To the Editor,
Tako-Tsubo syndrome, stress cardiopathy or transient apical ballooning, is a very rare clinical condition, and consists of a reversible acute heart failure. It is common in middle-aged women, following intense periods of psychological or physical stress.1
As described in the nineties, it consists of an acquired myocardiopathy that simulates all clinical, analytical, electrocardiographic and echocardiographic aspects of an acute, usually apical, attack.2 It is usually presented as an acute heart failure, with typical or atypical chest pain. It also presents with TS segment alterations and/or repolarisation on the electrocardiogram (ECG) and positive troponin curve. The electrocardiogram shows a severe myocardial dysfunction with a reduced ejection fraction. However, studies for detecting coronary ischaemia (stress ergometry or coronary angiography) are, by definition, negative.3
The most accepted histopathological theories discuss transient microvascular spasms caused by catecholaminergic discharge in predisposed patients. More recent studies champion a neurocardiogenic theory.4
Prognosis is almost always benign, with complete myocardial function recovery, and the relapse rate is between 2% and 10%.5
As with all acute heart disorders, Tako-Tsubo syndrome can induce acute or chronic renal failure through the classic mechanisms of secondary kidney involvement. We describe the case of a partially recovered acute kidney failure after resolving the heart disorder.
The patient is a 51-year-old female, smoker, with no relevant history of events. She came to the hospital in March 2010 with clinical symptoms of oedemas in her lower limbs that had developed over a month. She did not have dyspnoea, chest pain or any other symptoms. The emergency department found that she had renal function deterioration with 1.54mg/dl creatinine (baseline creatinine 1.1mg/dl) and microalbuminuria (95mg/day). The rest of the analyses were within the normal range and the ECG showed negative T waves for leads V5 and V6.
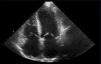
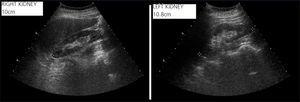
She was admitted for examination; the most noticeable result was from a transthoracic echocardiogram that revealed a severely depressed systolic function (ejection fraction of the left ventricle of 25%), with overall hypokinesia and slight hyperechogenicity of the ventricular wall (Figure 1). The other complementary tests were negative. The abdominal ultrasound found small kidneys (10cm and 11cm) with good corticomedullary differentiation (Figure 2).
Two weeks later, cardiac magnetic resonance imaging was performed showing that the ventricular function and heart contractility were normal. A subcutaneous fat biopsy was performed to verify possible amyloidosis, which was also negative. Stress ergometry performed three months later was negative for myocardial ischaemia.
In view of this, the patient was diagnosed with transient myocardial dyskinesia. Performing the ventriculography was not considered given that she had good myocardial recovery, and so as to not worsen the kidney failure. When the doctor spoke to her again, she mentioned that her family situation had been extremely stressful days before her symptoms started.
After the renal function reached a maximum creatinine level of 2mg/dl, it started to improve. It was 1.4mg/dl in the last examination performed in the nephrology department. Furthermore, ventricular function continued to be normal in later ultrasound scans.
This is a representative case of a type 1 cardiorenal syndrome (kidney involvement secondary to acute heart failure) in the context of a recently reported complex pathology, such as the Tako-Tsubo syndrome. It is a prerenal failure, in which an adequate recovery of renal function should be expected.
While there are no good early markers available for kidney dysfunction, renal function must be closely monitored for any patient with an acute heart disease for an early diagnosis. If the cardiologist and the nephrologist work together in acute management of the treatment, patient prognosis could improve.
Figure 1. Transthoracic echocardiogram
Figure 2. Kidney ultrasound