The influence of socioeconomic and cultural barriers in the choice of renal replacement therapy (RRT) techniques in advanced chronic kidney disease (ACKD) has been scarcely explored, which can generate problems of inequity, frequently unnoticed in health care.
The aim of this study is to identify the "non-medical" barriers that influence the choice of RRT in an advanced chronic kidney disease (ACKD) consultation in Spain.
Material and methodsRetrospective analysis including the total number of patients seen in the ACKD consultation in a tertiary hospital from 2009 to 2020. Inclusion in the ACKD consultation began with an eligibility test and a decision-making process, conducted by a specifically trained nurse. The variables considered for the study were: age, sex, etiology of CKD, level of dependence for basic activities of daily living (Barthel Scale) and instrumental activities of daily living (Lawton and Brody Scale), Spanish versus foreign nationality, socioeconomic level and language barrier. The socioeconomic level was extrapolated according to home and health district by primary care center to which the patients belonged.
ResultsA total of 673 persons were seen in the ACKD consultation during the study period, of whom 400 (59.4%) opted for hemodialysis (HD), 156 (23.1%) for peritoneal dialysis (PD), 4 (0.5%) for early living donor renal transplantation (LDRT) and 113 (16.7%) chose conservative care (CC). The choice of PD as the chosen RRT technique (vs. HD) was associated with people with a high socioeconomic level (38.7% vs. 22.5%) (p = 0.002), Spanish nationality (91% vs. 77.7%) (p < 0.001), to a lower language barrier (0.6% vs 10.5%) (p < 0.001), and to a higher score on the Barthel scale (97.4 vs 92.9) and on the Lawton and Brody scale (7 vs 6.1) (p < 0.001). Neither age nor sex showed significant differences in the choice of both techniques.
Patients who opted for CC were significantly older (81.1 vs 67.7 years; p < 0.001), more dependent (p < 0.001), with a higher proportion of women (49.6% vs 35.2%; p = 0.006) and a higher proportion of Spaniards (94.7% vs 81%, p = 0.001) in relation to the choice of other techniques (PD and HD). Socioeconomic level did not influence the choice of CC.
ConclusionDespite a regulated decision-making process, there are factors such as socioeconomic status, migration, language barrier and dependency of the population that influence the type of RRT chosen. To address these aspects that may cause inequity, an intersectoral and multilevel intervention is required with interdisciplinary teams that include, among others, social workers, to provide a more holistic and person-centered assessment.
La influencia de los determinantes sociales de la salud en la elección de las técnicas de tratamiento renal sustitutivo (TRS) en la enfermedad renal crónica avanzada (ERCA) ha sido escasamente explorada, pudiendo generar problemas de inequidad, frecuentemente desapercibidos en la asistencia sanitaria.
El objetivo de este estudio es identificar las desigualdades sociales y económicas que influyen en la elección de TRS en una consulta de Enfermedad renal crónica avanzada (ERCA) en España.
Material y métodosAnálisis retrospectivo incluyendo el total de pacientes atendidos en la consulta de ERCA en un hospital terciario desde 2009 a 2020. La inclusión en la consulta de ERCA comenzaba por un proceso de toma de decisiones, conducido por una enfermera específicamente instruida. Las variables consideradas para el estudio fueron: edad, sexo, etiología de la ERC, nivel de dependencia para las actividades básicas de la vida diaria (Escala de Barthel) y actividades instrumentales de la vida diaria (Escala de Lawton y Brody), nacionalidad española versus extranjera, nivel socioeconómico y barrera idiomática. El nivel socioeconómico se extrapoló según el domicilio y el distrito sanitario por centro de atención primaria al que pertenecían los pacientes.
ResultadosUn total de 673 personas fueron atendidas en la consulta de ERCA en el periodo de estudio, de los cuales 400 (59,4%) optaron por la técnica de hemodiálisis (HD), 156 (23,1%) por diálisis peritoneal (DP), 4 (0,5%) por trasplante renal de donante de vivo (TRDV) anticipado y 113 (16,7%) eligieron tratamiento conservador (TC). La elección de DP como técnica de TRS elegida (frente a HD) se asoció a personas con nivel socioeconómico alto (38,7% vs 22,5%) (p = 0,002), a la nacionalidad española (91% vs 77,7%) (p < 0,001), a una menor barrera idiomática (0,6% vs 10,5%) (p < 0,001), y a una mayor puntuación en la escala de Barthel (97,4 vs 92,9) y en la escala de Lawton y Brody(7 vs 6,1) (p < 0,001). Ni la edad ni el sexo mostraron diferencias significativas en la elección de ambas técnicas.
Los pacientes que optaron por TC eran significativamente de mayor edad (81,1 vs 67,7 años; p < 0,001), más dependientes (p < 0,001), con una mayor proporción de mujeres (49,6% vs 35,2%; p = 0,006) y una mayor proporción de españoles (94,7% vs 81%, p = 0,001) en relación con la elección de otras técnicas (DP y HD). El nivel socioeconómico no influyó en la elección de TC.
ConclusiónA pesar de que el proceso de toma de decisiones en la elección de TRS está reglado y estandarizado, existen factores como la situación socioeconómica, la migración, la barrera idiomática o la dependencia que influyen en el tipo de TRS elegido. Para abordar estos aspectos que pueden ser causa de inequidad se requiere de una intervención intersectorial y multinivel con equipos interdisciplinares que incluyan, entre otros, trabajadores sociales, para brindar una evaluación más holística y centrada en la persona.
There are studies that claim that incorporating patients with advanced chronic kidney disease (ACKD) into the decision making process regarding the choice of renal replacement therapy (RRT) would achieve an equal distribution between hemodialysis (HD) and home techniques (home HD and peritoneal dialysis [PD]).1,2 However, the reality is that, despite their undoubted advantages,3 home techniques continue to be underused RRT modalities in a large proportion of countries, including Spain.4–6 The latest report of the Spanish Registry of Renal Patients in 2020 shows that, as in the previous year, only 16% of the incident population in RRT chose PD, while 79.5% chose HD and 4.5% received a renal transplant (RT), mostly from a living donor, with no official data on the choice of conservative treatment (CT).6 This low use of home techniques is influenced by various factors and numerous ideas have been put forward to help minimize the barriers to the adoption and retention of these treatments at home.7,8
It is well known that clinical factors, such as severity of comorbid conditions,9 or considerations related to the individual values of the person making the choice, for example, the need for travel or independence10 have an influence on the patient´s choice of the modality of RRT. However, the influence on the choice of technique of socioeconomic and cultural barriers has not been explored adequately, and it may generate an undetected inequity problem in health care. Since the publication in 1974 of the Lalonde report, it has been known that sociodemographic, economic and cultural determinants explain more than 75% of health outcomes,11 thus it is essential to consider the individual, including his or her background and circumstances, in order to address needs and activities we propose to carry out with an individual patient.
The main objective of this study was to identify the "non-medical" barriers that influence the choice of RRT, such as demographic factors, CKD etiology, socioeconomic factors, nationality or language in an ACKD consultation in a tertiary hospital in Spain. As a secondary variable, we analyzed glomerular filtration rate (GFR) on arrival at the ACKD clinic and whether or not they were potential candidates for RT.
MethodsPatientsThis is a retrospective analysis performed from 2009 to 2020 of all patients seen in the ACKD outpatient clinic (CKD stages 4 and 5) (estimated GFR rate < 30 ml/min/1.73 m2) of the Hospital del Mar, in Barcelona (Catalonia, Spain), who had completed the discussionn and decision-making process.
Decision-making methodologyInclusion of the patient in the ACKD clinic was initiated through a nursing consultation, which was the one that carried out the decision-making process, and consisted of 3 consecutive visits, divided into 3 phases. In the first phase, the patient's values and preferences were explored using value cards labeled "not important", "somewhat important", and "very important", and from which the patient chose 2 cards that were “very important ones” (for example, if a patient chose "to be independent" and "fear of blood and needlesticks", his possible most value-oriented treatment option could be PD). In a second phase, information about the different options available was provided with audio-visual material. Finally, in a third deliberative phase, the patient made a decision on their choice of RRT modality, whenever he felt ready After a clinical assessment to determine whether or not the option was feasible, patients that opted for PD were sent to a specific clinic on this technique with the nurse and physician responsible for PD;. The rest of the patients who opted for HD, live transplant and CT remained in the initial consultation. This study only shows the final result of the decision-making process and the patient's choice of one technique or another based on his or her specific values and preferences after the nursing consultation. It does not describe the start of the technique; therefore, those patients who were subsequently excluded from PD due to medical problems were not considered.12 In the center analyzed, the possibility of choosing home HD was not available.
VariablesDemographic and clinical data were obtained from the electronic medical records of the reference center. The variables considered for the study were: age, sex, etiology of CKD, level of dependence for basic activities of daily living (Barthel scale) and instrumental activities of daily living (Lawton and Brody scale), nationality (Spanish vs. foreign), socioeconomic level and language barrier (those patients with communication difficulties due to not speaking or understanding the language).
Other variables recorded were GFR on arrival at the ACKD clinic and whether they were potentially transplantable according to the nephrologist's opinion.
Measuring instrumentsBarthel scaleThe Barthel scale13 explores whether there is independence for basic activities of daily living. There are 10 activities included in the original index: eating, transferring between chair and bed, personal grooming, toileting, bathing or showering, moving (walking on a smooth surface or in a wheelchair), climbing or descending stairs, dressing or undressing, stool control and urine control. The range of possible values for the Barthel scale is between 0 and 100, with 5-point intervals for the original version. The closer a subject's score is to 0, the more dependent he or she is, and the closer it is to 100, the more independent. This information is obtained by directly asking the individual or his or her primary caregiver.
Lawton and Brody scaleThe Lawton and Brody scale14 explores instrumental activities of daily living. Activities included are: using the telephone, shopping, food preparation, cleaning, washing, traveling, taking medications, and managing finances. Each item can have a numerical value from 1 (independent) to 0 (dependent). The final score is the sum of the value of all responses and ranges from 0 (maximum dependence) to 8 (total independence). This information is obtained by directly asking the individual or his or her primary caregiver.
Assessment of socioeconomic levelThe socioeconomic level was extrapolated according to home residence and health district of primary care center to which the patient belongs. Primary care centers were classified according to their corresponding district to obtain the total number of cases per district. The most recent information (2017) on the average income of the health districts was extracted from official data provided by the Barcelona City Council.15 The estimate used was the per capita household income, which considers the income available for consumption and the accumulated savings per person. Subsequently, and with the aim of simplifying the analysis, we summarized and grouped the scores according to the socioeconomic level of the district in which they live.16 In this way, patients were classified into 3 socioeconomic level groups: low, medium-low and medium-high.
Statistical analysisNumerical variables were described as mean and standard deviation, while categorical variables were shown as the number and percentage of subjects. Comparisons between groups were performed with Student's t-test for continuous variables and the chi-square test for categorical variables. Multivariate analysis was also performed using binary logistic regression to assess which factors were independently associated with decision making and the choice between HD and PD. In the multivariate analysis, the dependent variable was PD versus HD and the variables included in the model were age, sex, diabetic nephropathy, GFR at the start of ACKD, socioeconomic level, nationality, language barrier, Barthel index, Lawton and Brody index, and candidacy for RT. All statistical analyses were performed using the R statistical package version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria).
Ethical considerationsThis analysis followed the regulations of the European Union law on data protection and privacy for all individuals within the European Union (GDPR/2018), and the Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects.
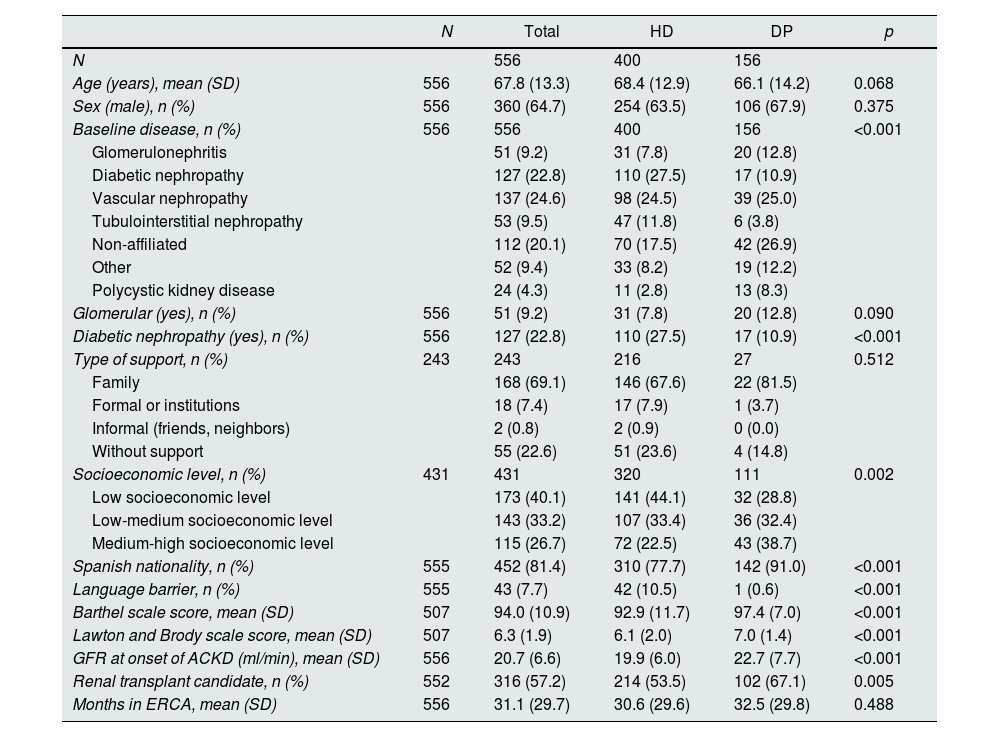
ResultsA total of 673 persons with stage 4 or 5 CKD were seen in the ACKD clinic during the study period, of whom 400 (59.4%) opted for HD, 156 (23.1%) for PD, 4 (0.5%) for live RT and 113 (16.7%) for CT. Table 1 shows the comparison between the persons who chose the 2 dialysis modalities (HD at the center vs. PD) and the the sociodemographic factors associated with the choice of the different treatments. The choice of PD as the RRT technique (vs. HD) was associated with a medium-high socioeconomic level (38.7 vs. 22.5%; p = 0.002), Spanish nationality (91 vs. 77.7%; p < 0.001) and a lower language difficulty (0.6 vs. 10.5%; p < 0.001), as well as with a higher score on the Barthel scale (greater independence in basic activities of daily living) (97.4 vs. 92.9) and on the Lawton and Brody scale (greater independence in instrumental activities of daily living) (7 vs 6.1; p < 0.001). Neither age nor sex showed significant differences in the choice of both techniques.The proportion of potentially transplantable persons was higher in the group that chose PD vs. HD (67.1 vs. 53.5%; p = 0.005). Those who chose PD had a significantly higher GFR than those who opted for HD at the time when the technique was chosen (22.7 vs. 19.9 ml/min; p < 0.001) (Table 1).
Sociodemographic factors associated with the choice of a modality of renal replacement therapy (hemodialysis versus peritoneal dialysis) in ACKD.
| N | Total | HD | DP | p | |
|---|---|---|---|---|---|
| N | 556 | 400 | 156 | ||
| Age (years), mean (SD) | 556 | 67.8 (13.3) | 68.4 (12.9) | 66.1 (14.2) | 0.068 |
| Sex (male), n (%) | 556 | 360 (64.7) | 254 (63.5) | 106 (67.9) | 0.375 |
| Baseline disease, n (%) | 556 | 556 | 400 | 156 | <0.001 |
| Glomerulonephritis | 51 (9.2) | 31 (7.8) | 20 (12.8) | ||
| Diabetic nephropathy | 127 (22.8) | 110 (27.5) | 17 (10.9) | ||
| Vascular nephropathy | 137 (24.6) | 98 (24.5) | 39 (25.0) | ||
| Tubulointerstitial nephropathy | 53 (9.5) | 47 (11.8) | 6 (3.8) | ||
| Non-affiliated | 112 (20.1) | 70 (17.5) | 42 (26.9) | ||
| Other | 52 (9.4) | 33 (8.2) | 19 (12.2) | ||
| Polycystic kidney disease | 24 (4.3) | 11 (2.8) | 13 (8.3) | ||
| Glomerular (yes), n (%) | 556 | 51 (9.2) | 31 (7.8) | 20 (12.8) | 0.090 |
| Diabetic nephropathy (yes), n (%) | 556 | 127 (22.8) | 110 (27.5) | 17 (10.9) | <0.001 |
| Type of support, n (%) | 243 | 243 | 216 | 27 | 0.512 |
| Family | 168 (69.1) | 146 (67.6) | 22 (81.5) | ||
| Formal or institutions | 18 (7.4) | 17 (7.9) | 1 (3.7) | ||
| Informal (friends, neighbors) | 2 (0.8) | 2 (0.9) | 0 (0.0) | ||
| Without support | 55 (22.6) | 51 (23.6) | 4 (14.8) | ||
| Socioeconomic level, n (%) | 431 | 431 | 320 | 111 | 0.002 |
| Low socioeconomic level | 173 (40.1) | 141 (44.1) | 32 (28.8) | ||
| Low-medium socioeconomic level | 143 (33.2) | 107 (33.4) | 36 (32.4) | ||
| Medium-high socioeconomic level | 115 (26.7) | 72 (22.5) | 43 (38.7) | ||
| Spanish nationality, n (%) | 555 | 452 (81.4) | 310 (77.7) | 142 (91.0) | <0.001 |
| Language barrier, n (%) | 555 | 43 (7.7) | 42 (10.5) | 1 (0.6) | <0.001 |
| Barthel scale score, mean (SD) | 507 | 94.0 (10.9) | 92.9 (11.7) | 97.4 (7.0) | <0.001 |
| Lawton and Brody scale score, mean (SD) | 507 | 6.3 (1.9) | 6.1 (2.0) | 7.0 (1.4) | <0.001 |
| GFR at onset of ACKD (ml/min), mean (SD) | 556 | 20.7 (6.6) | 19.9 (6.0) | 22.7 (7.7) | <0.001 |
| Renal transplant candidate, n (%) | 552 | 316 (57.2) | 214 (53.5) | 102 (67.1) | 0.005 |
| Months in ERCA, mean (SD) | 556 | 31.1 (29.7) | 30.6 (29.6) | 32.5 (29.8) | 0.488 |
Patients who chose conservative treatment and those who chose live transplantation were excluded.
ACKD: advanced chronic kidney disease; GFR: glomerular filtration rate (ml/min); PD: peritoneal dialysis; HD: hemodialysis; SD: standard deviation.
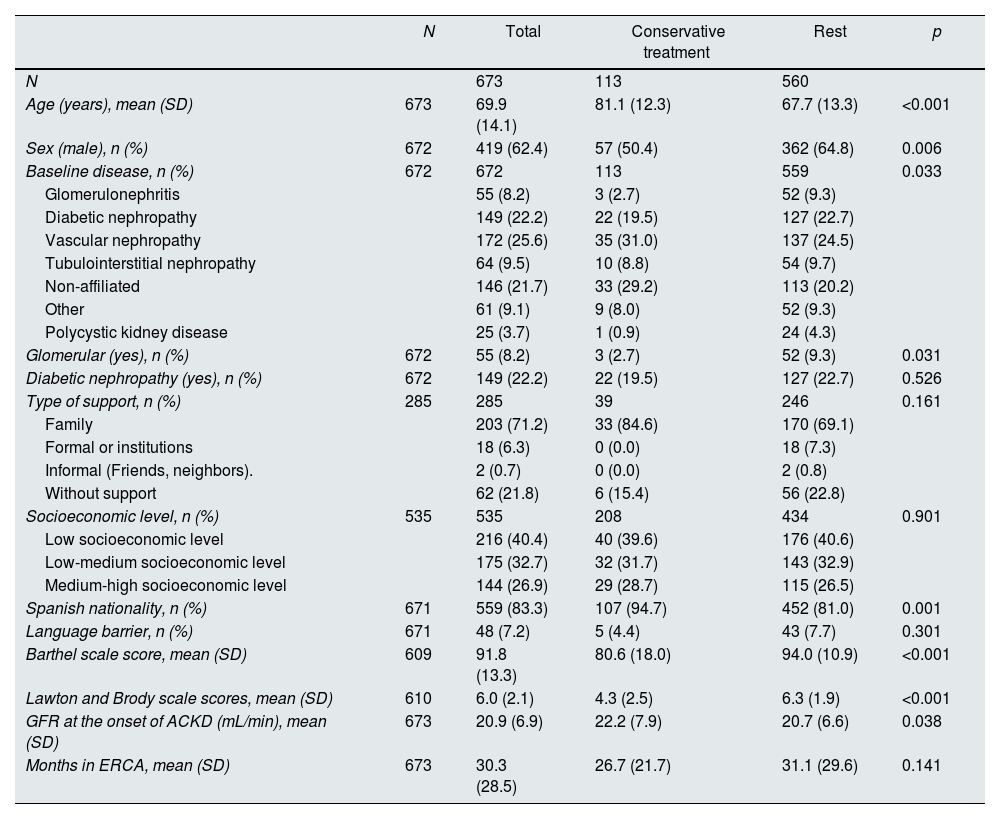
Table 2 shows the comparison between patients who chose CT vs. the rest who chose some dialytic technique as their RRT modality. Patients who opted for CT were significantly older (81.1 vs. 67.7 years; p < 0.001), more dependent (p < 0.001), with a higher proportion of women (49.6 vs. 35.2%; p = 0.006) and of Spanish nationality (94.7 vs. 81%; p = 0.001), compared to those. Socioeconomic level did not influence the choice of TC.
Sociodemographic factors associated with the choice of conservative treatment modality in ACKD.
| N | Total | Conservative treatment | Rest | p | |
|---|---|---|---|---|---|
| N | 673 | 113 | 560 | ||
| Age (years), mean (SD) | 673 | 69.9 (14.1) | 81.1 (12.3) | 67.7 (13.3) | <0.001 |
| Sex (male), n (%) | 672 | 419 (62.4) | 57 (50.4) | 362 (64.8) | 0.006 |
| Baseline disease, n (%) | 672 | 672 | 113 | 559 | 0.033 |
| Glomerulonephritis | 55 (8.2) | 3 (2.7) | 52 (9.3) | ||
| Diabetic nephropathy | 149 (22.2) | 22 (19.5) | 127 (22.7) | ||
| Vascular nephropathy | 172 (25.6) | 35 (31.0) | 137 (24.5) | ||
| Tubulointerstitial nephropathy | 64 (9.5) | 10 (8.8) | 54 (9.7) | ||
| Non-affiliated | 146 (21.7) | 33 (29.2) | 113 (20.2) | ||
| Other | 61 (9.1) | 9 (8.0) | 52 (9.3) | ||
| Polycystic kidney disease | 25 (3.7) | 1 (0.9) | 24 (4.3) | ||
| Glomerular (yes), n (%) | 672 | 55 (8.2) | 3 (2.7) | 52 (9.3) | 0.031 |
| Diabetic nephropathy (yes), n (%) | 672 | 149 (22.2) | 22 (19.5) | 127 (22.7) | 0.526 |
| Type of support, n (%) | 285 | 285 | 39 | 246 | 0.161 |
| Family | 203 (71.2) | 33 (84.6) | 170 (69.1) | ||
| Formal or institutions | 18 (6.3) | 0 (0.0) | 18 (7.3) | ||
| Informal (Friends, neighbors). | 2 (0.7) | 0 (0.0) | 2 (0.8) | ||
| Without support | 62 (21.8) | 6 (15.4) | 56 (22.8) | ||
| Socioeconomic level, n (%) | 535 | 535 | 208 | 434 | 0.901 |
| Low socioeconomic level | 216 (40.4) | 40 (39.6) | 176 (40.6) | ||
| Low-medium socioeconomic level | 175 (32.7) | 32 (31.7) | 143 (32.9) | ||
| Medium-high socioeconomic level | 144 (26.9) | 29 (28.7) | 115 (26.5) | ||
| Spanish nationality, n (%) | 671 | 559 (83.3) | 107 (94.7) | 452 (81.0) | 0.001 |
| Language barrier, n (%) | 671 | 48 (7.2) | 5 (4.4) | 43 (7.7) | 0.301 |
| Barthel scale score, mean (SD) | 609 | 91.8 (13.3) | 80.6 (18.0) | 94.0 (10.9) | <0.001 |
| Lawton and Brody scale scores, mean (SD) | 610 | 6.0 (2.1) | 4.3 (2.5) | 6.3 (1.9) | <0.001 |
| GFR at the onset of ACKD (mL/min), mean (SD) | 673 | 20.9 (6.9) | 22.2 (7.9) | 20.7 (6.6) | 0.038 |
| Months in ERCA, mean (SD) | 673 | 30.3 (28.5) | 26.7 (21.7) | 31.1 (29.6) | 0.141 |
ACKD. advanced chronic kidney disease; GFR: glomerular filtration rate (ml/min); SD: standard deviation; GFR: glomerular filtration rate (ml/min).
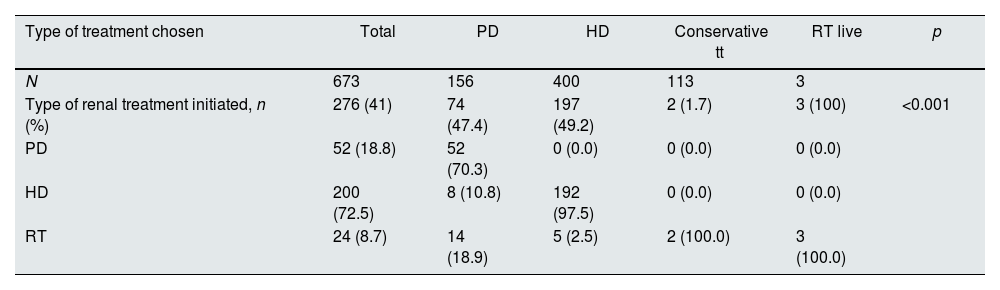
Table 3 shows the techniques chosen compared to the techniques with which they started treatment.
Comparison of type of treatment initiated by patients vs. treatment chosen (N = 397).
| Type of treatment chosen | Total | PD | HD | Conservative tt | RT live | p |
|---|---|---|---|---|---|---|
| N | 673 | 156 | 400 | 113 | 3 | |
| Type of renal treatment initiated, n (%) | 276 (41) | 74 (47.4) | 197 (49.2) | 2 (1.7) | 3 (100) | <0.001 |
| PD | 52 (18.8) | 52 (70.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| HD | 200 (72.5) | 8 (10.8) | 192 (97.5) | 0 (0.0) | 0 (0.0) | |
| RT | 24 (8.7) | 14 (18.9) | 5 (2.5) | 2 (100.0) | 3 (100.0) |
Patients who died, were lost in consultation, transferred or were still active in the advanced chronic kidney disease clinic at the time of analysis are not included.
PD: peritoneal dialysis; HD: hemodialysis; RT: renal transplantation; tt: treatment.
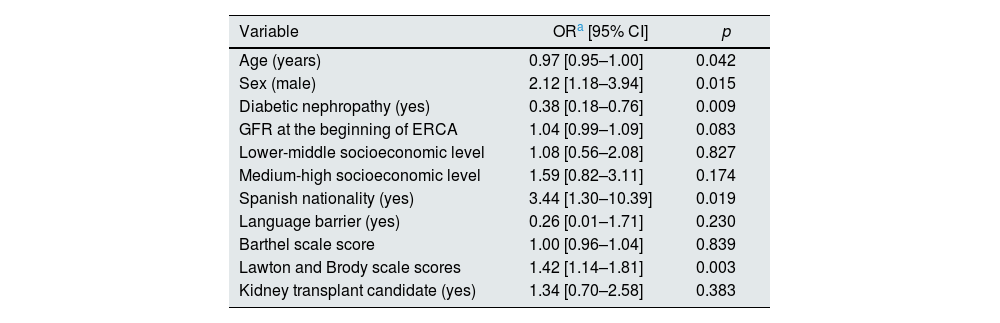
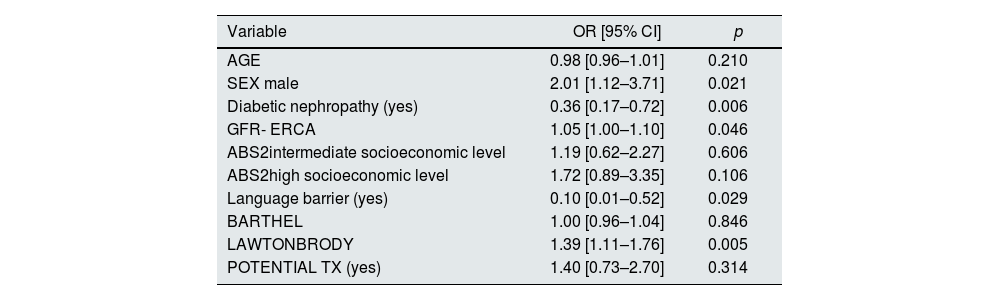
In view of the possibility that variables such as nationality and language barrier were related to each other, 2 multivariate analyses were performed: one including nationality and the other excluding it. This analysis showed that male sex, diabetic nephropathy, Spanish nationality, and greater independence in instrumental activities of daily living were associated with the choice of PD independently of the rest of the variables (Table 4). Once nationality was excluded, the language barrier was independently associated with the choice of HD versus PD (Table 5).
Multivariate analysis of the choice of peritoneal dialysis versus hemodialysis (binary logistic regression).
| Variable | ORa [95% CI] | p |
|---|---|---|
| Age (years) | 0.97 [0.95–1.00] | 0.042 |
| Sex (male) | 2.12 [1.18–3.94] | 0.015 |
| Diabetic nephropathy (yes) | 0.38 [0.18–0.76] | 0.009 |
| GFR at the beginning of ERCA | 1.04 [0.99–1.09] | 0.083 |
| Lower-middle socioeconomic level | 1.08 [0.56–2.08] | 0.827 |
| Medium-high socioeconomic level | 1.59 [0.82–3.11] | 0.174 |
| Spanish nationality (yes) | 3.44 [1.30–10.39] | 0.019 |
| Language barrier (yes) | 0.26 [0.01–1.71] | 0.230 |
| Barthel scale score | 1.00 [0.96–1.04] | 0.839 |
| Lawton and Brody scale scores | 1.42 [1.14–1.81] | 0.003 |
| Kidney transplant candidate (yes) | 1.34 [0.70–2.58] | 0.383 |
Number of patients included in the analysis: 390 (83 peritoneal dialysis and 307 hemodialysis).
Spanish nationality were considered to have no language barrier.
ACKD: advanced chronic kidney disease; CI: confidence interval; GFR: glomerular filtration rate (ml/min); OR: odds ratio; SD: standard deviation.
Multivariate analysis of the choice of peritoneal dialysis versus hemodialysis (binary logistic regression), excluding nationality.
| Variable | OR [95% CI] | p |
|---|---|---|
| AGE | 0.98 [0.96–1.01] | 0.210 |
| SEX male | 2.01 [1.12–3.71] | 0.021 |
| Diabetic nephropathy (yes) | 0.36 [0.17–0.72] | 0.006 |
| GFR- ERCA | 1.05 [1.00–1.10] | 0.046 |
| ABS2intermediate socioeconomic level | 1.19 [0.62–2.27] | 0.606 |
| ABS2high socioeconomic level | 1.72 [0.89–3.35] | 0.106 |
| Language barrier (yes) | 0.10 [0.01–0.52] | 0.029 |
| BARTHEL | 1.00 [0.96–1.04] | 0.846 |
| LAWTONBRODY | 1.39 [1.11–1.76] | 0.005 |
| POTENTIAL TX (yes) | 1.40 [0.73–2.70] | 0.314 |
Number of patients included in the analysis: 390.
Spanish nationals were considered to have no language barrier.
CI, confidence interval; OR, odds ratio.
The main finding of this study is that in people living in areas with a high socioeconomic level, Spanish nationality, a higher level of independence in basic and instrumental activities of daily living, and the no existence of a language barrier favor the choice of PD over HD in the center, while age, sex, and degree of dependence favor the choice of CT. In the multivariate analysis, male sex, Spanish nationality and greater independence in instrumental activities of daily living are independent variables that favor the choice of PD, and having diabetic nephropathy favored the choice of in-center HD.
These results show that some variables, such as nationality and language barrier, are related to each other; foreign patients have a greater probability of presenting a language barrier, which is why this is no longer significant in the multivariate model that includes nationality; the case with socioeconomic level is similar, Its inclusion in the multivariate model does not improve prediction because nationality is probably correlated with socioeconomic level. Excluding nationality in the model shows that the language barrier is independently associated with the choice of HD versus PD.
These findings confirm the known higher incidence, prevalence, progression and complications and lower survival of CKD in socioeconomically disadvantaged populations.17–19 In relation to the choice of RRT technique, a reduced utilization of PD has been described in areas with low resources.20 Only one study conducted in Australia showed more likelihood of using HD at the center by patients from more economically advantaged areas.21 Although there are studies that help to understand the influence of socioeconomic gradients on health status, adequate policies to reduce these inequalities have not yet been developed.22 To exercise true person-centered care and equity in decision making, additional interventions that address patients' knowledge, education, attitudes, motivations, skills and resources should be supported, and where identified deficits are specifically addressed, with interdisciplinary teams that include social workers.23
Another finding of this study is the association between migrants and/or people with a language barrier and the choice of in-center HD versus PD. It has been argued that the underutilization of home dialysis by racial/ethnic minorities24 cannot be explained solely by differences in age and health status.25 There are barriers, such as differences in language, religion, lower levels of health literacy, or less access to health care services and information,26 that could give rise to these disparities. The language barrier can increase vulnerability in hospital care and creates a gap in the freedom of choice of these individuals. Therefore, personalized interventions to overcome these barriers should be implemented in the process of making decisions about the modality of RRT in order to achieve equitable, free and tailored decision-making.27,28
Traditionally, functional and/or psychological dependence has restricted the use of home therapies. In this study, a higher level of dependency favors the choice of in-center HD over PD. The incorporation of assisted PD programs could be an alternative to in-center HD for people with a higher degree of dependency who choose this technique, in whom a better health-related quality of life has been demonstrated.29
In relation to the choice of CT, the results obtained are the same as those reported in the reference literature,30,31 highlighting that the persons who opted for this alternative were significantly older, had greater functional deterioration and there was a greater predominance of women (50%) than in the group that chose to undergo RRT (30%). Sex has been described as a cause of inequity in health care, sometimes due to biological factors (sex) and other times due to cultural factors (gender). Qualitative studies would be necessary to study these gender differences in the choice of technique in greater depth.
This study has several limitations, such as the observational/retrospective nature of the analysis, the fact that it involves a single center, the lack of home hemodialysis among the techniques offered, the absence of data on comorbidity and social support, and the cross-sectional design, which means that the results are limited to associations and not causality. Although there is a possibility that the mean income of health districts differs from the personal income of one individual patient, it is a proxy measure and widely used.15,16 Future studies should analyze the socioeconomic circumstances of this population on an individualized basis (contributory pensions, non-contributory pensions, no pensions, etc.).
In addition, some factors that have been related to the choice of RRT in ACKD have not been considered, such as the degree of comorbidity, coping capacity, frailty, modality adjustment with lifestyle, distance to the center, level of education, and verbal and written information on the modality.32 These limitations should be balanced with the strengths of this study, which includes a cohort of patients in ACKD that evaluates for the first time in our country the influence of sociodemographic factors on the choice of technique.
In conclusion, the findings obtained indicate that although the decision-making process is described and regulated, there are factors, often not taken into account, that can affect equity in the choice of RRT modality. Taking into account the socioeconomic, cultural and dependency needs of the population we serve it is increasingly necessary to effectively reduce health inequities. It is necessary to address the states of vulnerability that affect RRT options. Achieving this imperative requires an intersectoral and multilevel intervention, i.e., with intervention of the Third Sector of Social Action and the competent public administrations, including hospital network, primary through case managers and socio-health network), with interdisciplinary teams that include, among others, social workers, in order to identify specific needs, review available governmental aid and the processing of the same adapted to the need, to provide a holistic and person-centered assessment.
FinancingThis manuscript has not received any funding.
Conflict of interestThe authors declare that they have no conflicts of interest.