Antecedentes: La peritonitis fúngica es una complicación infrecuente pero grave en pacientes en diálisis peritoneal continua ambulatoria (DPCA). Métodos: Durante un período de 10 años (1999- 2008), de un total de 175 pacientes con insuficiencia renal crónica en tratamiento con DPCA, estudiamos retrospectivamente 10 casos de peritonitis fúngica, analizando los factores predisponentes, aspectos clínicos, agentes etiológicos y tratamiento. El diagnóstico se estableció por la presencia de efluente peritoneal turbio con recuento superior a 100 leucocitos/μl y aislamiento de hongos en el cultivo microbiológico. Resultados: La peritonitis fúngica representó un 3,6% del total de peritonitis. Nueve pacientes tenían historia de peritonitis bacteriana previa y todos habían recibido antibioterapia. Otros hallazgos destacables fueron: edad superior a 70 años (50%) y diabetes mellitus (40%). El examen microscópico del líquido peritoneal fue de utilidad para sospechar la infección en 6 pacientes (60%). Los agentes responsables de peritonitis fueron: Candida parapsilosis (4), C. albicans (2), C. tropicalis (1), C. glabrata (1), C. famata (1) y Fusarium oxysporum (1). Los antifúngicos utilizados en el tratamiento fueron: fluconazol intraperitoneal y oral, vorizonazol intravenoso y oral y anfotericina B intravenosa. A consecuencia de la infección fúngica, 8 pacientes fueron transferidos a hemodiálisis. Un paciente murió antes de ser diagnosticado y otros tres durante el episodio de peritonitis. Conclusiones: Los pacientes con episodios de peritonitis bacteriana previos y tratamiento antibiótico presentaron un mayor riesgo de desarrollar peritonitis fúngica. C. parapsilosis fue el patógeno más frecuente. El tratamiento antifúngico junto con la retirada del catéter peritoneal fue eficaz en el 60% de los pacientes.
SUMMARY
What is known about this issue?
Fungal peritonitis is one of the most serious complications of peritoneal dialysis. It is rare, but carries a high morbidity and mortality. Previous episodes of bacterial peritonitis and antibiotic therapy are major risk factors. Yeasts are the most common aetiologic agents. Treatment is not fully established.
What is the purpose of this study?
This study reports our experience of fungal peritonitis over 10 years, demonstrating its low incidence in patients on peritoneal dialysis (episodes of peritonitis account for 3.6% of the total). We report on its severity (40% mortality), the importance of risk factors for the development of the infection, the use of direct microscopy in aetiological diagnosis (60% sensitivity), the increase in non-albicans Candida species in the aetiology (80%), especially C. parapsilosis, a predominant species with a poor prognosis, and the usefulness of fluconazole for treatment.
INTRODUCTION
Peritonitis is one of the most common complications in patients on peritoneal dialysis, especially of bacterial origin. Fungal infection is rare but is associated with high morbidity, as it can lead to catheter obstruction, abscess formation and development of sclerosing peritonitis. This is associated with high mortality1-12 and it also leads to peritoneal dialysis failure, which means that the patient has to transfer to haemodialysis. It occurs in patients who have spent a long time on a peritoneal dialysis programme and who have previous episodes of bacterial peritonitis and treatment with broad spectrum antibiotics, among other predisposing factors.1,2,5,7-18 Its clinical presentation is similar to bacterial peritonitis and its aetiology includes most species of yeast and pathogenic and environmental filamentous fungi, although Candida species are the most common, especially C. albicans.1,5,9,12,14,15,19
The treatment of fungal peritonitis is not well established. There are only a few studies with a small number of patients treated. There are indications from the International Society of Peritoneal Dialysis and the Spanish Society of Nephrology, which recommend the removal of the peritoneal catheter along with administration of antifungal agents.5,6,8,10,12,15-17,20,21
The aim of this study was to analyse predisposing factors, clinical aspects, aetiology and treatment guidelines for patients on continuous ambulatory peritoneal dialysis who developed an episode of fungal peritonitis over a 10-year period.
MATERIALS AND METHODS
A retrospective study of cases of fungal peritonitis between January 1999 and December 2008 was performed. A total of 175 patients with chronic kidney disease were included on a programme of continuous ambulatory peritoneal dialysis, of whom 95 were men and 80 women with a mean age of 54.6 years (17-84 years). The causes of renal failure were diverse: vascular (17.1%), glomerulonephritis (21.1%), diabetic nephropathy (17.7%), interstitial nephropathy (16.0%), polycystic kidney disease (4.6%), others (4.6%) and unknown (19.4%).
Fungal peritonitis was suspected with the following symptoms: presence of abdominal pain, fever, impaired condition in general, cloudy peritoneal effluent with a count of 100 or more leukocytes/μl and more than 50% polymorphonuclear cells, with a torpid development and previous antibiotic therapy. It was confirmed by isolation of the fungi in microbiological culture.
To determine the aetiology, 50-100ml of peritoneal fluid was sent to the microbiology laboratory. Some of the fluid was cultured in blood culture bottles, the rest was centrifuged at 3,000 rpm for 15 minutes and the precipitate examined directly under a microscopic with lactophenol blue, Gram stain and blood agar culture, MacConkey agar and Sabouraud dextrose agar with chloramphenicol. The yeasts were identified by their growth characteristics on CHROMagar Candida media and by the commercial system, carbon compounds assimilation ID 32C (bioMérieux, France). Filamentous fungi were identified by colony characteristics and microscopic observation of the fungal components. Antifungal susceptibility testing using the Sensititre YeastOne system (AccuMed International, UK) was also used.
RESULTS
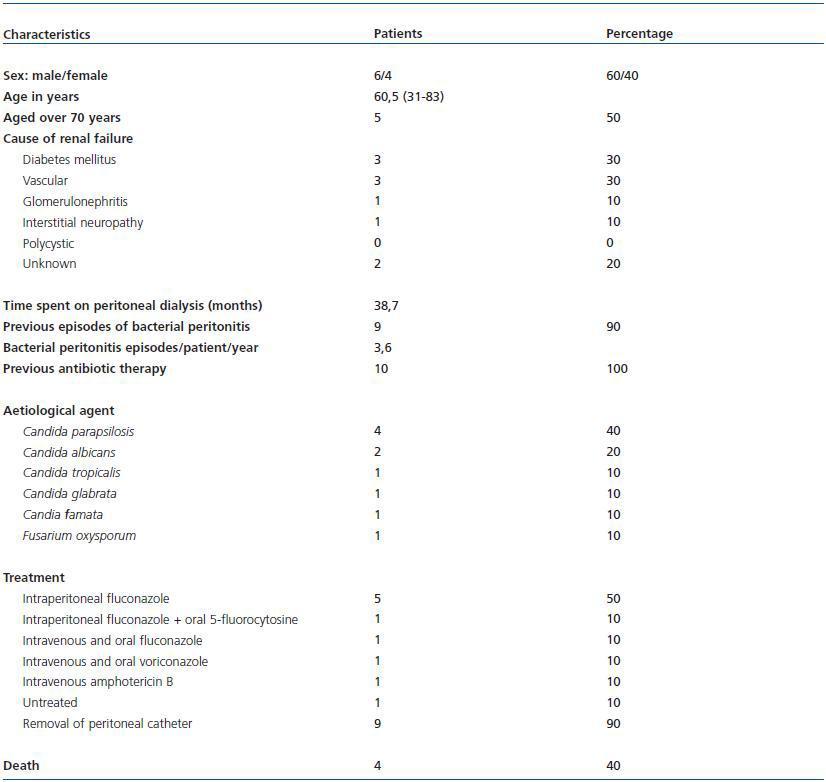
The number of episodes of peritonitis detected during 1999-2008 in the 175 patients under study was 278, of which only 10 were fungal peritonitis (3.6% of total number of peritonitis episodes). The overall average of peritonitis per patient per year was 1.4 in patients with bacterial peritonitis and 3.6 in patients with fungal peritonitis. The characteristics of these 10 patients are shown in Table 1.
About 60% of the patients were men and 50% were older than 70. The average time spent on the peritoneal dialysis programme was 38.8 months. 90% had had previous episodes of bacterial peritonitis. All patients had received antimicrobial therapy within 2 months prior to the onset of fungal infection.
Microscopic examination of peritoneal fluid led to the diagnosis in 6 patients (60%). Yeast growth was detected in nine of the episodes, all belonging to the genus Candida, but of four different species. The hyaline filamentous fungus Fusarium oxysporum was identified in just one case. The yeasts showed in vitro sensitivity to amphotericin B, fluconazole, ketoconazole, voriconazole and 5-fluorocytosine; a strain of C. tropicalis were resistant to itraconazole.
All patients had abdominal pain and cloudy peritoneal effluent with greater than 100 leukocytes/μl and more than 50% polymorphonuclear cells. Fever was observed in three of them, and hypoalbuminaemia was detected in two.
One 83-year old patient with peritonitis due to C. glabrata died the day after demonstrating clinical symptoms, without specific treatment and prior to confirmation of mycological diagnosis. The remaining patients suspected of having a fungal infection were given antifungal treatment and had their peritoneal catheters removed. During the fungal infection, eight patients required haemodialysis and three of them died: two with peritonitis due to C. parapsilosis and the other due to C. famata. Only one patient had the peritoneal catheter reinserted again 4 weeks after the end of clinical symptoms, and was successfully returned to the peritoneal dialysis programme. The overall mortality rate was 40%.
DISCUSSION
The incidence of fungal peritonitis in patients on peritoneal dialysis ranges from 1 to 23% of all episodes of peritonitis, according to various authors.1-14 In our experience, the incidence was low, only 3.6%. However, compared with another study conducted between 1982-1989 on 100 patients with 161 episodes of peritonitis, 22 with an incidence of 1.9%, there was a noticeable increase of fungal infection. Innovation in peritoneal dialysis systems and the use of more biocompatible solutions are considered key factors in reducing episodes of bacterial peritonitis. However, for fungal peritonitis, there appear to be other factors that contribute to reducing infection, mainly preventive measures, early removal of the peritoneal catheter and the use of antifungal agents.16
Knowledge of the risk factors is important in preventing fungal infection, especially pre-treatment with broadspectrum antibiotics,1,2,4-10,12-15 which in our study was present in all patients, following episodes of bacterial peritonitis in 90% of cases. We also noted a greater number of episodes of peritonitis in patients with fungal infection, more than double that in patients with bacterial peritonitis. 2,7-9,12,23 Advanced age and diabetes mellitus were other factors associated with fungal peritonitis in our study.3-5,8,9,12,15,17,24,25
Growth in a culture medium was instrumental in establishing the aetiology. The Candida yeasts were responsible for most episodes of peritonitis, as happened in many other published studies.1,3,5,8,9,12,14,15,19,23,25,26 C. albicans is the most common species in most publications, but in recent years non-albicans species have gained some prominence, especially C. parapsilosis, which is sometimes found in similar numbers to C. albicans. In our study, C. parapsilosis was the main species causing fungal peritonitis, followed by C. albicans. The isolation of C. tropicalis is not very frequent,3,19,25 and even less in C. glabrata8,19,25,27 and C. famata.5,25,28 Filamentous fungi account for a small percentage compared to yeast in most studies, as happened in ours, although the genera described are very diverse. The genus Fusarium has been reported on rare occasions.3,17,29-31
The yeasts in our series had an excellent in vitro sensitivity to antifungal agents recommended for the treatment of fungal peritonitis. These results are consistent with those reported in more extended sensitivity studies32,33 and suggest that empirical treatment is reasonable for certain infections attributed to the Candida species.
In our patients, the clinical manifestations were similar to those described for bacterial peritonitis, and the evolution of the fungal infection was similar to other published studies.1,6,8,11,12,14,17,18,34 The fungal infection led to the removal of the peritoneal catheter and the abandonment of the dialysis programme. According to most authors, early withdrawal of the catheter within 24 hours is essential to resolve the clinical picture associated with the introduction of antifungal therapy.5,6,8,10,15-17,21 The recommended antifungal treatments for fungal peritonitis are limited: fluconazole, voriconazole, amphotericin B and caspofungin. The most recommended is intraperitoneal fluconazole associated with oral 5-fluorocytosine. Intravenous amphotericin B alone or in combination with other antifungal agents is also used, although the benefits have not been shown.4,9,25,35 We obtained good results with fluconazole for cases of peritonitis caused by C. albicans but not C. parapsilosis or C. famata, although both strains showed in vitro sensitivity to antifungal treatments. It seems therefore that the cause of death was related to other factors, including the aetiology of the peritonitis. Two of the deceased patients were infected by C. glabrata, C. famata and C. parapsilosis, suggesting that the peritoneal infection by non-albicans species may be worse and corroborates the view of some authors that the presence of C. parapsilosis is a poor prognosis factor.14,23,36
Some authors believe that the use of new dialysis solutions with bicarbonate or low concentrations of lactate and glucose can improve patient response to fungal infection, although there are few studies in this respect.37 Moreover, it has been reported that patients with repeated episodes of peritonitis and prolonged antibiotic therapy may have a decreased risk of fungal infection by prophylaxis with oral fluconazole (100mg/day) or daily rinses with nystatin.24,38
In conclusion, fungal peritonitis in peritoneal dialysis is a rare but serious complication, which stops the technique from functioning, requiring transfer to haemodialysis. Previous episodes of bacterial peritonitis and antibiotic therapy are the most common risk factors. Clinical manifestations are similar to bacterial peritonitis. Peritoneal fluid microscopy is useful for suspected fungal infection. The Candida yeasts, especially C. albicans and in recent years C. parapsilosis, are responsible for most episodes; infection with filamentous fungi is occasional. Treatment requires removal of the peritoneal catheter and administration of antifungal agents, with fluconazole considered the first choice. Early diagnosis and treatment reduce morbidity and mortality.
Table 1. Characteristics of nine patients with fungal peritonitis