | |||||
|---|---|---|---|---|---|---|
| Variables | No hospitalization | Non-PD-related | PD-related | No hospitalization | Non-PD-related | PD-related |
| (N=92) | (N=9) | (N=3) | (N=80) | (N=10) | (N=13) | |
| Age (years) | 56.4±16.2 | 59.5±18.3 | 67.7±7.6 | 57.1±16.2 | 58.1±15.7 | 55.2±17.8 |
| Gender | ||||||
| Female N (%) | 52 (56.5) | 2 (22) | 3 (100) | 45 (56) | 2 (20)* | 10 (77) |
| Male N (%) | 40 (43.5) | 7 (78) | 0 (0) | 35 (44) | 8 (80) | 3 (23) |
| Caucasian N (%) | 70 (76) | 6 (66) | 1 (36) | 59 (74) | 8 (80) | 10 (77) |
| Education (years) | 8 (5–11) | 8 (5–11) | 5 (5–5)* | 8 (5–11) | 8 (5–11) | 8 (5–11) |
| Caretaker (yes) N (%) | 55 (60) | 4 (50) | 3 (100) | 48 (60) | 5 (50) | 9 (61) |
| Diabetes mellitus N (%) | 41 (44.6) | 3 (37.5) | 3 (100) | 37 (46) | 4 (40) | 6 (46) |
| PD vintage (month) | 15 (8–26) | 23.5 (18–46) | 24 (19–49) | 16 (9–27) | 20 (5–25) | 23 (7–33) |
PD: peritoneal dialysis.
*P<0.05.
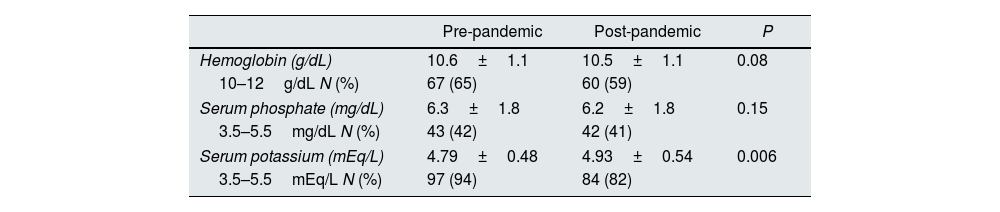
The mean laboratory results were compared between both periods. Only serum potassium levels increased significantly in the post-pandemic period compared to those in the pre-pandemic period (Table 3). The percentage of participants with mean results within the target decreased 12, 6 and 1 percentage points for serum potassium, hemoglobin, and serum respectively.
Comparison of laboratory results before and after the pandemic (N=103).
| Pre-pandemic | Post-pandemic | P | |
|---|---|---|---|
| Hemoglobin (g/dL) | 10.6±1.1 | 10.5±1.1 | 0.08 |
| 10–12g/dL N (%) | 67 (65) | 60 (59) | |
| Serum phosphate (mg/dL) | 6.3±1.8 | 6.2±1.8 | 0.15 |
| 3.5–5.5mg/dL N (%) | 43 (42) | 42 (41) | |
| Serum potassium (mEq/L) | 4.79±0.48 | 4.93±0.54 | 0.006 |
| 3.5–5.5mEq/L N (%) | 97 (94) | 84 (82) | |
In this retrospective analysis, we found a significant increase in the total hospitalization rate due to PD-related causes and a slightly higher prevalence of metabolic disorders after the start of the pandemic and telemedicine implementation.
In active patients included in our PD program, the total hospitalization rate before the pandemic more than doubled after the pandemic (IRR=2.48 [95% CI, 1.29–4.75]) and PD-related causes increased more than seven times (IRR=7.25 [95% CI, 2.11–24.78]). Among the PD-related hospitalizations, infectious causes, which were absent in the pre-pandemic period, were the most prevalent in the post-pandemic period (9 of 15 [60%], eight patients were hospitalised due to peritonitis). We raised possible causes for this finding: lack of proper training for telemedicine transition for the healthcare team and patients; difficulties in selecting patients that could benefit from face-to-face visits; the impossibility of catheter exit-site visual inspection via the telemedicine tool used (telephone call); and patients’ delay in seeking medical evaluation at the first signs of infection due to fear of exposure to COVID-19.
Our literature search found only one study that implemented a similar telemedicine protocol and reported pre- and post-pandemic results. The investigation was conducted in PD centers in the Dominican Republic and included 946 patients. Contrary to our results, the authors did not find a difference in the hospitalization or peritonitis rates during the first 3 months before and after the pandemic.13 Years before the pandemic, Gallar et al. in 2007, reported a shorter duration of hospitalization in a group of patients undergoing PD who were followed up via hybrid monitoring (face-to-face appointments or telemedicine by teleconference every other month) than in a group of patients undergoing PD who were followed up via face-to-face appointments.10
We found few significant differences in patient characteristics according to the hospitalization status. Compared to patients not hospitalised, those hospitalised for a PD-related cause had a lower educational level only in the pre-pandemic period. There was a lower prevalence of women in the non-PD-related hospitalization group than in the no hospitalization group in the post-pandemic period.
No significant differences were found in the mean hemoglobin and serum phosphate levels between the two periods; however, serum potassium levels increased in the post-pandemic period than in the pre-pandemic period, and the percentage of patients with inadequate examination results increased from 6% (before the pandemic) to 18% (after the pandemic). Hyperkalaemia was the most prevalent disturb, since only 1 patient presented hypokalaemia in both periods, however, these differences do not seem to be clinically relevant. In patients undergoing PD, risk factors for hyperkalaemia have been poorly studied and have been associated with anuria.14 Based on our clinical experience, we believe this increment might reflect a possible decrease in dialysis prescription and dietary adherence.
Our results suggest that the healthcare model implemented for distance monitoring of our patients undergoing PD was not effective in evaluating signals not complained by the patients during the consultation, which could be reflected in clinical decompensations. This might have been implicated in the observed increase in PD-related hospitalization rates during the pandemic. As previously shown, when well-managed, distance monitoring can deliver quality care for this population with some extra advantages such as time-saving and lower cost compared to the current routine6,8 In addition to routine consultations, technological solutions for remote daily monitoring of home-based automated peritoneal dialysis (APD) treatments are also available, making it feasible to detect problems early and correct inadequate dialysis delivery. Using this tool, researchers found a significant reduction in hospitalization rate and days after propensity score matching with APD group without this monitoring.15 Currently, this technology is not available for most developing countries due to cost issues.
Our study has some limitations. First, because of the observational retrospective design, no conclusions can be drawn regarding causality. In addition, the clinical context of our single-center population and the telemedicine model implemented in a pandemic scenario needs to be considered when extrapolating results to other populations. To the best of our knowledge, this is the first study to compare hospitalization rates and metabolic disorders 6 months before and after the pandemic. In addition, the outcome analysis of the same patients undergoing PD in both periods increased the power of the exposure effect.
In conclusion, in our PD population, we found a significant increase in hospitalization rates after the COVID-19 pandemic and telemedicine implementation mainly due to PD-related infectious causes. Strategies to improve telemedicine assistance with proper training and tools are needed for the PD population.
Conflict of interestAll authors declare that there is no conflict of interest.