La dislipemia es un reconocido factor de riesgo cardiovascular en la población general, pero no así en pacientes con enfermedad renal crónica (ERC). Los objetivos del presente estudio han sido determinar si las alteraciones lipídicas más comunes, así como las concentraciones de apolipoproteína (apo) A y B, son capaces de predecir la mortalidad y el desarrollo de nuevos episodios cardiovasculares (CV) en pacientes con ERC en estadios previos a la diálisis. Se trata de un estudio de observación prospectivo histórico en el que se incluyeron 331 pacientes con ERC en estadios 4-5 prediálisis. Se determinaron los siguientes parámetros lipídicos: colesterol total, triglicéridos, HDL, LDL, apo A-I y apo B. Se analizó la asociación de estas variables con la mortalidad global y con el desarrollo de episodios CV. La mediana de seguimiento fue 985 días, y durante este período hubo 105 fallecimientos y 54 nuevos episodios CV. En un modelo multivariable de Cox ajustado al resto de covariables de reconocida importancia pronóstica, la razón de riesgo (RR) por cada 10 mg/dl de apo A fue de 0,915 (IC 95%: 0,844 a 0,992; p = 0,031). Los pacientes con una relación apo A/apo B elevada (tercil superior, >1,42) también tuvieron una supervivencia significativamente mejor que la del resto de los pacientes estudiados (RR = 0,592, IC 95%: 0,3680-0,953; p <0,05). No hubo relación significativa entre los parámetros lipídicos y el desarrollo de episodios CV. En conclusión, las concentraciones de apo A y una relación apo A/apo B elevada se asocian con un mejor pronóstico vital en pacientes con ERC prediálisis.
INTRODUCTION
Cardiovascular disease is the leading cause of death and disability in developed countries. The association between lipid alterations and increased cardiovascular mortality in the general population is a well-recognised fact.1,2
Patients with chronic kidney disease (CKD) are at a higher risk of developing cardiovascular diseases (CV) than the general population.3-5
However, in this patient group, we do not observe a correlation between increased lipid concentration and mortality.6,7 On the contrary, increased mortality associated with low total cholesterol levels has been shown in patients in advanced stages of CKD.8 The deterioration of the nutritional state caused by prolonged exposure to uraemia and dialysis and the development of malnutritioninflammation-atherosclerosis (MIA) syndrome could explain this epidemiological peculiarity which goes against the general tendency.7,9
However, CKD is associated with alterations in lipoprotein metabolism, in both initial and late stages. This can manifest itself independently from total plasma lipid concentrations, and could potentially contribute to accelerating the development of atherosclerosis.10-12
Apolipoproteins A (apo A) and B (apo B) are the structural proteins in HDL and LDL lipoproteins, respectively. Levels of apo B are better than LDL levels at reflecting the spectrum of proatherogenic lipid particles (VLDL, IDL and LDL).13 The antiatherogenic role played by apo A also appears to be more important than that of HDL, and this apolipoprotein is very much involved in the HDL particle maturation process mediated by lecithin-cholesterolacyltransferase,14 as well as in various antioxidant processes.15 Some epidemiological studies have shown that the relationship between apo A and apo B is a remarkable predictor of the development of ischaemic heart disease in the general population.16,17 The role these apolipoproteins play in predicting the evolution of CKD patients is not well understood.
The objectives of the present study are to determine whether the most common lipid alterations, as well as concentrations of apo A and apo B, are capable of predicting mortality and the development of new CV episodes in patients with CKD in predialysis stages.
MATERIAL AND METHODS
Patients
This historical prospective observational study included all consecutive patients referred for a predialysis consult between June 2003 and June 2007. The only inclusion criterion was having stage 3, 4 or 5 chronic kidney disease previous to dialysis.
The total number of patients under study was 331 (156 women and 175 men) with a mean age of 65 ± 15 years. The average follow-up period was 985 days. The renal failure aetiology was as follows: unregistered (116 patients), primary glomerulonephritis (58 patients), diabetic nephropathy (68 patients), chronic interstitial nephropathy (42 patients), renal polycystic disease (19 patients), ischaemic nephropathy (24 patients) and other kidney disease (6 patients).
The diagnosis of diabetic nephropathy was made according to clinical criteria in most cases (suspected diagnosis). In another 30 diabetic patients, we observed that the cause of renal failure was due to reasons other than diabetic nephropathy; in these cases, it was diagnosed using more conclusive methods (renal biopsy, imaging diagnosis showing polycystic disease or ischaemic nephropathy, etc.).
Comorbidity was very prevalent in this study group. Upon classifying the patients according to the associated disease copresence index (the comorbidity index described by Davies et al15 ), 134 showed no significant comorbidity, 147 had a mild to moderate comorbidity and 50 had severe comorbidity. Diabetes mellitus was the most frequent comorbidity (in 98 patients), followed by ischaemic disease of the central or peripheral nervous system (77 patients), heart failure (66 patients) and ischaemic heart disease (48 patients).
The most frequently-prescribed drugs in the study group were antihypertensives (angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, etc.), diuretics, statins, platelet antiaggregants and phosphorus binders.
Collection of clinical data and laboratory analysis
The clinical and analytical data were collected during the first visit, which was recorded as the beginning of follow-up of patient evolution. The information on the associated comorbid processes was obtained from the clinical history. The diagnosis of ischaemic heart disease was considered if the patient presented one of the following: previous myocardial infarction, clinical signs of ischaemic heart disease, or a positive angiogram, stress test result or isotope scan. Peripheral vascular disease was diagnosed in cases with clear clinical symptoms or signs, or when there was shown to be significant stenosis (> 50%) in the distal aortic, renal, lower limb or carotid areas. Patients with an aortic aneurism were also included in this group.
A new CV episode was considered to be the development of acute severe ischaemic processes: myocardial infarction, unstable angina, transient ischaemic attacks or cerebrovascular accidents, or severe ischaemia of the lower limbs. Sudden death by an undetermined cause was not considered to be a CV episode.
After nocturnal fasting, blood was drawn to analyse the following: complete blood count, urea, creatinine, calcium, phosphorus, albumin, total cholesterol, HDL-cholesterol and triglycerides (Hitachi 917, Roche Diagnostics, Germany), bicarbonate (IL-1306 gas analyzer, Instrumental Laboratory, Milan, Italy) and C-reactive protein (nephelometry, N High Sensitivity CRP, Behring, Marburg, Germany). Levels of LDL cholesterol were estimated using the formula by Friedwald et al.18 Glomerular filtration rate was estimated by the MDRD-4 method19 and proteinuria was measured in 24-hour urine samples using a benzethonium chloride turbidimetric assay (U/CSF protein, Roche Diagnostics, Germany).
Measuring plasma levels of apolipoproteins A-I and B was done by immunonephelometry (Behring Nephelometer BNII, Marburg, Germany), with inter-assay coefficients of variation of 5% for apolipoprotein A and 4% for apolipoprotein B.
Study design and statistical methods
Death due to any cause and the development of new CV episodes, whether or not they were fatal, were the events for analysis.
Patients were monitored following the initial evaluation with regular visits every 1 to 3 months while they continued in predialysis treatment, or by indicating any change in evolution after beginning dialysis; they were censored in cases of death due to any cause, kidney transplant, interrupted follow-up or upon reaching the end date for the study (November 2008).
To evaluate apo A and apo B¿s ability to predict mortality or the development of new CV events, we performed a discrimination analysis by constructing ROC (receiver operating characteristic) curves and calculating the area under the curve. According to the results of this analysis, we chose the best predictor parameter(s) and examined the clinical and biochemical characteristics of patients in each tertile of distribution frequencies for that parameter in order to find confounding factors. Continuous variables were compared between groups using analysis of variance (ANOVA) or the Kruskal-Wallis test, according to the distribution characteristics of the variables. The post hoc comparisons were made by using the Scheffe test. To compare two continuous independent variables, we used the Student-t test for unpaired samples or the non-parametric Mann-Whitney test according to the distribution characteristics of the variables. The chisquare test was used to compare discrete variables. The degree of relationship between two continuous parameters was analysed using Pearson¿s correlation coefficient.
To establish whether or not there was an independent association between study variables (apolipoproteins) and mortality or the development of new CV episodes, we used multivariate Cox proportional hazards models and we determined relative risks and 95% confidence intervals. These study variables were analysed both continuously and discretely (tertiles).
The models were adjusted upon introducing variables or risk factors with a potential influence on the final phases of the study (age, sex, comorbidity index, plasma albumin, Creactive protein, residual renal function, proteinuria, statins, etc.). The choice of the variables best adjusted to the models was performed automatically by the progressive conditional elimination process.
To confirm risk proportionality in all survival studies, we examined graphs from correlating the logarithm (-survival rate logarithm) with the survival time logarithm, and graphs of partial residues of each covariable compared with survival time.
Data from this study was presented as means and standard deviations (± SD), or as medians and interquartile ranges. A value of p < 0.05 was considered to be statistically significant. Statistical analysis was performed and graphics created using SPSS software version 15.0 (SPSS, Chicago, USA).
RESULTS
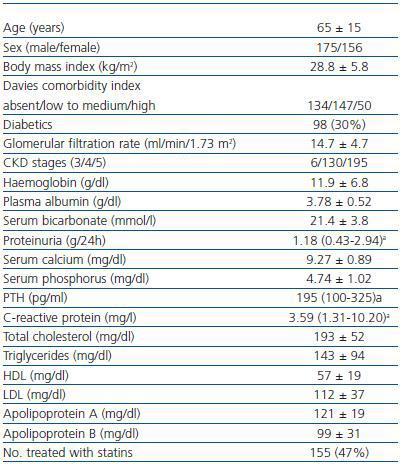
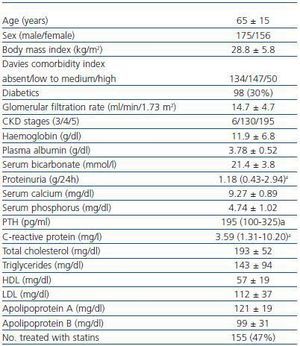
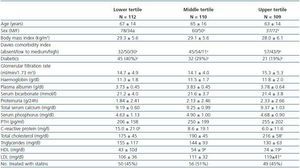
The most important characteristics of the patients in the study are shown in table 1. Note that the patients¿ mean total cholesterol and lipoprotein levels are in an acceptable range, and so are their apolipoproteins.
Almost half of the patients were being treated with different statin drugs with widely varying doses. There were no significant differences in total cholesterol, HDL, LDL, apo A or apo B among the patients receiving and not receiving statins. Patients treated with statins showed significantly higher triglyceride and VLDL levels (165 ± 99 compared to 124 ± 85mg/dl; p < 0.0001; 33 ± 25 compared to 22 ± 16mg/dl; p < 0.0001, respectively, Student-t test), and lower C-reactive protein levels than in untreated patients, with a difference in the statistical significance limit (7.5 ± 11.9 compared to 12.1 ± 21.9mg/l; p = 0.06; Mann-Whitney test).
Association between lipid, lipoprotein and apolipoprotein levels and mortality/new cardiovascular episodes
During the study period (median follow-up length: 985 days), there were 105 deaths, 54 new CV episodes, 15 follow-up interruptions, 185 starting dialysis and 37 receiving kidney transplants in the patient group. The median follow-up length before starting dialysis (predialysis period) was 549 days.
In the ROC curve analyses, no significant associations were observed between total levels of cholesterol, triglycerides or LDL and mortality. HDL concentrations were negatively associated with mortality (area below the curve 0.416, p = 0.014). The apo A concentrations were also negatively associated with mortality, but with a lower level of significance (area below the curve 0.372; p < 0.0001).
Concentrations of apo B were not related with mortality, but the apo A/apo B quotient was, although not as strongly as apo A concentrations (area below the curve 0.403; p = 0.005).
The only parameter that was significantly associated with the development of new CV episodes was the concentration of apo A (area below the curve 0.410; p = 0.035).
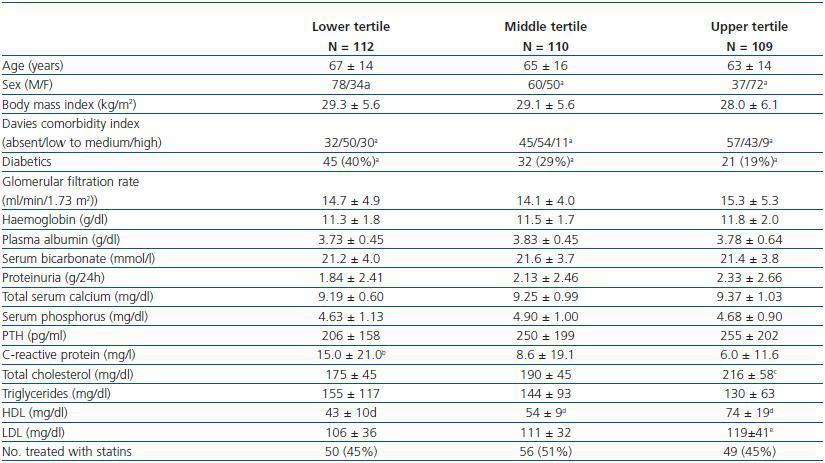
Table 2 shows the characteristics for patients grouped by apo A tercile. We observe significant differences for sex, comorbidity index and levels of C-reactive protein among the three groups. Women were predominant (78%) in the patients grouped in the upper tertile for apo A, which had a lower incidence rate of associated diseases and above all, for diabetes mellitus (19% compared to 40% in those grouped in the lowest tertile for apo A). Patients grouped in the lowest tertile had significantly higher levels of C-reactive protein than the rest of the subgroups. Patients with higher apo A concentrations also had higher levels of total cholesterol, HDL and LDL. No differences in the proportion of patients treated with statins were found among the three subgroups.
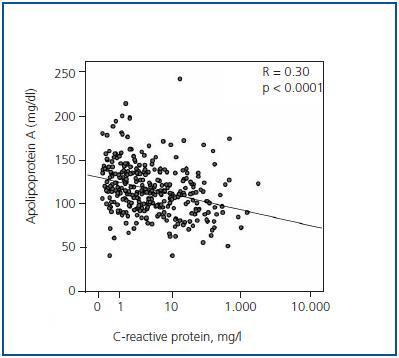
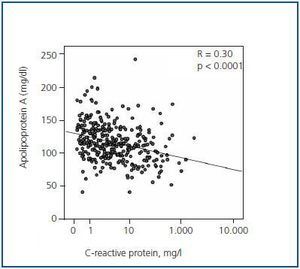
An inverse linear correlation was observed between concentrations of apo A and C-reactive protein (as a logarithm) (r = -0.30; p < 0.0001) (figure 1), but not with plasma albumin (r = -0.021; NS).
Apolipoprotein A concentrations, apo A/apo B quotient and survival or development of new cardiovascular episodes
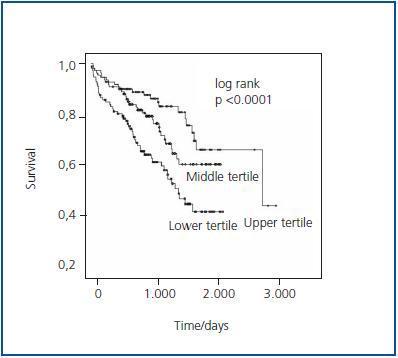
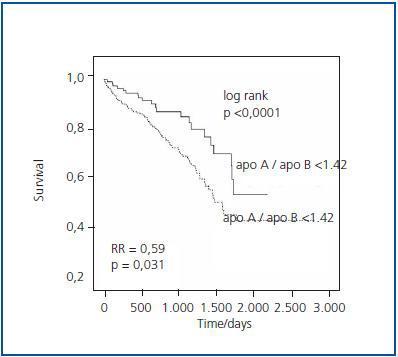
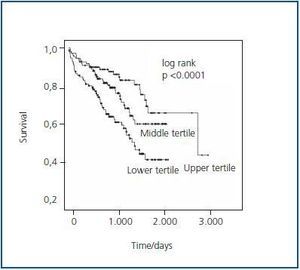
In survival curves made using the Kaplan-Meier method without adjusting for other factors with a potential influence on mortality, we observed significant differences among patients grouped according to apo A tertile (log-rank = 17.05; p < 0.0001) (figure 2). We also observed differences in the statistical significance limit for survival with no new CV episodes; it was more favourable in those patients grouped in the upper tertile for apo A (log-rank = 5.76; p = 0.056).
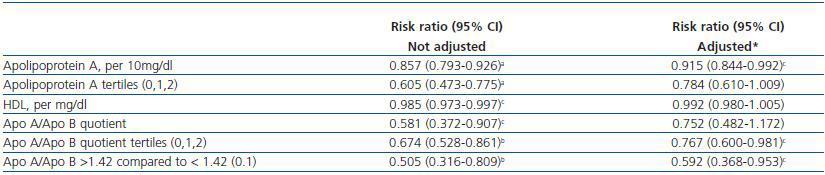
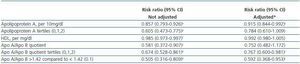
In a multivariate Cox model adjusted by age, sex, body mass index, comorbidity index, serumalbumin, C-reactive protein, statin treatment and residual renal function, the risk ratio (RR) for each 10mg/dl of apo A was 0.915, with 95% confidence intervals (CI) of 0.844 and 0.992 (p = 0.031) (table 3).
When the variable apo A is introduced in the multivariate model in the form of distribution frequency tertiles, statistical significance was not reached (RR = 0.784; 95% CI: 0.610-1.009; p = 0.059).
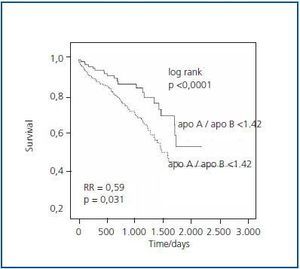
The substitution of the variable apo A by HDL concentrations did not improve adjustment of the multivariate model (table 3). Substitution of apo A with the apo A/apo B quotient in the multivariate model was not significant (table 3). Rather, statistical significance was observed as a survival predictor when the variable was introduced in the form of apo a/apo b tertiles or high levels (upper tertile, i.e. apo A/apo B > 1.42) (table 3 and figure 3).
The main factors determining the development of new CV episodes in the multivariate model were age (RR for each additional 10 years: 1.39; 95% CI: 1.06-1.72), and the comorbidity index (RR = 4.340; 95% CI: 2.819-6.682). No lipid parameters or statin treatment analysed in this study were significantly correlated with the development of new CV episodes in the adjusted models.
DISCUSSION
The results of this study show that total serum cholesterol and triglyceride levels are not associated with mortality in CKD patients in pre-dialysis. In addition, levels of LDL cholesterol and apolipoprotein B (apo B13), which is theoretically the best indicator representing atherogenic lipid particles, were not associated with a poorer survival rate. Instead, the lipid parameters with the strongest association with survival were apolipoprotein A (apo A) concentrations and the apo A/apo B relationship. This parameter¿s association with survival was not linear; more favourable survival was only observed in patients with the highest levels (upper tertile). None of the lipid parameters under study was related to the development of new CV episodes during the follow-up period in an analysis adjusted by other risk factors.
The results of the studies analysing the relationship between lipid alterations and mortality in CKD patients on dialysis conclude that there is no association, or even that there is a paradoxical or contradictory association, to that observed in the general population: a lower survival rate in those cases with lower total cholesterol or LDL cholesterol levels.6-9
An exception to these observations may be found among black CKD patients, whose survival may be affected negatively by hypercholesterolaemia, even in those undergoing dialysis.20 The negative effect on the nutritional state caused by prolonged exposure to terminal uraemia, dialysis procedures and the development of inflammation have been cited as a possible explanation for the inverse relationship between lipid alterations and mortality.7,9 The present study includes only patients with advanced CKD who have not yet begun dialysis so as to limit some of the confounding factors. But even in predialysis states, no relationship was observed between cholesterol levels, LDL, apo B or triglycerides and mortality or new CV episodes. Unlike other studies of predialysis patients with CKD,9 we found no negative relationship between total cholesterol or LDL levels and mortality in this study. It is likely that the preserved nutritional state found in most of our patients would explain the differences between this study¿s findings and those of other studies.
The mean concentration of apo A-I decreases proportionally to the decrease in glomerular filtration rate in CKD,21 and this metabolic alteration is considered to be a CV risk factor, although no studies have demonstrated a relationship between the levels of this protein and mortality in CKD. The results from the present study show that high concentrations of apo A-I are associated with better survival.
Some demographic, clinical and biochemical characteristics of the patients grouped into tertiles according to the apo A level distribution frequency were significantly different. The patients with the highest concentrations of apo A were younger, predominantly female, with a lower number of diabetics and lower overall comorbidity, and a significantly lower mean level of C-reactive protein. Furthermore, we observed a significant correlation between apo A and Creactive protein levels. This association between apo A levels and inflammation markers has already been described,22,23 and this apolipoprotein can be considered a negative acutephase reactant. In this way, it is difficult to determine whether the positive effect that high apo A levels have on CKD patient survival is due to the antiatherogenic mechanism, or if it simply serves as an indirect inflammation marker, or if both are true. However, we must point out that apo A levels added prognostic information about the survival of these patients when introduced in multivariate models including covariables such as age and the comorbidity index, as well as albumin and C-reactive protein levels.
Although a good correlation was made between the apo A and HDL levels, it is possible that the predictive power of mortality for any reason was better with apo A than with HDL. In the final phase of the study, mortality was significantly associated with apo A levels, but not HDL levels.
The apo A/apo B ratio was associated with survival, but not as a monotonic function. Only those patients with a high ratio had a higher survival rate. It is likely that high levels of apo A/apo B identify patients with a better vital prognosis and coincide with characteristics such as absence of inflammatory and malnutrition process, along with controlled apo B levels (whether or not by pharmacological means) that are more similar to those providing contrasted survival benefits to the general population.
This study has certain limitations. The study had set covariables, and did not consider variables that changed over time (increases or decreases in lipid values in a certain follow-up time). A large percentage of patients received treatment with statin drugs, and although this covariable was taken into account for all survival analyses, we cannot rule out the possibility of a certain degree of influence over the results due to medication and dose heterogeneity, and due to maintaining the prescription over time.
In addition to the apolipoproteins A-I and B, there are others (apo A-IV, apo E, apo[a], etc.) that may have a potential effect on the evolution of these patients, and which were not analysed in this study.
To conclude, the total serum lipid and lipoprotein levels in predialysis patients with advanced CKD do not affect survival or the development of new CV episodes. On the other hand, high apo A levels and a high apo A/apo B ratio were associated with a better vital prognosis in this patient group.
Before we can recommend measuring these apolipoproteins as prognostic markers in CKD, additional studies will be needed to determine their relationship with subclinical arteriosclerosis, as well as effects that pharmacological modifications to plasma concentrations of these proteins may have on patient survival.
Table 1. Clinical and biochemical characteristics of patients included in the study
Figure 1.
Table 2. Characteristics of patients grouped in tertiles according to the frequency distribution of apolipoprotein A level
Figure 2.
Table 3. Prognostic value of the different study parameters for mortality, in Cox regression models with or without adjustment for other covariables.
Figure 3.