To the Editor:
Echinococcosis is an endemic zoonosis caused by the Echinococcus tapeworm, in which human beings participate by ingesting eggs excreted in dog faeces or other hosts.1 Uncommonly, it may occur with cysts located in the pelvis.2
We report the case of a 73-year-old male, who at the age of 33 had an operation due to a right pulmonary hydatid cyst which was complicated with a severe anaphylactic reaction after cyst rupture. He was referred with impaired renal function with creatinine (Cr) 3mg/dl. The patient complained of prostate symptoms with pollakiuria and nocturia with abdominal palpation consistent with large distended bladder.
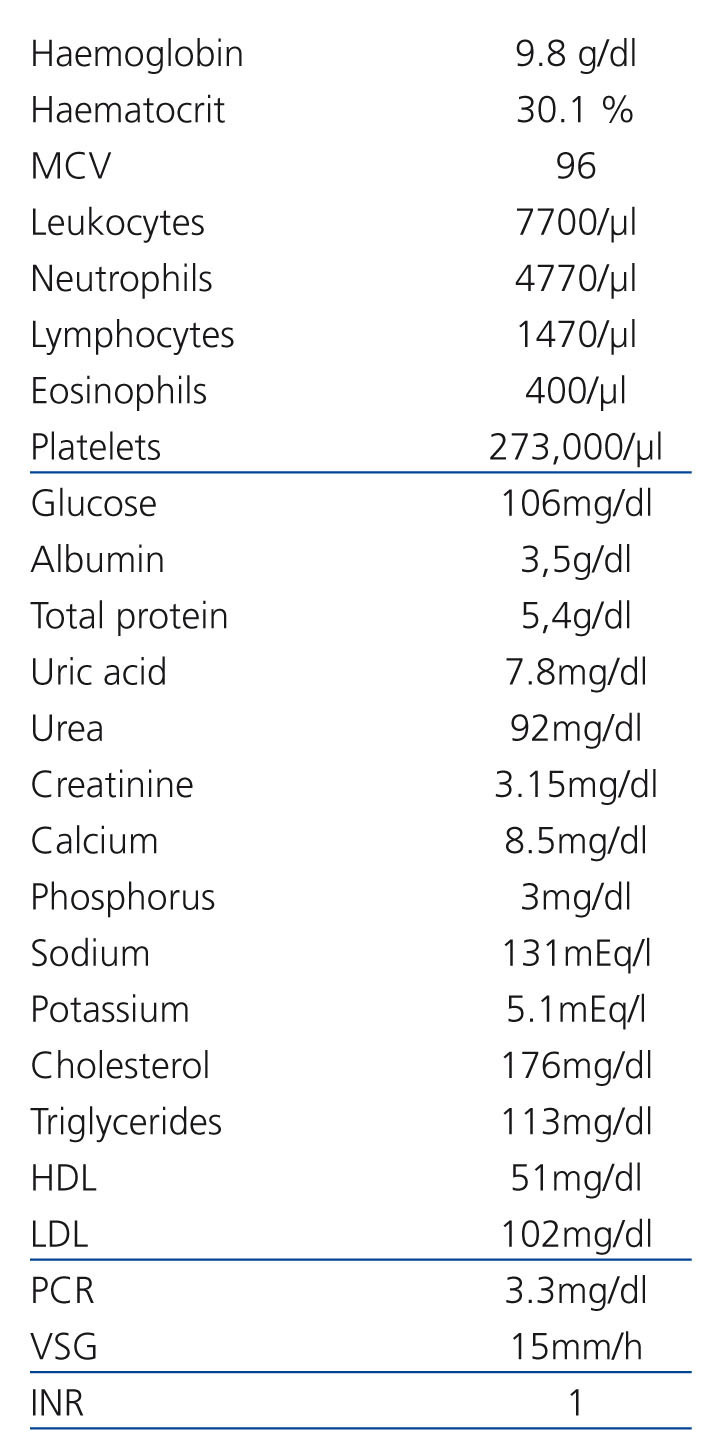
The clinical chemistry is displayed in Table 1. The urine sediment was normal, proteinuria and urine culture were negative and the immunological study and tumour markers were normal (prostate-specific antigen 2.33ng/ml). Echinococcus granulosus in blood was high, 9.18kU/l (0.00-0.35), and serology for Echinococcus IgG enzyme immunoassay (EIA) was negative. The chest X-ray excluded pulmonary lesions. On vesicoprostatic ultrasound we observed a large solid-cystic retrovesical mass with bilateral ureterohydronephrosis, grade IV in the right kidney (RK) and grade III in the left kidney (LK).
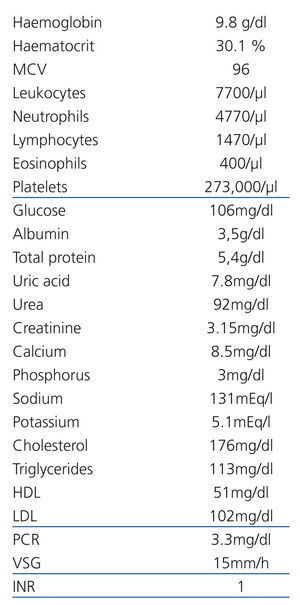
The MRI (Figure 1) showed a large space-occupying lesion of a maximum diameter of 17.5cm invading the pelvic cavity with the upper pole at the height of L4-L5, and almost total collapse of the bladder. It had a well-defined ovoid shape with multiple internal septa, consistent with hydatid cyst of Polat’s II2B type. In the lower pole of the LK, a 61mm ovoid lesion consistent with inactive type III hydatid cyst was observed. There was dilatation of both renal collecting systems, with reduced RK, which had a diameter of 84mm and cortical thinning. The LK had a longitudinal diameter of 11cm.
Following an unsuccessful attempt of ureteral catheterisation by cystoscopy, bilateral nephrostomy was performed with partial improvement of renal function (Cr 2.4mg/dl), through which two ureteral catheters were placed.
After two months of treatment with albendazole, supra- and infraumbilical midline laparotomy was performed, in which we observed a retrovesical cyst which occupied the entire lower pelvis and infiltrated the right lateral wall of the ureter. Intracystic injection was performed with hypertonic saline and subsequent aspiration of its contents, leaving a liquid with “grape skins”. Marsupialisation of the cyst was performed, maintaining the wall adjacent to the bladder and right nephroureterectomy.
The left ureteral catheter was removed 5 months after surgery. The pollakiuria and nocturia gradually improved, but nocturia persisted 2 to 3 times. Treatment with albendazole was maintained for a total of 6 months, with excellent tolerance. The Echinococcus granulosus in blood was 4.19kU/l and serology continued to be negative (IgG EIA index 0.52). Cr 1.5mg/dl was maintained with proteinuria of 1g/day.
From a renal point of view, hydatidosis can cause haematuria or low back pain.2 Also, glomerulonephritis mediated by immune complexes and secondary amyloidosis have been described.3,4 Several cases of retrovesical hydatid cyst2 have been published, although it is a rare form of manifestation (0.1%-0.5% of hydatid cysts).1 Most occur as a result of the rupture of an abdominal or pelvic cyst or dissemination by the Douglas pouch during a surgical procedure. It usually occurs with nonspecific urinary symptoms and even urinary retention. Fewer than 15% of retrovesical hydatid cysts2 can fistulise, particularly to the bladder,5,6 with hydatiduria being a sign of pathognomonic of vesicular cystic fistula.7
Our patient was referred for kidney failure study and was diagnosed with a large retrovesical hydatid cyst, with no history of rupture or surgery of an abdominal or pelvic cyst. It seems logical to think that, during the pulmonary cyst operation, haematogenous seeding occurred following rupture, with the formation of a pelvic cyst, which quietly grew over the years.
The detection of Echinococcus granulosus circulating antigens in serum is less sensitive than the detection of antibodies, which is the diagnostic method of choice.8 A negative serological test does not rule out echinococcosis, as occurred in our case. There are currently no serologic tests with sensitivity and specificity of 100%,8 so its result must always be compared with the radiological findings.
Chemotherapy with albendazole or mebendazole is recommended before and after surgery,9-11 since it reduces the risk of peritoneal seeding and decreases cystic tension for easier removal. We conducted preoperative treatment for 2 months with albendazole and a further 4 months after surgery.
We bring attention to this case since a detailed history and a high rate of suspicion, particularly in patients from endemic areas, help to establish the diagnosis of pelvic hydatidosis.
Conflicts of interest
The authors declare that they have no conflicts of interest related to the contents of this article.
Table 1. Analysis on admission
Figure 1. MRI