Introducción: El Plan de Calidad y Mejora en Diálisis Peritoneal (DP) de la Sociedad Española de Nefrología (S.E.N.) recomienda el uso de indicadores y estándares. Hasta el momento pocos grupos los han evaluado. Objetivo: Estudiar la evolución y cumplimiento de dichos indicadores. Métodos: Recogida prospectiva de los pacientes incidentes en DP (2003-2006) del Grupo Centro de Diálisis Peritoneal. Se recogen datos basales y semestrales de prescripción y evolución clínica, eficacia, factores de riesgo, morbimortalidad cardiovascular, anemia y abandono de técnica. Resultados: 490 pacientes (edad: 53,6 años; 61,6% hombres) con seguimiento máximo de 3 años. Causas de ERC: glomerular 25,5%, diabética 16,0%, vascular 12,4%, intersticial 13,3%. El 26,48% estaban en lista de trasplante. Eficacia de diálisis: en la primera disponible, la función renal residual era 6,37ml/min, el 67,6% de los pacientes cumplía todos los objetivos de eficacia. Sólo un 38,6% se mantiene dentro de rango todo el primer año. Anemia: el 79,3% reciben agentes eritropoyéticos y consiguen una hemoglobina (Hb) media de 12,1 g/dl. El porcentaje de pacientes en rango (Hb: 11-13 g/dl) mejora al año (58,4 frente a 56,3%), manteniéndose durante el primer año sólo un 25,6%. Riesgo cardiovascular (CV): el control óptimo tensional mejora del 36,9 al 47,4%, sólo el 15,3% permanece en rango durante todo el año. Los diabéticos presentan mayor comorbilidad cardiovascular (48,9 frente a 17,7% con eventos CV previos; p <0,001) y peor control sobre estos factores: hipertensión (40,9 frente a 17,9%; p <0,01); obesidad (22,1 frente a 16,6%; p <0,02) y dislipemia (33,7 frente a 21,8%; p <0,02). Evolución: se estiman tasas de: 1) mortalidad: 0,06 (IC 95% 0,04-0,08) muertes/paciente-año; 2) hospitalización 0,65 (0,58-0,72) ingresos/paciente-año; 3) infección peritoneal 0,50 (0,44-0,56) episodios/paciente-año. Conclusión: Disponemos de una referencia multicéntrica para los nuevos indicadores. El grado de control en HTA, anemia y eficacia mejoran al año, pero se alejan de las recomendaciones, especialmente si se valoran durante todo el seguimiento. Los diabéticos presentan mayor comorbilidad y peor control de los factores CV.
Introduction: In 2007 the Scientific Quality-technical and Improvement of Quality in Peritoneal Dialysis was edited. It includes several quality indicators. As far as we know, only some groups of work had evaluated these indicators, with inconclusive results. Aim: To study the evolution and impact of guidelines in Peritoneal Dialysis. Methods: Prospective cohort study of each incident of patients in Peritoneal Dialysis, in a regional public health care system (2003-2006). We prospectively collected baseline clinical and analytical data, technical efficacy, cardiovascular risk, events and deaths, hospital admissions and also prescription data was collected every 6 months. Results: Over a period of 3 years, 490 patients (53.58 years of age; 61.6% males.) Causes of ERC: glomerular 25.5%, diabetes 16%, vascular 12.4%, and interstitial 13.3%. 26.48% were on the list for transplant. Dialysis efficacy: Of the first available results, the residual renal function was 6.37 ml/min, achieving 67.6% of all the objectives K/DOQI. 38.6% remained within the range during the entire first year. Anaemia: 79.3% received erythropoietic sttimulating agents and maintained an average Hb of 12.1 g/dl. The percentage of patients in the range (Hb: 11-13 g/dl) improved after a year (58.4% vs 56.3% keeping in the range during this time of 25.6%). Evolution: it has been estimated that per patient-year the risk of: 1) mortality is 0.06 IC 95% [0.04-0.08]; 2) admissions 0.65 [0.58-0.72]; 3) peritoneal infections 0.5 [0.44-0.56]. Conclusion: Diabetes Mellitus patients had a higher cardiovascular risk and prevalence of events. The degrees of control during the follow-up in many topics of peritoneal dialysis improve each year; however they are far from the recommended guidelines, especially if they are evaluated throughout the whole study.
INTRODUCTION
Over the past years, the prevalence of advanced chronic kidney disease (ACKD) and kidney replacement therapy in any of its forms has increased. On a social/public health level, this involves an elevated cardiovascular (CV) morbid-mortality and uses a great amount of resources.1
This scenario compels the clinical staff and manager to insure the efficiency of resources to a maximum. One of the tools developed to this effect are the global standard guidelines, which facilitate decision-making and drafting of improvement plans, both for processes and results.2
The improvement cycle passes through four basic stages: indicator elaboration and attainment, comparison of these with references or standards, solution planning for the identified area to be improved and implementation of these actions. In summary, achievement of the best possible results is sought after as well as the reduction in inter-individual variability in the service provided.2
This is why a research group was created in 2002 for the Management of Quality in Nephrology, supported by Spanish Society of Nephrology (SEN), which has drafted several guidelines with quality indicators, mainly in the field of haemodialysis (HD).3-5
In 2007, thanks to the collaboration with a group of peritoneal dialysis (PD)6 experts, the Scientific-technical Quality and Improvement Programme in Peritoneal Dialysis was published, aimed at establishing (faced with the absence of sufficient scientific evidence to date) quality indicators and their standards in this field. Lastly, indicators and objectives are published in 2010.7
To date, only a few research groups, both national8-10 and internacional,6,11 have tried to transfer the proposed indicators to real situations in their units, basically as far as efficacy and safety of the technique, as well as control of anaemia or mineral metabolism.
The aim of our study was to analyze the characteristics of the PD incident patients, the compliance with these clinical guidelines and the subsequent evolution of these patients.
PATIENTS AND METHODS
This is a multicentre observational cohort study, with systematic consecutive sampling of the patients belonging to different departments of the hospitals in the PD regional health care system (GCDP by spanish initials) with a maximum follow-up of three years. This group is composed of 19 public hospitals in the central region of the country, serving a global health care community of 8.8 million people.
Over three years (from January 2003 to January 2006), all the patients starting PD are recorded and monitored until the end of treatment or death. On admission, demographic parameters, cause of the nephropathy, comorbidity, origin and reason for choosing this technique (free choice or by medical indication due to HD contraindication) are collected. The Charlson index was used to estimate comorbidity, previously validated for PD.12 Data regarding objectives, efficacy, residual function, peritoneal transport, anaemia treatment and blood pressure (BP) were collected at the beginning and at six months. The peritonitis, programme admissions or exits were recorded as they occurred.
Each centre uses identical databases, specifically designed for this multipurpose data collection. The databases are collected in a central office and unified every six months. A Data Manager audits and debugs the data by ranks and logical routines. Patients sign the informed consent on commencement of the therapy.
Although there are no unified treatment protocols, complying with the current guidelines objectives of efficacy, anaemia and BP control is recommended.7 According to the degree of control of BP figures, patients are classified into three subgroups: optimum control if the BP is less than 140/90mmHg, the limits are lowered to 130/80mmHg for DM patients or with prior CV event; isolated SBP when the diastolic blood pressure (DBP) is controlled and the systolic blood pressure (SBP) is greater than the limit; and poorly controlled if the DBP is greater than the limit, independent of the SBP value. Statistical management and analysis of all this data is performed with the SPSS v11.0 statistical manager. Data of numerical variables are shown as mean and standard deviation (SD). Variables without normal distribution (for example: age, Charlson index) are presented as median and range or interquartile interval. All the rates obtained (mortality, admissions and peritonitis) are referred to the technique real time for each patient. Comparisons are made using Student’s t-tests, the Student’s t-tests for paired samples, the chi-square or McNemar, according to the nature of the variables. Survival analysis test is made with Kaplan-Meier. Survival data is displayed as mean survival probability and confidence interval at 95% (CI 95%). All the incident patients are included in the analysis and the loss in follow-up reduced to 0.8%. For each survival analysis, different events are considered, considering the remaining people leaving the programme as follow-up losses. Therefore, the four analyses performed consider: death as an event for patient survival analysis; switching to HD as an event for the technique maintenance analysis; the aggregate of death and switch to HD is the event for successful analysis of the technique and, lastly, the death aggregate including change to HD, transplantation, recovery of renal function and transferral (any programme exit or loss of follow-up) allow us to estimate the technique real time. This last data can be of great interest for the design of management models or prospective follow-up studies, since it is the real time we have to care for and supervise the patient.
RESULTS
Cohort description
This analysis included 490 incident patients from 2003 to 2006 with a follow-up of 532.26 years-patient and a mean follow-up of 13.36 months (range: 0.1 to 36 months). The most relevant admission characteristics were: 53.6 years (range: 16-92), 61.6% male, Charlson comorbidity index (Ch index) 5, interquartile range (3-7), 19.1% with diabetes mellitus (DM) diagnosis and 23.7% with prior CV events. The most prevalent advanced ACKD aetiologies were: glomerulonephritis 25.5%, diabetic nephropathy 16%, ischemic vascular 12.4%, interstitial 13.3%, adult polycystic kidney disease (APKD) 10.6%. 89.9% are in PD because they decided so and the rest by medical indication. 8% come from failed transplantation and 19.7% from HD. 26.48% of the patients were included on the transplant list in the first 6 months. Table 1 gathers other cohort parameters.
Evolution
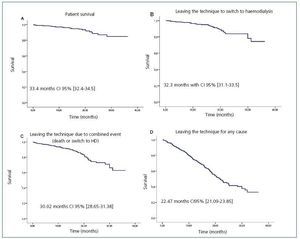
At the end of the follow-up 21.4% of the patients underwent a transplantation, 5.5% deceased, 7.4% switched to HD and 2.1% recovered renal function, the rest remained with the technique. Only 4 patients left the follow-up (0.8%).
Thirty patients deceased during the follow-up, calculating a mortality of 5.6% per year in risk and an annual mortality rate for the population of 0.056 with a CI at 95% (0.04-0.08). The most outstanding causes of death are: 46.6% CV, 20% infectious, 10% tumoral, 6.7% PD suspension, 3.3% respiratory and 3.3% hepatic-digestive.
Mean patient survival is estimated at 33.4 months with a CI at 95% (32.4-34.5); technique maintenance is estimated at 32.3 (31.1-33.5); technique success (event: death or switch to HD) is estimated at 30.02 (28.65-31.38) and PD permanence (event: any person leaving the programme or loss of follow-up) is estimated at 22.47 (21.09-23.85) (Figure 1).
Admission per patient and year in risk was 0.65 (without considering admissions for peritonitis) and an estimated annual rate within the interval at 95% (0.58-0.72). Including stays for peritonitis over 2 days, the annual admission rate is 0.79 (0.72-0.87) admissions per patient and year, i.e. one admission every 1.26 years. The mean hospital stay does not follow a normal distribution and presents an average median stay of 5.5 days and an interquartile range of (2-11).
There were 264 cases of peritonitis in 151 patients (31 patients had two episodes, 18 three and 13 over three), with a global rate in the sample of 0.5 episodes of peritonitis per year in risk and a CI at 95% of 0.44-0.56 episodes per year; i.e. one peritonitis event every two years. 41.1% of the patients with peritonitis required admission.
The mean rate of loss of residual kidney function in cases remaining at least one year on the technique was 2ml/min per year.
Cardiovascular risk
Before commencing PD, 9.15% had suffered an acute myocardial infarction, 12.68% had peripheral arteriopathy (1% with major amputation), 4.78% had acute cerebrovascular disease and 6.44% some episode of congestive heart failure (CHF). As a whole, 23.7% of the patients had suffered some prior CV event and 2.2% (n = 11) three or more.
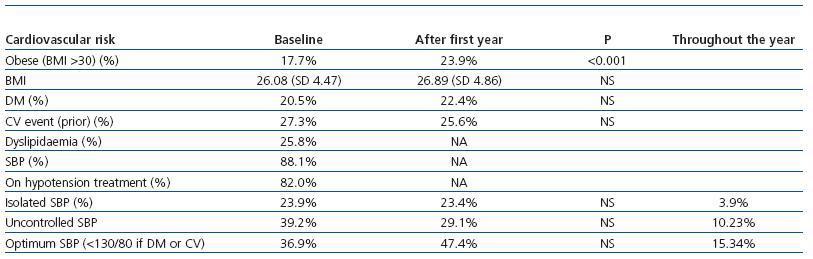
82.02% of the hypertensive patients received hypotension treatment. The baseline BP values were 132.47 (SD = 20.36) and
79.86 (SD = 12.49) mmHg. Stratified according to the degree of control, 47.2% presented optimum control, 23.1% isolatedsystolic blood pressure (SBP) and 29.7% poor control. Diabetic patients controlled their blood pressure worse than non-diabetics (each according to the optimum recommended degree of control), 28.4% versus 47.2% respectively (chi-square 10.23; value P 0.001). Data displayed in Table 1.
Patients diagnosed with DM had greater prevalence of prior CV events at the start of PD (48.9% versus 17.7%; P < 0.001). The prevalence of uncontrolled CV risk factors was greater among the DM. Therefore, greater percentages of uncontrolled SBP stand out (40.9% versus 17.9% for isolated SBP and 30.7% versus 34.9% for SBP); as well as obesity (body mass index [BMI] > 30: 22.1 versus 16.6%, P = 0.02; BMI 26.85 [SD = 4.15] versus 25.65 [SD = 4.6]; P = 0.026) and dyslipidaemia (33.69 versus 21.85%; P = 0.02). Neither age nor gender is associated to different degrees of achievement of BP control objectives.
The evolution over the first year of the control of classic CV risk factors is collected in Table 2. The annual comorbidity updates gather three new DM diagnoses and 21 new diagnoses of CV pathology in patients that did not previously have these diagnoses. The causes of admission were: 21 episodes of coronary ischemia or acute myocardial infarction (AMI), 7 cases of heart failure (CHF), 4 strokes (CVA), 8 amputations and one arrhythmia.
Efficacy and peritoneal dialysis techniques
The initial technique was CAPD with manual interchange in 65.5% of the patients, the rest used a cycling technique chosen by the nephrologist in charge. Table 1 displays the cohort descriptive data. Patient distribution by peritoneal permeability according to the baseline Twardoski PET was: 14.3%, high transport; 35.1%, mid-high; 37.3%, mid-low, and 13.3%, low transport.
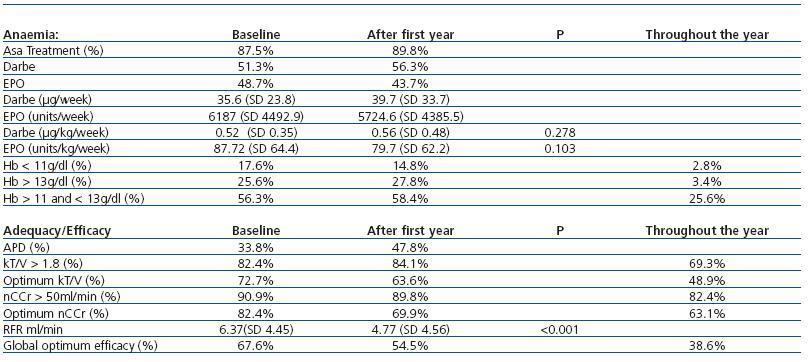
In the first efficacy measurement available a month after commencing the technique, 67.6% of the patients met all the efficacy objectives in the SEN Guidelines. Of the patients with more than one year follow-up (n = 176), only 38.6% had all their values within range during the year. Table 2 describes the distribution in techniques and efficacy data, achievement of objectives and peritoneal permeability by techniques and their evolution over the first year. For this evolutional analysis, only patients in the same type of technique during follow-up are considered.
Anaemia treatment
79.3% of the patients received treatment with erythropoietic factors (47.9% with EPO αo βand 52.1% with darbepoetin α) to reach a mean haemoglobin (Hb) of 12.1g/dl. 67% maintain Hb > 11g/dl during the entire first year of follow-up and only 25.6% between 11 and 13g/dl. The evolution of patients in the first year is displayed in Table 2.
DISCUSSION
Our study provides current and reliable estimators on meeting therapeutic objectives, admission and mortality rates in our representative incident population. This data can be useful as an initial comparison reference with the recently published Quality Objectives Guidelines. The importance of a systemised approximation with a global viewpoint to our patients’ problems is clear: knowing the results of our surroundings and comparing them with external references can help to improve these results.2 From an individual viewpoint, there are publications proving that patients who meet the greater number of therapeutic objectives have a better vital prognosis. For the time being these are only available to patients on HD, but not PD.13
The use of clinical guidelines, objectives, quality plans and indicators began in the field of HD spurred on by the eagerness to guarantee appropriate quality and uniformity in patient care. The public health system that finances dialysis treatment and the SEN have encouraged the arranged HD supply companies to develop these systems.3-5 However, the scenario for PD is another matter. With a minority presence with respect to HD (one PD patient for every eight on HD) and fairly disperse programs (less than 25 patients per centre mean prevalence in our register), we have required more time to develop these actions.7 On the other hand, we do not have sufficient contrasted evidence to establish the objectives that allow us to reduce the risk, nor the prior experience to indicate the standards for our indicators. This explains that in the guidelines published this year, more than half the indicators still have no defined standard.7
The demographic characteristics of our population (basically regarding age and DM presence is concerned) are more similar to European and Canadian studies than those from the USA.14,15 As previously discussed in other analyses of our group, the elevated prevalence of DM and the obesity in the registers from the USA make it difficult to extrapolate their results to our situation.
The hospitalisation rate was lower than registered in other series, such as the USRDS register, a likely fact in relation to lower age and comorbidity in our patients.16,17 The rate of admissions due to peritonitis is inferior to that published in other series17,18 and meets the recommendation of the quality standards.7
In comparison with other studies, such as the NECOSAD (with an 80% survival rate after 2 years), our mortality rate is lower.15 It is even lower than the national mean recorded in the register of renal patients. To explain this, we considered as possible factors the fact of including only incident patients, the not too elevated age and a lower DM prevalence. Most of the studies found less or similar mortality in PD patients than in HD patients during the first 2 years,14 a tendency that progressively evens out, especially in patients aged over 65.15 Furthermore, the chosen dialysis technique does not seem to have prognostic value, particularly when it is corrected by selection and comorbidity criteria.19 These considerations, added to the lack of quality indicators that are sufficiently validated in PD (can be compared to the HD), have not allowed the establishment of clear recommendations for one or the other technique.
Although we do not have clear and defined indicators in PD as regards validation and prediction of the cardiovascular risk, we have observed that the degree of control of conventional factors such as BP is sufficient. This is in harmony with that reported in other series in our surroundings.10
As previously published, the comorbidity at the start of the PD is the main factor of vital prognosis. We cannot discern whether the final results depend on the combined action of CV events prior to commencing the technique, age, the DM itself or the patient’s treatment during the technique process.20 In our opinion, systematic detection of CV disease in the early stages of the CKD could result more advantageous for control of CV morbid-mortality. 21
The initial attainment of dialysis efficacy objectives is not difficult in the first stages on PD, in a similar way to that referred to by other groups in our surroundings.8 However, maintenance of these after a year of follow-up decreases dramatically, together with the loss of RFR and even less patients maintain them in all the available values throughout the first year. Anyway, several randomised studies have proven that a larger dose of dialysis does not improve survival.22
Data obtained with respect to anaemia treatment are acceptable if duly evaluated (baseline and after a year), even though it is true that in only 25% Hb is maintained within the recommended target during the first year. However, this fact is better than the previous HD references. In a recently published Spanish study, less than 5% of the patients on HD were able to maintain their Hb values in the range throughout the year, although in this case monthly determinations were carried out.23 The analysis of the factors that associated a better approach to these objectives is not within the scope of this study and does not allow for adequate comparison with other records.16
The main limitations of this study are the absence of shared action protocols and the follow-up time of the patients, which is under 2 years. An early and integral approach to the advanced ACKD and the various kidney replacement techniques allow for patient mobility between PD/HD/transplantation. Therefore, one third of those commencing the follow-up do not finalise the study. In any case, it should be pointed out that the mean stay does not increase much in other studies or registers with longer track records.10,19 It is more relevant that the first cause of leaving the PD programme is transplantation and approximately one in 4 incident patients have already received a transplant in an average time of little over a year. It seems that the new model of integrated kidney replacement treatment has a preferential route in PD as the anteroom to transplant.24 The other limitation is the absence of shared protocols, however, the GCDP holds 6-monthly meetings in which the application of clinical guidelines is recommended, results are analysed and specific aspects of patient treatment are discussed. It is to be expected, that over time, this operating system will lead us to standardise our methods.
It is a relevant study both for its design as well as its sample size. It allows for identification of areas susceptible of improvement and start up corrective actions. Furthermore, faced with the absence of published nationwide data, it can aid other PD units as a reference, with the final objective for all of reducing their existing variability.8
In summary, patients that begin PD in our surroundings are younger than in HD, although they present a similar pondered Charlson index adjusted to their age. The hospitalisation, mortality and peritonitis rate was lower than that of other registers. We still have no adequate instruments for measuring CV risk in PD, and the current situation suggests that our patients are not sufficiently controlled. The degree of control in hypertension, anaemia and efficacy improves after a year, however they are far from the recommendations, especially if they are evaluated throughout the whole study.
The lack of standardisation in many of the tools proposed lately continues to limit the doctors’ efforts to reduce the variability of their clinical practice. Therefore, we are still in need of studies on the prognosis of our patients in the different kidney replaced treatment techniques.
Conflict of interest
The authors affirm that they have no conflicts of interest. This project is jointly funded by: Baxter (2003-2009), Amgen (20052009), Fresenius (2007-2009) and Gambro (2008-2009) through an agreement with the Nephrology Foundation of Madrid (Fundación Madrileña de Nefrología-SOMANE).
The authors affirm the sources of prior or subsequent sponsorship as the journal requires, but the characteristics of the article consider that there is no conflict of interest.
Table 1. Achievement of CV risk objectives, at the start, a year later and throughout the year in patients with a minimum of one year follow-up
Table 2. Achievement of anaemia and adaptation objectives at the start, after a year and throughout the year in patients with a minimum of one year follow-up
Figure 1. Kaplan-Meier estimator for patient survival (A), transferral to HD (B), leaving the technique due to combined event (death or HD) (C), and exit for any cause (death, switch to HD, transferral, recovery of kidney function or transplantation). Mean survival