To the Editor:
Sodium retention is an expected situation in patients with proteinuria and hypoalbuminaemia. Though the conventionally proposed mechanism is based on the low plasma oncotic pressure produced by hypoalbuminaemia, a pathophysiological explanation that proposes a primary renal retention of sodium has recently been accepted.1,2 This mechanism is independent of aldosterone. We present a case of membranous nephropathy with hyporeninaemic hypoaldosteronism.
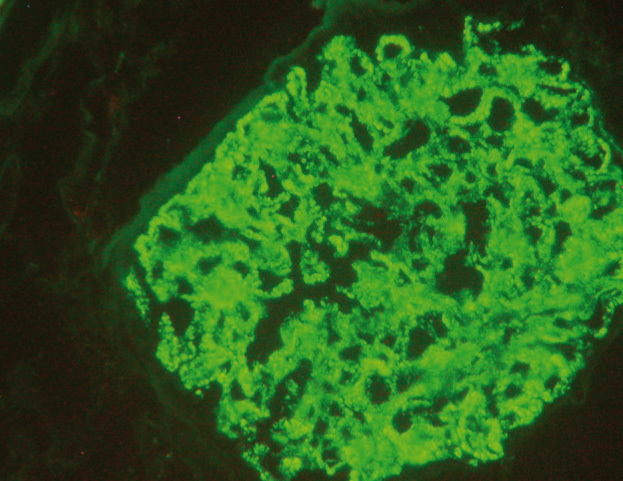
A 43-year-old male was referred to our clinic with three grams of proteinuria a day. His history included common variable immunodeficiency that had required immunoglobulin infusion years before and idiopathic thrombocytopenic purpura untreated at present. The physical examination at the time of the consultation revealed blood pressure of 125/78mmHg, with a heart rate of 70 beats per minute and minimal oedema. The blood test showed the following parameters: haemoglobin 14.2g/dl, platelets 182,000 per µl, sodium 143mEq/l, potassium 4.2mEq/l, bicarbonate 25.2mEq/L, creatinine 0.73 mg/dl, urea 27mg/dl, albumin 3.4g/dl, total protein 6.0g/dl, cholesterol 247mg/dl, glycosylated haemoglobin 4.4%. The following values were found in urine: albuminuria 2868mg/day (albumin/creatinine 1017mg/g) sodium 228mmol/day and potassium 48 mmol/l. In the immunological study, anti-neutrophil cytoplasmic, anti-glomerular basement membrane, anti-double-stranded DNA and anti-nuclear antibodies were negative. Immunoglobulin and complement levels were also in the normal range. At that time it was decided to perform a renal biopsy, which revealed membranous nephropathy (Figure 1).
The patient was initially treated with renin-angiotensin-aldosterone system inhibitors, with proteinuria decreasing to 500mg per day. However, this treatment had to be discontinued due to hyperkalaemia. The transtubular potassium gradient was 4.71 and the suprarenal study confirmed hyporeninaemic hypoaldosteronism (aldosterone <1.6ng/l, plasma renin activity 0.1ng/ml/h), with a Synacthen test that stimulated cortisol and normal sex hormones.
We consider that this case offers new pathways for understanding the role of aldosterone in patients with proteinuria. There are currently two hypotheses that try to explain sodium and water retention in nephrotic syndrome: underfill and overfill. In the first of these, the mechanism is based on low oncotic pressure produced by hypoalbuminaemia accompanying the nephrotic syndrome.1 As a result, there is renin and aldosterone stimulation, generating water and sodium retention. However, there is some controversy over this theory as the only cause of volume overload; as such, it has been proven that albumin administration in these patients does not produce an increase in natriuresis and that proteinuria per se does increase urine sodium excretion independently of plasma albumin.3,4 Recently, a new hypothesis regarding primary sodium retention by the kidney has been developed and, as such, Svenningsen et al. have suggested that proteinuria includes the filtration of proteolytic enzymes capable of directly activating the collecting duct of the epithelial sodium channel, allowing sodium retention and thus inhibiting aldosterone.2,5 Furthermore, in the nephrotic syndrome there is increased activity of phosphodiesterase in the collecting duct, allowing atrial natriuretic peptide and urodilatin degradation. The experimental administration of phosphodiesterase inhibitors reversed this positive sodium balance situation. This situation has also been demonstrated in patients with renal failure and cirrhosis.6,7 Filtered proteolytic enzymes in patients with proteinuria include plasmin, which in normal conditions is not found in the urine. However, the conversion of plasminogen to plasmin by urokinase in these patients produces a direct action on the sodium channel gamma subunit in the collecting duct, whose mission is to inhibit said channel (and therefore mass sodium reabsorption). This causes primary sodium retention independent of aldosterone (which in these cases would be inhibited).8
Very few cases have been published on this situation.9,10 The longest series includes 23 non-diabetic patients with nephrotic syndrome. Five of them had low levels of renin and aldosterone. Moreover, as in our case, these five patients had membranous nephropathy.4 In the latest case published, Hommos et al. warn about the importance of the neurohumoral system for producing sodium retention in nephrotic states. According to the authors, it is necessary that the sympathetic nervous system is intact in order to permit intratubular reabsorption of sodium.
Although in our case the renin-angiotensin-aldosterone system is inhibited, starting blockers of this system reduced proteinuria to less than half a gram per day.
We did not find any relationship in literature between variable common immunodeficiency and idiopathic thrombocytopenic purpura.
Therefore, patients with proteinuria could alternate between states of hypo and hyperaldosteronism as mechanisms responsible for sodium retention by the kidney. Nevertheless, longer series are necessary as well as a more extensive follow-up period and serial measurements of aldosterone, natriuresis and proteinuria to explain what factors determine a patient being at one extreme or the other of the same clinical profile with different and alternative pathogenic pathways.
In conclusion, we can say that in the differential diagnosis of hyperkalaemia in the nephrotic syndrome we must exclude the uncommon presence of hyporeninaemic hypoaldosteronism.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Figure 1. Renal biopsy