Preeclampsia (PE) is a major cause of fetal morbidity and mortality. In the Western World, PE affects 2–7% of pregnancies and is responsible for 50,000 deaths annually. Early detection is a priority as it can change the clinical course, but there are no biomarkers or instrumental methods with high sensitivity and specificity. Only the hyperbaric index has a sensitivity and specificity of 99% for early identification of pregnant women at risk of developing PE, but its use is not widespread.
ObjectiveTo assess the usefulness of the hyperbaric index in the primary prevention of hypertensive pregnancy complications in a public healthcare area.
Material and methodsThis is a retrospective study of pregnancies that occurred in our area during the period 2007–2012 (N=11,784). The diagnosis was established by the hyperbaric index and pregnant women at risk were treated with ASA at night.
ResultsIn pregnant patients referred to the nephrology clinic (38.2%), diagnosed as high-risk for PE, and treated with 100mg ASA/night (from week 17), the incidence of PE episodes was reduced by 96.94%.
Introducción La preeclampsia (PE) es una importante causa de morbimortalidad fetal, que en el mundo occidental afecta al 2–7% de los embarazos y es responsable de 50.000 muertes anuales. La detección precoz es prioritaria, ya que puede cambiar su curso clínico, pero no se dispone de biomarcadores ni métodos instrumentales de alta sensibilidad y especificidad, solamente el índice hiperbárico tiene una sensibilidad y una especificidad del 99% para la identificación precoz de las gestantes en riesgo de desarrollo de PE, pero está escasamente difundido.
ObjetivoValorar la utilidad del índice hiperbárico en la prevención primaria de las complicaciones hipertensivas del embarazo en un área sanitaria.
Material y métodosEstudio retrospectivo realizado entre los embarazos habidos en nuestra área durante el periodo 2007–2012 (N=11.784). El diagnóstico se estableció mediante el índice hiperbárico y las gestantes en riesgo fueron tratadas con AAS nocturno.
ResultadosEn las gestantes remitidas a consulta de Nefrología (38,2%), diagnosticadas de alto riesgo de PE y tratadas con AAS 100mg nocturno (desde la semana 17) se redujo la incidencia de episodios de PE un 96,94%.
High blood pressure (HTN) is the most common clinical complication during pregnancy, and preeclampsia (PE) is a major cause of fetal morbi-mortality (low-birth weight or premature birth), and maternal complications including acute renal failure, HELLP syndrome, liver failure and even brain edema, seizures and death.1 In the Western world, PE affects a 2–7% of all pregnancies, and the basic pathogenic phenomenon is endothelial dysfunction caused by an imbalance of angiogenic factors producing placental abnormalities with ischemia. Endothelial dysfunction is not a limited process that is resolved at birth, but may persist and pose a future cardiovascular risk.2
Therefore, even though PE should be diagnosed early, angiogenic factors are not sensitive or specific enough to be used in clinical practice3,4; neither is hyperuricemia, although it is often correlated with the degree of severity early initiation of PE; according to two recent systematic reviews, evidence supporting a correlation between hyperuricemia and PE is limited.5 In addition, these reviews have shown that uric acid is a poor predictor of maternal-fetal complications.6 In our experience, based on the use of the hyperbaric index (HBI) as the gold standard, risk factors including primiparous pregnancies in advance age, use of oral contraceptive drugs, or a family history of HTN are predictive of PE.7
For instrumental methods, experts do not recommend the use of the uterine artery Doppler8; however, the HBI or the area of blood pressure (BP) excess above the upper limit of the tolerance range has a 99% sensitivity and specificity for the early screening of pregnant patients at risk of PE9; only the identification serpina1 by the proteomic profiling of urine10 or the evidence of podocyturia have a 100% sensitivity and specificity.11 Once the risk is detected, PE is significantly reduced by the early administration of ASA12 and vitamin D13 at night.
Therefore, the diagnosis is made with an HBI greater than 12, in addition to conventional risk factors, and prevention includes a high-dose of ASA, 100–300mg at night, resulting in a significantly reduced risk of hypertensive complications resulting from pregnancy before week 17.
The objective of the present work is to assess the use of the HBI for the primary prevention of PE in our health sector.
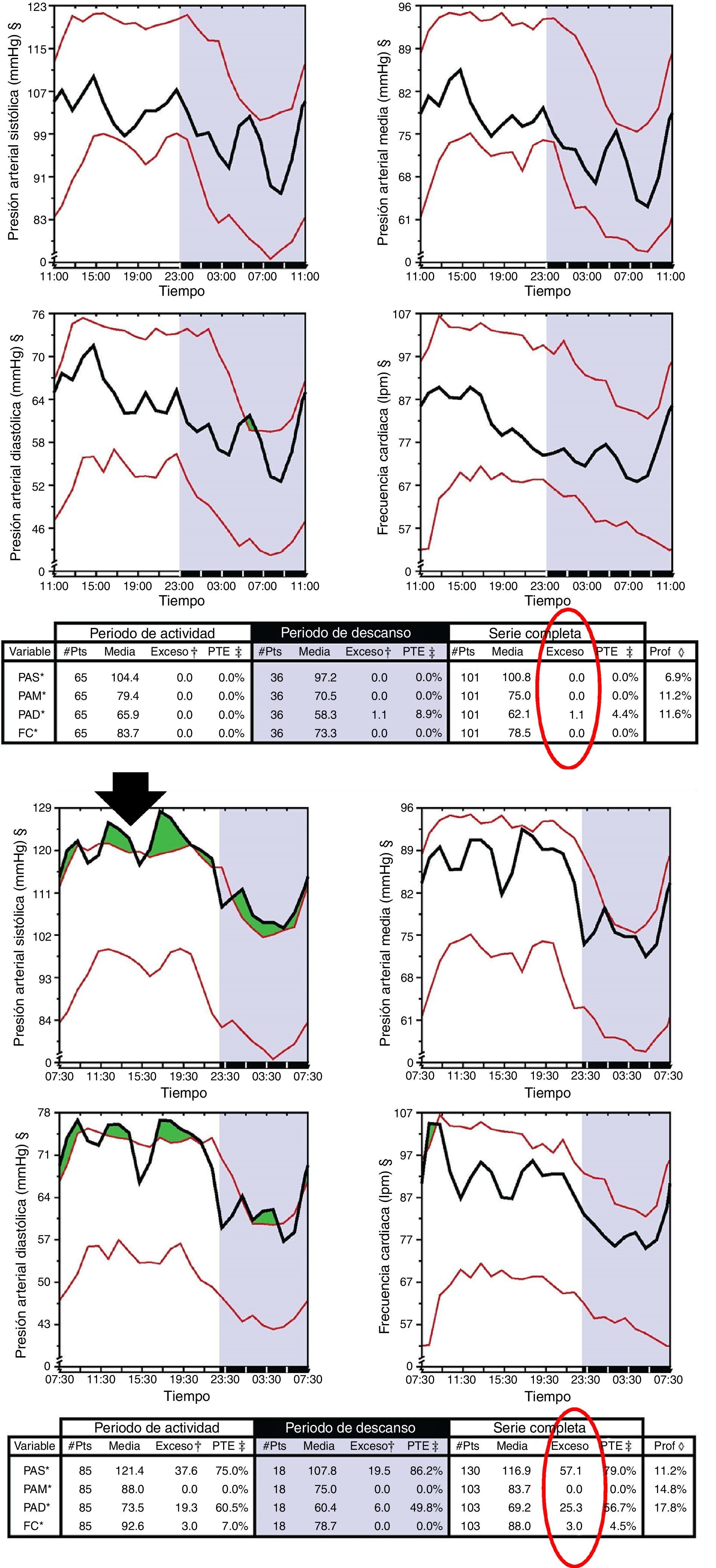
Materials and methodsThis was a retrospective study in pregnant women followed in our area between 2007 and 2012 (N=11,784). We reviewed the incidence of PE in pregnant women with high risk (HR) consultations and consultations “without HR” from three local hospitals (University Hospital Complex of Ourense [Complejo Hospitalario Universitario de Ourense, CHUOU]), the regional hospital ([Hospital Comarcal, HC] of Verín and Valdeorras) and in HR pregnant women referred to Nephrology Consultation (NC) services. In pregnant women referred to NC (before the 17th week of pregnancy), BP was monitored for 48hs as an outpatients using Spacelab 92007. An HBI of greater than 12 was considered a marker of PE risk (Fig. 1), and pregnant women with a pathologic HBI were treated with 100mg of AAS and vitamin D supplements at night provided that they had vitamin D deficiency. These pregnant women were monitored throughout pregnancy in the nephrology outpatient clinics.
HR pregnant women were defined as women who met any of the following criteria: elderly pregnant woman, morbid obesity, previous history of PE, diabetes mellitus, HTN, systemic disease (DLE, antiphospholipid syndrome), cardiopathy, family history of cardiovascular disease, smoking, twin pregnancy, or use of oral contraceptives.
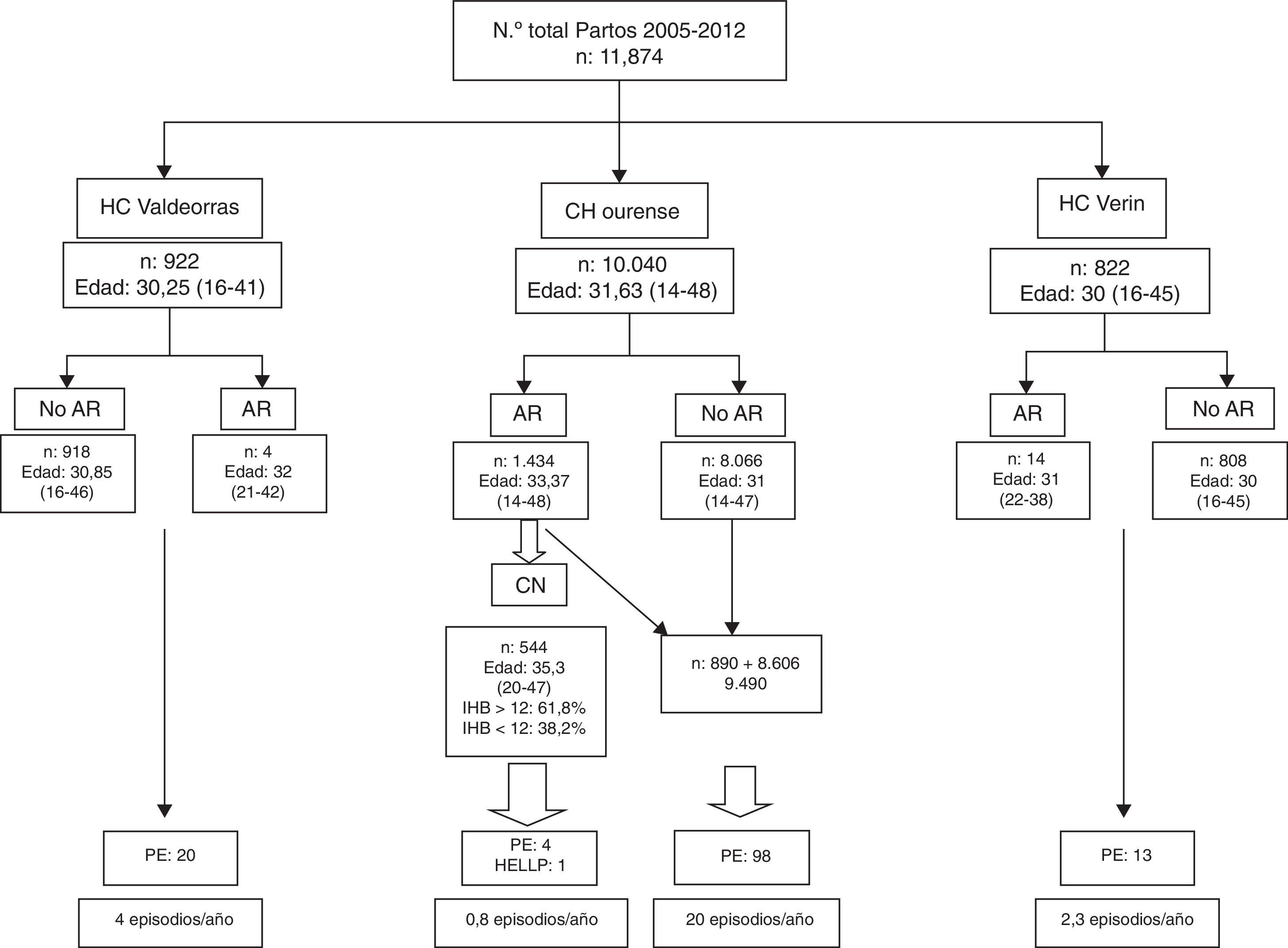
ResultsThe total number of deliveries between 2005 and 2012 was 11,784 (Fig. 2), of which 85.20% took place in the CHUOU, 7.82% in the HC of Valdeorras, and 6.91% in the HC of Verín, and the mean age of these pregnant women attended in these different centers ranged from 30 to 31.63 years old (Fig. 2). Referral from Obstetrics to HR clinics in regional centers was exceptional: 0.4% in the HC of Valdeorras and 1.70% in the HC of Verín, whereas in the CHUOU, the percent of referrals was of 14.28%. Only 34.93% of these pregnant women were referred to NC, 61.8% of them had a HBI greater than 12, while 32.8% of them showed a normal HBI.
The incidence of PE was 4episodes/year in the HC of Valdeorras and 2.3episodes/year in the HC of Verín. In the CHUOU, the incidence of PE among pregnant women who were not referred to NC was 20episodes/year, whereas 0.8episodes/year were reported among patients attending NCs including four pregnant women, two of whom had DLE, the third had intolerance to ASA, and the fourth had HELLP syndrome.
DiscussionPE is a syndrome characterized by HTN and proteinuria after the 20th week of pregnancy in women with no previous history of HTN or proteinuria. In the Western world it affects between 2% and 7% of all pregnancies, although it may threefold greater in other geographical regions.14 Mortality is 10–15%, with nearly 50,000 deaths every year. Therefore, early detection is crucial and may alter its clinical course.
The basic mechanism is a defect in placental implantation. In a normal pregnancy the cytotrophoblast overregulates metalloproteinase expression causing the conversion of epithelium to endothelium, a process mediated by the vascular endothelium growth factor (VEGF), the placental growth factor (PIGF), and angiopoietin.
In PE, there is an increase in placental and serum levels of the antiangiogenic circulating factor, sFlt-1, which binds to PIGF and VEGF and inhibits the interaction with its endothelial receptors (FIt1); as a result, NOSe is also activated, resulting in oxidative stress and placental ischemia. In PE, these factors are elevated levels at weeks 9 and 11, together with a concurrent decrease in PGF before the onset of PE.15
In addition to angiopoietin,16 other factors involved in the development of PE are low oxygen rates, resistance to insulin,17 and vitamin D deficiency. VEGF is regulated by vitamin D,18 and vitamin D deficiency-insufficiency in PE women leads to endothelial dysfunction and HTN. Finally, among other problems, placental abnormalities in the mother give rise to increased peripheral resistances due to the activity of AT1 agonistic antibodies19 and increased endoglin levels, a co-receptor of TGF B1 and TGF B3, which acts as a potent anti-angiogenic protein, “kidnapping” PGF and VEGF.
Paradoxically, none of these factors have the sensitivity-specificity and availability required for clinical use3 in the early diagnosis of PE, neither are conventional vascular risk factors5,6 or instrumental methods,8 except for BP. In early pregnancy, BP was classically considered to be useful for PE screening, and although accuracy was higher when mean BP was above 90mmHg, its predictive value was low.20 These poor outcomes of the static measurement of BP resulted from the use of the threshold for the definition of essential HTN. The pattern of BP in women with PE or HTN is known to be different and predictable; this way, differences in BP between a normotensive pregnant woman and a pregnant woman with complications (PE or gestational HTN) are detected from the first trimester with significant differences in the circadian MESOR of systolic (12mmHg) and diastolic (7mmHg) BP. As a result, the “quantification” of the “excess” in the threshold of BP or HBI, with a 99% sensitivity-specificity, allows for the screening of pregnant women at risk of PE.9
In our series, HBI was pathological in 61.9% of pregnant women referred from HR visits, but it was normal in 38.2%, thereby showing that HBI allows for a more accurate differentiation than conventional AR criteria.9 Pregnant women at high risk of PE were identified “early”, and treatment decreased its incidence from 26.3 to 0.8episodes/year, mainly in the CHUOU, which accounts for the 34% of HR pregnant women we received. No HR pregnant women came from the 2 HC, and the rate of PE remained similar to that of areas where primary care is not available.14 Protocols are common and this situation may have resulted from “clinical inertia”.
Activated platelets and coagulation system, leading to an imbalance between the synthesis of prostacyclins and thromboxane A2, result from the ischemic placental damage in PE. Therefore, several studies to assess the use of antiaggregants in the primary prevention of PE were conducted, but the initial results were discouraging,21–23 although a review report24 reveals how the risk of PE is reduced by 17% by the use of antiplatelets. All these studies have a methodologic problem: the dose of ASA and the dosing schedule. Several studies have shown that 100–150mg/dl of ASA is effective compared to lower dosing (50–80mg/dl)25 and that it should be administered before week 17 and at night,12 considering that inhibition of the thromboxane A2 synthesis by ASA is dose-dependent and that the dose is administered at night. Consequently, all pregnant women referred to NC (34.92%) and with a HBI greater than 12 (61.8%) (Fig. 2) were treated with 100mg of ASA at night during the entire pregnancy, and the incidence of PE episodes was decreased 96.94%.
In conclusion, the use of NC for the primary prevention of HTN complications during pregnancy and the use of the HBI as a diagnostic method is highly effective, and this is why routine healthcare exams should be conducted between HR consultations and Nephrology consultations during pregnancy.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: González AO, Moya SU, Arenas Moncaleano IG, Borrajo Prol MP, García García MJ, López Sánchez L. Índice hiperbárico en la prevención primaria de las complicaciones hipertensivas del embarazo de alto riesgo. Nefrologia. 2015;35:572–577.