Introduction: Hospitalised chronic haemodialysis patients often develop malnutrition due to many causes, which worsens throughout their hospital stay. The objective of the study is to analyse if the disorders related to hospitalisation influence the degree of malnutrition suffered during the hospital stay. Patients and Methods: Over a period of more than three months, we retrospectively chose chronic haemodialysis patients that were admitted for more than four days, excluding those cases that died in the hospital. We randomly chose one admission episode per patient so as to avoid excessive weighing of repeated admissions. We took data concerning weight changes, pre-admission and post-discharge analytical results, analytical results following first week of hospital stay, disorders causing hospital admission and those that developed during the hospital stay. We created a point score system to record the total of illnesses presented. Results: The study included 77 patients, aged 67±12 years and having undergone haemodialysis for 31±34 months. Hospital stay was 17.8±12.6 days (median, 12 days). We observed that many patients admitted for digestive and osteoarticular disorders, heart failure or coronary syndrome lost more weight during their hospital stay, although no significant differences were reached. The total number of disorders suffered during the hospital stay was independent of the cause of hospitalisation. Anaemia, heart arrhythmias and signs of heart failure were associated with longer hospital stays, however it was only anaemia that was significantly related to greater weight loss. Weight loss was not related to surgery or infections. Albumin levels during the first week of hospital stay were different depending on the disorder upon admission. It was lower when the patients were admitted for digestive disorders (ANOVA, P=.05). Changes in albumin and creatinine levels before and after the hospital stay did not differ among disorders. We observed a relationship between having presented with more disorders during the stay and a longer stay, lower initial albumin and greater weight loss following discharge. In the multivariate analysis, we found the following weight loss predictors: stay, anaemia, and sepsis. We also found the following hospital stay predictors: Charlson’s comorbidity index, heart arrhythmias, anaemia, sepsis and surgery. Conclusions: Malnutrition during the hospital stay depends on the duration and the number of disorders that develop during this time, the cause of admission having less impact on this. Albumin levels decrease earlier in patients that are going to develop more disorders during hospital stay.
Introducción: Durante la hospitalización de pacientes en hemodiálisis crónica se produce un deterioro nutricional de origen multifactorial y que guarda relación con la duración de la estancia hospitalaria. El objetivo del estudio fue analizar si las patologías relacionadas con el ingreso influyen en el grado de deterioro nutricional sufrido durante el ingreso hospitalario. Pacientes y métodos: Seleccionamos retrospectivamente ingresos hospitalarios de pacientes en hemodiálisis crónica durante más de tres meses con una estancia superior a cuatro días, excluyendo aquellos casos que fallecieron en el hospital. Se eligió aleatoriamente un solo episodio de ingreso por paciente para evitar el peso excesivo de ingresos reiterados. Se recogieron cambios de peso, analítica preingreso y postingreso, analítica en primera semana de hospitalización, patologías causantes del ingreso y las aparecidas durante éste. Se construyó una puntuación para recoger el total de enfermedades presentadas. Resultados: El estudio incluyó a 77 pacientes con 67 ± 12 años y 31 ± 34 meses en hemodiálisis. La estancia hospitalaria fue de 17,8 ± 12,6 días (mediana, 12 días). Al considerar la causa de ingreso observamos una pérdida de peso algo mayor en pacientes ingresados por patología digestiva, osteoarticular, insuficiencia cardíaca o síndrome coronario, aunque sin alcanzar diferencias significativas. El número total de patologías sufridas durante el ingreso fue independiente del motivo de ingreso. La anemización, las arritmias cardíacas y la presencia de insuficiencia cardíaca se asociaron con una mayor estancia hospitalaria, siendo sólo la anemización la que se relacionó de forma significativa con mayor pérdida de peso. No se relacionaron con la pérdida de peso la realización de cirugía o la presencia de infecciones. La albúmina en la primera semana de hospitalización fue diferente según la patología del ingreso y fue más baja cuando ingresaron por patologías digestivas (ANOVA, p = 0,05). La variación de la albúmina y creatinina antes y después de la hospitalización no fue diferente según las patologías. Observamos una relación entre haber presentado un mayor número de patologías durante el ingreso con una mayor estancia, menor albúmina inicial y mayores pérdidas de peso tras el alta. Realizando análisis multivariante encontramos como predictores de la pérdida de peso la estancia, la anemización y la presencia de sepsis. Como predictores de la estancia encontramos el índice de comorbilidad de Charlson, la presencia de arritmia cardíaca, la anemización, la sepsis y la cirugía. Conclusiones: El deterioro nutricional durante la hospitalización depende de la duración de la estancia y del número de patologías sufridas durante el ingreso, influyendo menos el motivo de hospitalización. La albúmina se reduce de forma precoz en pacientes con ingresos que van a complicarse con un mayor número de patologías.
INTRODUCTION
Patients undergoing a chronic haemodialysis programme often need to be admitted to hospital; vascular access complications, infections and cardiovascular diseases are the main causes for admission.1-5 The frequency is 1.8-2.2 admissions per patient-year, resulting in a hospital stay of 13-17 days per patient-year.3,4,6,7 Of these admissions, 26%-34.9% are for more than 8 days and 11%-17% are more than 30 days.5,8-10 Patients that are often admitted to hospital are characterised by a high-grade comorbidity, a poorly functioning vascular access, older age, worse quality of life indices2,4,6,7,11,12 and a poor appetite, which is a very vague and multifactorial characteristic that however acts as a risk marker for a higher frequency of hospital admission and mortality in several studies.13,14 Furthermore, after patients of a certain age are admitted into hospital, an overall and functional deterioration is often observed,15 especially if hospitalisation has been long or complicated. It may also be followed by readmissions for up to 24%-36% of cases, which is often related to early discharge8,9,16,17 or is followed by post-discharge death.8,18,19 Following a hospital stay, patients often have to move to a residential home or minimum care units, especially patients of a certain age, which is related to a loss of quality of life.8,17,20
When patients are admitted to hospital, a significant weight loss is often observed, which is probably a sign of progressive malnutrition.8,21,22 In a study that had already been published, body weight loss was already observed at discharge, and continued progressively for at least 4 weeks after the hospital stay.22 This weight loss was not sex- or age-dependent, but was related to the length of the hospital stay8,22 and the presence of hypoalbuminemia, which is probably a sign of inflammation during hospital stay.22 Many factors are involved in this malnutrition,22 among which is reduced kilocalorie and protein counts caused by illness-related anorexia and because patients reject hospital food.23,24 On the other hand, inflammation- and prolonged fasting-related protein catabolism also cause protein reserves to be consumed, especially those from muscles, and body fat compartment, as occurs in patients who have been in the intensive care unit (ICU) for a long period of time or in difficult post-operative recoveries.25,26
However, the impact that disorders related to hospitalisation have on the nutritional state or weight loss in patients on haemodialysis has not previously been studied. Therefore, our objective was to perform a retrospective analysis to find out whether disorders that induce hospitalisation or that have developed during the hospital stay are related to malnutrition suffered by chronic haemodialysis patients during their stay.
PATIENTS AND METHODS
The Jaen Hospital Complex is the referral hospital for 650 000 inhabitants. Between January 2004 and December 2006, there were 290 patients undergoing chronic haemodialysis in three dialysis centres: a hospital unit, a satellite centre in Jaen city centre and a private dialysis centre in Úbeda (NefroÚbeda). Haemodialysis patients that need to be admitted to hospital for more than 2 days are always referred to the Jaen Hospital Complex no matter which town the patient is from or the dialysis unit that he or she uses. They come to our hospital because it is the only one that has a hospital haemodialysis programme.
We chose a random sample of patients that had been on the chronic haemodialysis programme for more than three months, and which had been hospitalised for more than 4 days during this time period. We decided that the hospital stay had to be more than 4 days as no noticeable nutritional changes would occur in a shorter period. We recorded 370 hospital stays of more than 4 days for 225 haemodialysis patients, with 1-11 hospitalisations per patient. The average age of this population was 67±14 years old and average hospital stay was 13.8±9.3 days (5-74 days).
We included planned and emergency hospitalisations in ours or other wards, due to any type of disorder. Only one hospital admission episode was chosen for each patient to avoid overrepresentation of certain patients and to therefore prevent self-correlation. When a patient had more than one admission during the study period, the first one was chosen for the study. We excluded patients that died during their hospital stay, since we were not able to analyse their evolution after discharge. Nor did we include patients that spent more than 4 days in the intensive care unit as we understood that weight changes would be excessive and much different from normal hospital stays. We obtained a random sample of patients by listing them in alphabetical order, and grouping them in sets of three, choosing the first of each group of three. The sample therefore included 34.2% of the patients that were hospitalised during the study period.
We collected demographic parameters and the patient’s base disorder to create the Charlson’s comorbidity index without adjusting for age,6 given that by performing the multivariate analysis we also use age as a covariate and both would therefore be found to be very correlated. We also collected data on routine analyses, dialysis adjustment parameters (nPNA and Kt/V [Daugirdas second generation]) for each patient before and after hospital admission. Pre-admission analysis was taken between one and six weeks before hospital admission. Post-discharge analysis was taken at one and 2 months after the patient was discharged. We also collected data on haemoglobin/haematocrit, urea, creatinine, potassium, albumin, transferrin and ferritin levels taken from patients that had these analytical results during the first week of hospitalisation. These data could not be fully reliable if patients received some type of food supplement (intradialysis parenteral nutrition, total parenteral nutrition or food supplements, etc.), and they were not studied.
We used the post-dialysis weight as a parameter which reflects the patient’s overall nutritional situation during haemodialysis, using the following hypothesis: a patient in a stable situation should not lose weight in the short term, i.e. in a space of a few months; more or less noticeable malnutrition will be indicated sooner or later by a post-dialysis weight loss, after performing the corresponding dry-weight adjustment and removing excess water from muscular mass reduction. Heart failure causes the dry weight to remain above the actual weight, at the expense of the body’s over-hydration, which hides a previous lean weight loss. This means that to a certain extent we also consider weight loss to be a reflection of nutritional loss. We therefore collected the post-dialysis weight a week before admission, weight upon admission and upon discharge, and weight at 2 and 4 weeks after hospital discharge. We calculated the weight variations (¿W) upon discharge (¿WDisch), at 2 weeks (¿W+2wk) and 4 weeks (¿W+4wk), the weight differences at each moment and admission weight. A negative value will indicate weight loss and a positive value weight gain. We counted the total number of haemodialysis sessions and the weight loss or accumulated ultrafiltration achieved in the haemodialysis sessions performed during the patients’ hospital stay.
We collected data on the disorder that caused the patient’s hospital admission and the most important disorders or complications that developed while the patient was in the hospital. Given the vast variety of disorders that developed, we have separated the most common ones into basic groups so that they could be analysed statistically (Table 1). As such, we collected the following data from medical records: temporary/permanent catheter infections, arteriovenous fistula infection, respiratory infection, urinary infection, unexplained fever, significant anaemia (need for transfusion of at least two units of packed red blood cells), higher or lower gastrointestinal bleeding, clinically significant vomiting/diarrhoea which impedes food intake for several days, arrhythmias, heart attack, clinical signs of heart failure (with clinical signs of dyspnoea, orthopnoea, lower oedema and need to perform additional dialysis), vascular and osteoarticular disorders, performing a major intervention (excluding vascular access disorders), deep vein thrombosis, tumour and sepsis (assessed separately from the infection that caused it).
We gave each disorder present upon admission (regardless of whether it caused the admission or not) an arbitrary weighing of one, and we added them together, putting them in groups of organs. We also obtained the total number of disorders suffered by each patient while in hospital. With this information we intended to create a point score system that reflected the severity or degree of stress suffered upon admission, to analyse whether it was related to the stay and the nutritional changes that had occurred. We therefore considered a point score system, including catheter or arteriovenous fistula, respiratory, urinary, osteoarticular and superficial infections (cellulitis, infected ischaemic fingers) as well as other types of infections (endocarditis, cholecystitis, etc.), and unexplained fever episodes. The heart disorders were: arrhythmias, acute coronary syndrome (with or without heart attack), heart failure (oedemas, dyspnoea and/or pleural effusion mainly resolved with dialysis). Digestive disorders were: biliopancreatic disorders (acute pancreatitis, biliary colic), intestinal (paralytic ileus, intestinal obstruction), higher/lower gastrointestinal bleeding and enough vomiting or diarrhoea to hinder food intake for several days. We included a variety of disorders that were suffered by only a few cases in the other disorder group: anaemia, osteoarticular disorder (fracture), vascular (limb ischaemia, stroke), graft intolerance, vein thrombosis, arteriovenous fistula thrombosis and tumours. We considered independent disorders to be those that presented sepsis and that needed a surgical intervention so that it could be assessed independently as a stress factor. For the purpose of this study, we defined sepsis when accompanied by general clinical deterioration, hypotension/shock and repercussion on the functionality of other organs such as an alteration in the patient’s level of consciousness, liver or respiratory dysfunction, heart failure, etc.
The results are expressed as mean ± standard deviation and average ± standard error of the mean, depending on what was indicated in each instance. Each variable was checked to see whether it followed a normal distribution using the Kolmogorov-Smirnov test. We found that stay and ferritin were the only non-normal variables; thus, we used their logarithm when we performed the comparisons. We used the Mann-Whitney test to compare the unpaired quantitative variables. We used Pearson’s chi-square test to analyse the relationship between the qualitative variables. To analyse the correlations we used the Spearman’s rank correlation coefficient. For the multivariate analysis, we used the multiple linear regression analysis, checking the multivariate normality using the residue analysis. Dichotomous qualitative variables were coded as absent (0) or present (1) for each category for the patient analysed. We chose P<.05 for significant differences.
RESULTS
We included 77 patients in this study: 37 men (48.1%) and 40 women (51.9%), aged 67±31 years old (range, 26-84) with 31±34 months on dialysis (range, 3-184), 22 of which (28.6%) were diabetics. Hospital stay was 17.8±12.6 days (range, 5-55 days), with a median of 12 days, first quartile of 9 days and third quartile of 21 days. The uncorrected Charlson’s index for age was 3.6±1.5 with a median of 3 and range of 2-8 (quartiles 2 and 5).
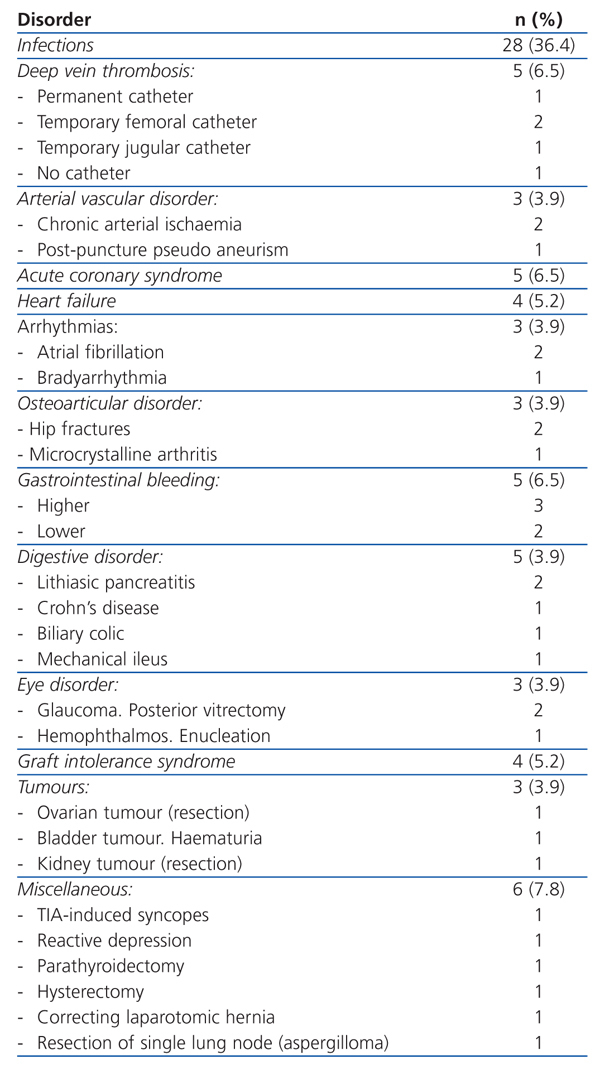
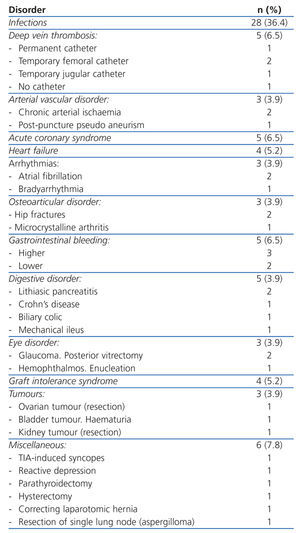
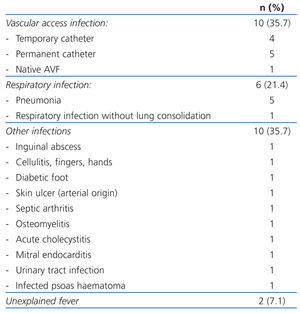
Table 1 shows the disorders that caused hospital admission and Table 2 hospital admision caused by infections. There was a large variety among the disorders and the most frequent were: temporary or permanent venous catheter infections (11.7%), followed by respiratory infections (7.8%), admissions for planned surgery (7.8%), acute coronary syndrome (6.5%), gastrointestinal bleeding (6.5%) and deep vein thrombosis (6.5%), among the most numerous.
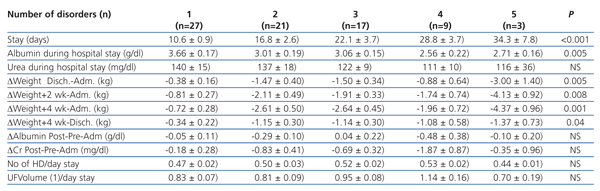
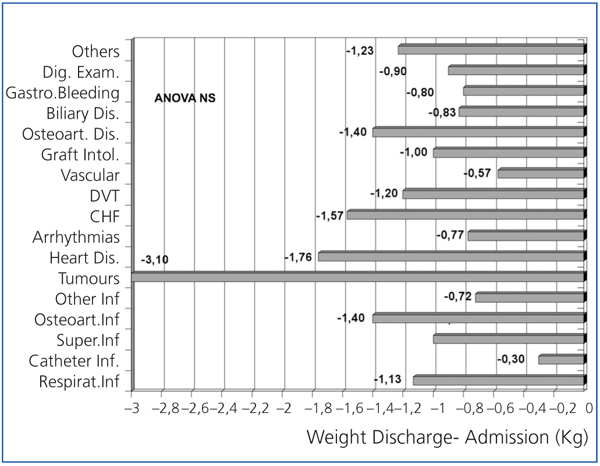
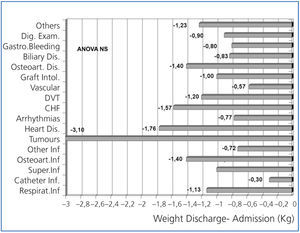
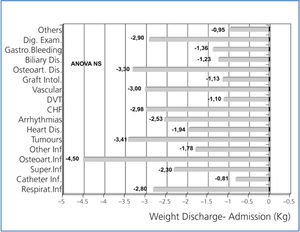
In Figures 1 and 2, weight loss is shown upon discharge and 4 weeks after hospital discharge, according to the disorder that caused the admission. Weight losses were present for almost all illnesses, and were more significant for digestive disorders, osteoarticular disorders and infections, heart failure, coronary syndrome and respiratory infections, although the reduced sample size of each group prevented us from comparing them.
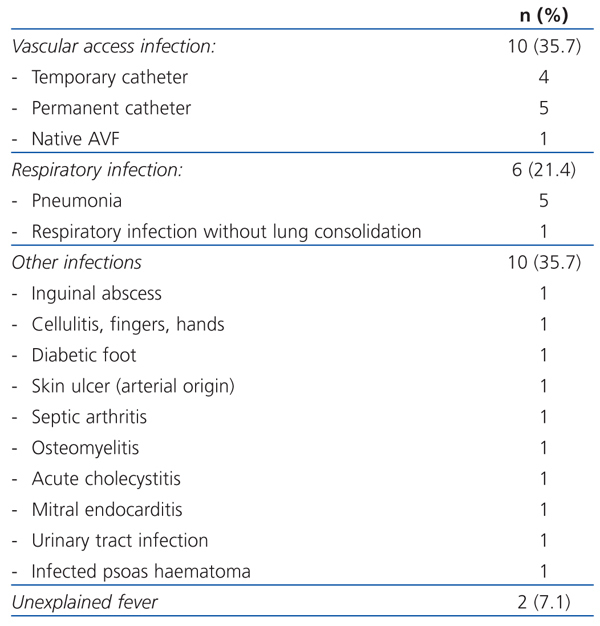
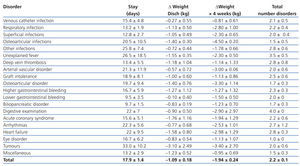
Table 3 shows the stay, weight loss suffered upon discharge and 4 weeks after discharge and the total number of disorders that developed during the hospital stay, according to the disease that caused the admission. There was a great variability in stays and weight loss, without having been able to show significant differences between the disorders that caused the admission, partly because of their reduced sample sizes. We can also observe that the total number of disorders that were suffered during the admission was similar in most cases. This indicates that the cause of admission often superposes many other conditions that contribute to making the stay longer and influence weight loss.
In a second step, we consider each illness present upon admission, deciding whether it was the cause of admission or whether it was additional, and we analysed its influence when the sample size was large enough. Temporary and permanent catheter infections are associated with a shorter stay and with less weight loss than other types of infection, although they are not significant. Eleven patients with infections presented with clinical signs of sepsis. These patients presented with less weight loss on discharge (sepsis -0.40±0.47kg versus no sepsis -1.20±0.19kg), at 2 weeks (sepsis -0.89±0.53kg versus no -1.77±0.23kg), at 4 weeks (sepsis -1.13±0.58kg versus no sepsis -2.08±0.26kg) and longer stay (sepsis 26.4±5.7 days versus no sepsis 16.4±10.8 days), although there were no significant differences.
Nineteen patients presented with anaemia and needed transfusion had a longer hospital stay (anaemia 24±3.6 days versus no anaemia 15.8±1.4 days; P=.047), lost more weight upon discharge (anaemia -2.12±0.54kg versus no anaemia -0.75±0.14kg; P=.024), at 2 weeks (yes -2.91±0.54kg versus no anaemia -1.23±0.20kg; P=.008), at 4 weeks (anaemia -3.60±0.55 versus no anaemia -1.40±0.22kg; P=.001). Gastrointestinal bleeding was not related to significant differences. Among the patients that did not have gastrointestinal bleeding, we observed that their erythropoietin dose was increased after admission (preadmission 9544±7044UI/week; post-discharge 11382±7513UI/week; P<.001).
Eleven patients presented with digestive symptoms with serious episodes of vomiting, and 12 had clinically significant diarrhoea, which caused their hospital stay to be lengthened and them to lose more weight, although we did not find any statistically significant differences. Seventeen patients underwent surgery; their weight did not change nor did they have to stay in hospital longer or shorter.
Ten patients presented with arrhythmias (mainly atrial fibrillation) causing hospital stay to be lengthened (arrhythmia 28.4±4.0 days versus no arrhythmia 16.3±1.5 days; P=.004) and greater weight loss, although differences were not statistically significant. Eighteen patients had clinical signs that were compatible with heart failure, which caused hospital stays to be longer (heart failure 24.4±3.4 days versus no heart failure 15.9±1.5 days; P=.03), greater weight loss 2 weeks after discharge (heart failure -2.11±0.44 versus no heart failure -1.50±0.25kg) and at 4 weeks (heart failure -2.67±0.46kg versus no heart failure -1.72±0.27kg), although they were not significant.
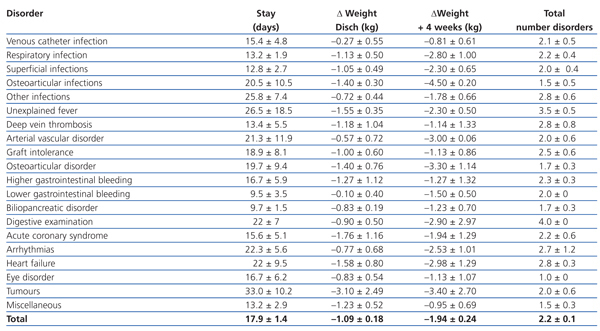
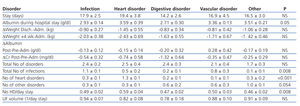
Table 4 shows how the groups of disorders were affected by hospital stay and changes in weight. Patients with heart disorders lost more weight, while we discovered that those with digestive disorders had greater drops in albumin and creatinine levels after being admitted to hospital, although these differences were not significant. However, we did find differences in albumin levels during the first week of hospitalisation (ANOVA P=.05) and patients with digestive disorders had the lowest albumin levels. The total number of disorders that developed during the hospital stay was similar among the different groups regardless of the disorder that had caused admission. The number of haemodialysis sessions/days stay was different depending on the type of disorder. Patients admitted due to a heart disorder had more sessions (ANOVA P=.008), although there were no significant differences with regards the total adjusted ultrafiltered volume for days stay.
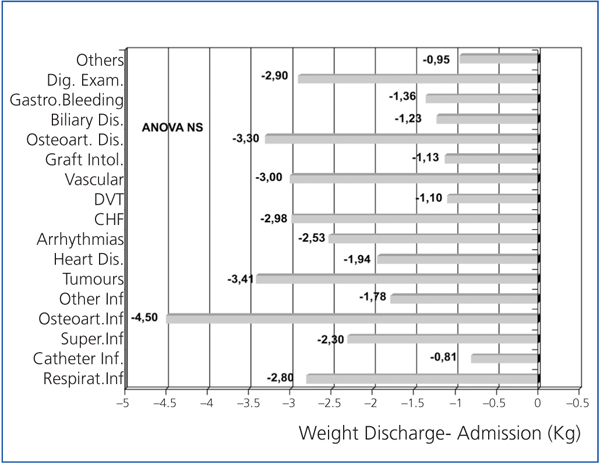
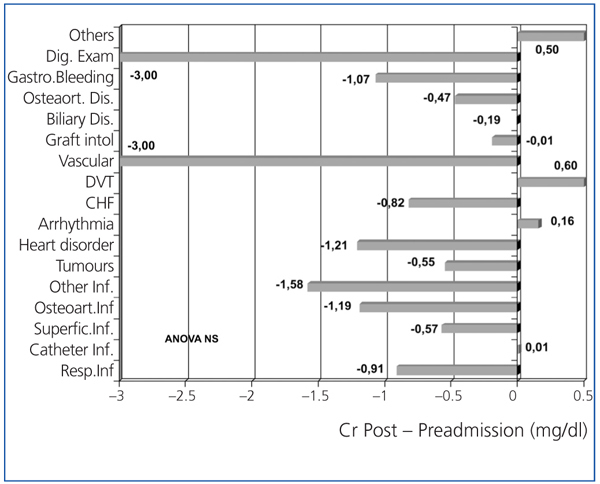
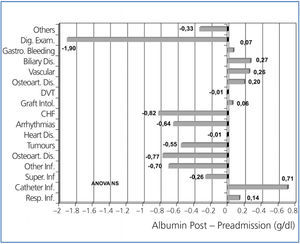
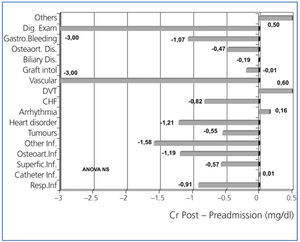
Figure 3 shows the variation of albumin comparing its levels before and after hospitalisation, according to the type of disorder that caused the patient’s hospital admission. Albumin levels were lower for digestive disorders, osteoarticular infections and various infections, heart failure and tumours. Figure 4 shows the variation observed for creatinine figures before and after hospitalisation. After being admitted to hospital, serum creatinine levels significantly decreased for patients with some disorders, such as infections, acute coronary syndrome, peripheral vascular disorder, gastrointestinal bleeding or admissions for digestive examination.
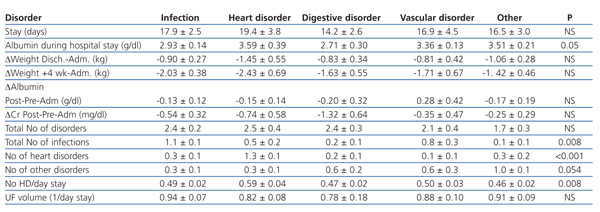
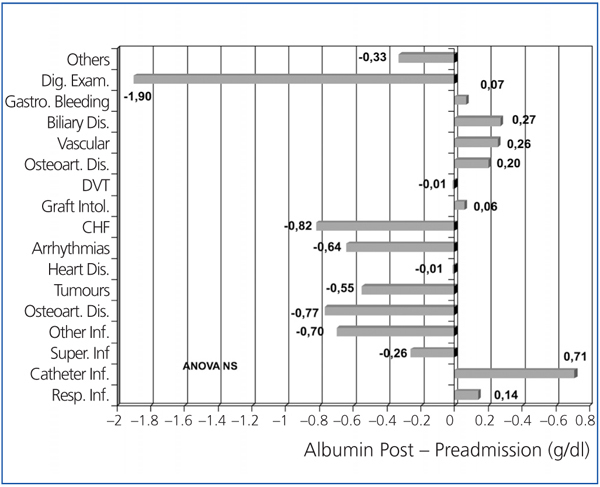
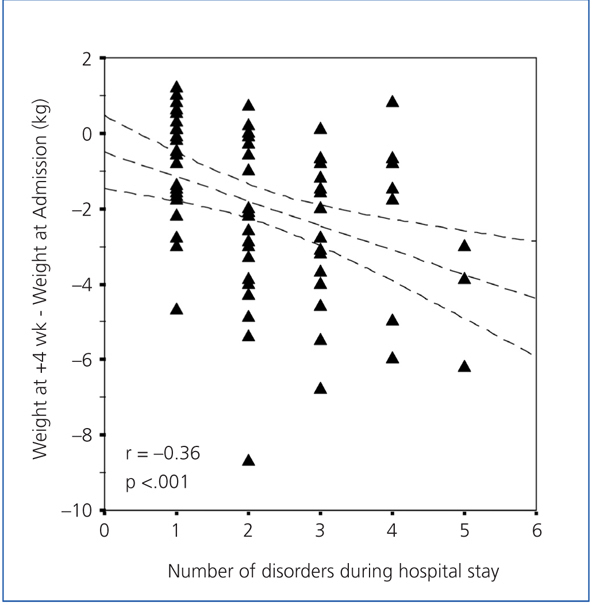
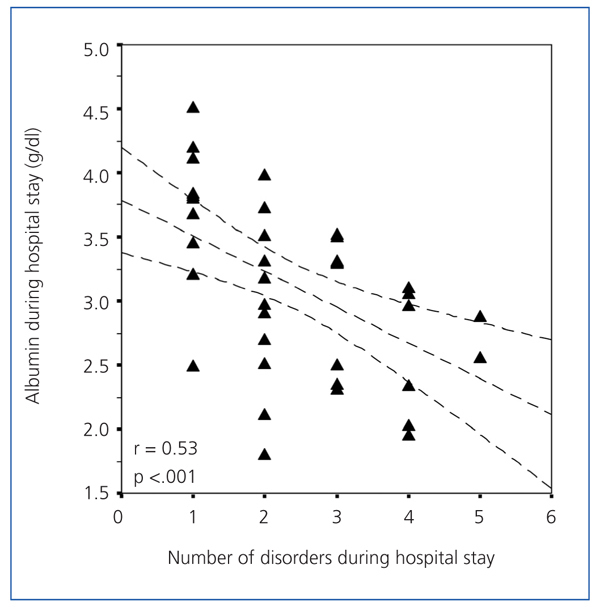
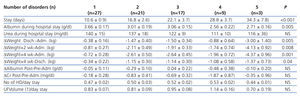
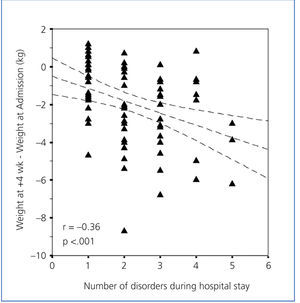
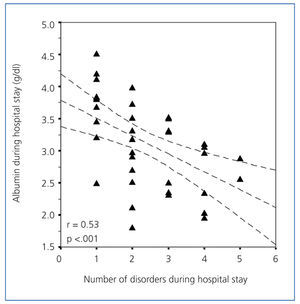
Table 5 shows how the total number of disorders during the hospital stay influenced the different variables. We observed that patients with more disorders, had longer hospital stays and lost more weight (Figure 5), and had lower albumin figures during the hospital stay (Figure 6), with significant differences. The serum urea levels during the first week of hospitalisation also decreased with the number of disorders, although this figure was not significant. We observed that patients with more disorders had a drop in the post-discharge creatinine figures, although they were not significant. We did not observe any differences on the post-discharge biochemical measurements on post-discharge protein (nPNA) or Kt/V intake.
We conducted a multivariate analysis using a linear regression analysis to find out which variables influenced weight loss during hospitalisation. Potentially predictive variables included: sex, age, months on dialysis, Charlson’s comorbidity index (without correcting for age), weight upon admission or body mass index, stay (Napierian logarithm), surgery and each of the disorders that developed during hospitalisation when there were more than 4 cases (categorised as no=0 and yes=1). For ¿W Disch.-Adm., stay, sepsis and anaemia were the influencing variables (¿W Disch.-Adm.=1.61 -0.98*Ln[Stay]-0.98*Anaemia+1.07*Sepsis; r=0.55; P<.001). For ¿W+2wk-Adm. the same variables were identified (¿W+2wk-Adm.=1.03-0.94*Ln[Stay]-1.29*Anaemia+1.12*Sepsis; r=0.51; P<.001). For ¿W+4wk-Adm. the related variables were stay, anaemia, weight upon admission, sepsis (¿W+4wk-Adm.=4.11-1.29*Ln[Stay]-0.038*Post-discharge+1.35*sepsis-1.62-Anaemia; r=0.63; P<.001).
We found the following to be stay predictors: months on haemodialysis, Charlson’s comorbidity index, heart arrhythmias, sepsis, anaemia and surgical intervention (Stay=-0.07*Months on HD+1.80*Charlson+15.5*Arrhythmia+14*Sepsis+10.7*Anaemia+6.8*Intervention; r=0.68; P<.001).
We introduced the disorder count by group in the multivariate analysis, and the variables that resulted in being stay predictors were the number of heart disorders, number of infections, number of digestive disorders, other disorders, sepsis, surgical intervention and Charlson’s comorbidity index (Stay=7.7*Heart Disorders Points+5.6*Infections Points+3.8*Digestive Points+7.4*Other Disorders Points+9.5*Sepsis+7.5*Intervention+1.8*Charlson; r=0.71; P<.001). If we were to use the total disorder count, stay predictor variables were the total number of disorders, sepsis, surgical intervention and the Charlson’s comorbidity index (Stay=5.9*Disorders points+8.6*Sepsis+8.4*Intevention+ 2.1*Charlson; r=0.69; P<.001).
By using the total number of disorders as a predictor of weight loss upon discharge, at 2 weeks and at 4 weeks, the multivariate analysis only finds stay (Napierian logarithm) and sepsis to be predictive variables (r=0.48-0.50; P<.001).
DISCUSSION
Malnutrition presented in hospitalised patients with chronic kidney disease on haemodialysis is caused by multiple factors that are reviewed in a recent study by our group.22 Nutrient intake is clearly reduced due to acute disorder-related anorexia which cause malnutrition. It is often related to the patient rejecting the food offered in the hospital, either because of the type of food, a stricter diet, or the way that the food is seasoned.23,24 Also poor tolerance to the dialysis sessions cause the patient to eat less, or not eat if the haemodialysis session is nearing. Frequent fasting periods for complementary tests or changes in the dialysis shift are added to this. Meanwhile, the disorders trigger a more or less intense inflammatory response which stimulates the protein catabolism and causes the patient to become resistant to insulin. This could cause situations that would lead to the consumption of body protein reserves and especially to the reduction of muscular compartment. This explains why weight is often lost after long hospital stays, as occurs with patients in intensive care units27 and chronic haemodialysis patients.22
In this study and the one we published recently,22 we did not want to use any definition of malnutrition, because our objective was to analyse the changes in body weight and in the analyses carried out before and after hospital admission, and discover whether there was a relationship between hospital stay and the disorder that caused hospital admission and the disorders that developed while the patient was in hospital. In the previous study we observed a weight loss that we interpreted as a result of malnutrition, in light of the analytical changes found. Unintentional weight loss is a key criterium that indicates that a patient is undergoing a process of malnutrition. For hospitalised patients it is the consequence of multiple factors among which inflammation plays a key role, which may lead to a protein-energy wasting syndrome28 if the symptoms are severe enough and the hospital stay long. In this retrospective study, we have not performed patient nutritional assessment, because we have focused on the weight changes as an overall nutritional indicator. The changes observed in serum protein levels during the hospital stay are a reflection of inflammation and do not provide nutritional information. Skinfold-based body fat and muscular circumference measurements reflect how the patient is, and are a consequence of the previous months and do not reflect how the patient progresses during the hospital stay given that a specific number of weeks would be needed for important changes to occur. Bioimpedance measurements are frequently altered and indicate excess extracellular fluid, meaning that the fat, lean body or muscular mass measurements are clearly distorted, making them less useful. In any case, the variation of the serum protein levels such as hs-CRP or prealbumin during hospitalisation will reflect how the inflammatory activity evolves, so that a gradual decrease in hs-CRP and gradual increase in prealbumin probably indicate that the intensity of the disorders has lessened and that they are prognostic markers of recovery and good progress. General improvement in these moments is likely to be accompanied by an improved appetite and probably an increase in nutrient intake. The patient’s overall assessment has shown to be useful as a marker of a greater incidence of problems during the hospital stay, which may be used to recognise important degrees of malnutrition/undernourishment and start renutrition measures. Simple questionnaires that assess previous weight loss or loss of appetite upon hospital admission can be used to recognise patients that are susceptible to suffering malnutrition. Renutrition measures can bee applied to these patients during the hospitalisation, which can shorten the hospital stay and reduce problems, although this has yet to be validated for patients undergoing haemodialysis.29
An important study limitation was that a reduced number of patients was included for each disorder group, which meant that it was difficult to perform a separate detailed analysis. However, we did obtain some interesting conclusions concerning the mechanisms that caused malnutrition in the chronic haemodialysis patients that were in hospital. In principle, we should expect patients with infectious disorders to lose more weight given that a greater inflammatory stimulus is triggered. The weight losses observed have been very varied from one infection type to another and seem to be more related to stay in each process than with infection type. Patients with vascular access infections, for example, stayed in hospital for a shorter time and did not lose as much weight as those suffering from pneumonia or respiratory infections. It could be argued that inflammation lasted longer for respiratory infections, which may explain the greater weight loss, but it is also true that once the fever symptoms lessened in these cases, recovery depended more on respiratory failure problems or additional heart failure than the infection itself. In the cases of endocarditis and osteoarticular infections, the fever process really only lasted a few days, but the stay was longer given the long-term antibiotic and locally-applied treatments, respectively, and the need for additional tests that caused the hospital stay to be longer. This has also been found by other authors.10,30 In this instance, weight loss would be due to the long hospital stay, more than the presence of a maintained or significant inflammatory stimulus, although we did not monitor patients with inflammatory markers to be able to check this hypothesis.
We have observed a relationship between low albumin levels and a longer hospital stay for hospitalised patients on chronic haemodialysis.22 Other authors found the same for patients admitted for infectious disorders.28 The lowest albumin figures are related to greater weight loss and a greater decrease in the post-discharge creatinine figures.22 In another study, our group analysed the levels of some proteins upon hospital admission and we observed that low levels of albumin, prealbumin and transferrin, and high levels of hs-CRP and alpha1-glycoprotein were correlated with a longer hospital stay, greater consumption of erythropoietic factors after admission and reduced serum creatinine levels and post-dialysis dry weight at 2 weeks and 4 weeks after discharge.31 However, the relationship between hypoalbuminaemia and these protein reductions and variables such as stay or weight loss is a lot more complex when the causal disorder or the disorders that are developed during the hospital stay are also considered. This is because they have a potential to stimulate different systemic inflammatory responses and a different ability to cause anorexia, protein loss through body fluids or ability to hinder tolerance to haemodialysis sessions. In our case, we observed lower albumin levels in patients with digestive disorders while patients with infectious disorders had fewer decreases. Patients with digestive disorders and a longer hospital stay lost more weight, but the same occurred for those with heart disorders despite them having the same serum albumin levels as patients with infections.
On the other hand, other conditions that complicate hospitalisation are added to the disorder that caused admission, and which cause the hospital stay to be longer. This can explain why a relationship is not found between the initial disorder and length of hospital stay8,10 or the probability of readmission8 (when we exclude admissions caused by vascular access problems). Each one can cause an inflammatory stimulus that helps the anorexia and protein catabolism remain high while the patient is in hospital. Some of these additional disorders could be more significant or lengthen the hospital stay more than the initial disorder, which would explain why we have not found a relationship between the admission disorders and the malnutrition. By counting the number of disorders present upon admission, we have found that patients with more disorders lost more weight, and their hospital stay was also longer. While surgical intervention did not seem to cause more weight loss in patients, we did find that significant anaemia was clearly associated with greater weight losses. This anaemia was present in gastrointestinal bleeding, but it did not cause the loss to be significant, as it was due to several disorders and a prolonged haematuria of the tumour site. Anaemia could be an indication of an erythropoietin-resistant inflammatory condition, which partly explains the post-admission anaemia that patients undergoing haemodialysis suffer.8,32,33 Furthermore, anaemia causes asthenia, which also involves a poor mental state and anorexia, which could also explain this relationship between anaemia and malnutrition.
We consider sepsis to be a sign of the severity of infectious processes. We included it in the analysis as a characteristic independent from the other disorders, observing that it was related to weight gain after hospitalisation. We did not use well-established international criteria to diagnose this condition, meaning that it could be questionable. This was because we only really considered it as part of a general condition in a situation of infection. Paradoxically, finding weight gain in these patients could be because the weight was not adjusted adequately during the hospital stay, given that they were more haemodynamically unstable and had a poor tolerance to ultrafiltration, since they continue being hyperhydrated until their general situation improves after discharge. It was weeks after discharge that their excess volume could be withdrawn.
In the multivariate analysis we have confirmed a point that we found in a previous study:22 there is a clear relationship between weight loss and hospital stay, even after adjusting for the degree of comorbidity and for disorders that developed during hospitalisation. It is difficult to separate stay and number of disorders because there is a clear relationship between the two: the more disorders presented by the patient, the longer the hospital stay. However, this is not always the case, as we have already commented, as some cases require prolonged treatment or need several complementary tests meaning that hospital stay has to be longer, without the patient necessarily being more severe. A study with more cases may be able to separate the influence of these factors more accurately and confirm that the hospital stay is a detrimental factor per se for the haemodialysis patient’s nutritional health. Many factors influence the length of haemodialysis patients’ stay, such as previous nutritional condition,34 age,2,28 whether the patient was cared for by nephrologists or internists,1 level of comorbidity6,11 and also the main disorder that caused the admission according some studies,2 although there is no relationship among others.10 Anorexia is related more often with hospitalisation and a longer hospital stay13,31 which could cause patients to eat less during their hospital stay, provoking malnutrition and more weight loss. Anorexia in hospitalised patients influences the level of inflammatory stimulus in active disorders, but also factors such as those that have already been mentioned, like the type of food offered due to the diet prescribed or the hospital’s catering. In this respect, making the diet less restrictive may be a good measure to try and alleviate the effect that low nutrient intake has on malnutrition. In a preliminary study we observed that protein and energy food supplements from the start of the admission may reduce weight loss, especially in long-stay hospital patients.35 Using intradialysis parenteral nutrition in hospitalised patients is a measure that may be taken to support poor nutrient intake when protein and energy supplements can not be administered orally due to digestive problems. However, no evidence has been published on the possible benefits for hospitalised patients.
In this study, we have used the ultrafiltration volume performed during their stay in the hospital with the intention of reflecting on the level of food intake, dietary intake or serum therapy, or to serve as a marker of the degree of malnutrition that could be produced. Malnutrition of patients undergoing haemodialysis causes the extracellular volume to expand as a result of fluid being released from the loss of muscular mass, and which accumulate given that the kidney is not functioning correctly. If we rule out the hypothesis that hypoalbuminaemia linked to the inflammation-malnutrition situation may cause the osmotic condition, the haemodialysis patients’ weight will be maintained artificially at the expense of this excess of extracellular fluid volume until it is not adjusted correctly with haemodialysis during the hospitalisation. We have not observed any relationship between the ultrafiltration volume or the need to perform more haemodialysis sessions with weight lost during the hospital stay, or any noticeable differences when considering each condition. We only found that patients with heart disorders underwent the most haemodialysis sessions, which would probably be translated as heart failure situations which would worsen ultrafiltration tolerance. Therefore, more sessions would be needed, although the same ultrafiltration volume will be achieved in the end.
In summary, patients undergoing chronic haemodialysis suffer malnutrition during hospitalisation, which depends on the hospital stay and not so much the disorder that causes the patient to be admitted. Patients that suffer more disorders during hospitalisation are those which present with worse malnutrition, caused by a longer hospital stay and everything associated with it, and/or due to the amount of disorders that occur. Significant anaemia seems to be an independent risk marker for malnutrition, as is maybe reflected in the weakness related to admission disorders or with the intensity of the inflammatory reaction caused. Treating hospitalised patients undergoing chronic haemodialysis must include a nutritional perspective and should try to detect whether patients are affected by anorexia. This will allow a sufficient dietary intake and will not make the hospital stay longer by preventing patient malnutrition, which translates to a loss of functionality and supposes a risk factor for readmission.
Table 1. Hospital admission causes for patients undergoing haemodialysis included in the study
Table 2. Infections that caused hospital admission
Table 3. Influence of cause of admission on different parameters analysed
Table 4. Main disorder that caused hospital admission and influence on different variables
Table 5. Influence in the number of disorders present during hospitalisation on length of stay, biochemical parameters, changes in weight, and number of haemodialysis sessions performed during hospitalisation
Figure 1. Variation in weight following discharge compared with weight at admission according to the main disorder that caused admission.
Figure 2. Variation of weight 4 weeks after discharge compared to weight at admission, depending on the main disorder that caused hospital admission.
Figure 3. Variation of serum albumin levels after hospital admission compared with levels before admission, considering the disorder that caused the admission
Figure 4. Variation of the serum creatinine (Cr) levels after hospital admission compared with levels before admission, considering the disorder that caused the admission
Figure 5. Variation of weight 4 weeks after discharge compared with admission, depending on the total number of disorders developed during the hospital stay.
Figure 6. Serum albumin levels during the first week of hospitalisation and number of disorders that developed during the hospital stay