Introducción: La determinación periódica del flujo sanguíneo (QA) es el método de elección para monitorizar la fístula arteriovenosa (FAVI) de los pacientes en hemodiálisis (HD) crónica. Objetivos: 1) Valorar la eficacia de la técnica de gradiente de temperatura (TGT) en la determinación de QA utilizando el dispositivo Twister® y comparar los resultados funcionales con el método Delta-H. 2) Analizar el efecto de la presión arterial sobre la función de la FAVI. Pacientes y método: Hemos determinado no invasivamente el QA de 30 FAVI (24 radial y 6 humeral; duración media 53,4 ± 78,5 meses) en 30 pacientes (edad media: 59,9 ± 14,1 años; sexo H: 60%, M: 40%; tiempo medio en HD: 37,4 ± 40,6 meses; nefropatía diabética: 20%) estables durante la HD mediante la TGT, descrita y validada por Wijnen et al. (Kidney Int 2007;72:736). El QA se calculó a partir de los valores de temperatura obtenidos mediante el monitor de temperatura sanguínea BTM, integrado en la máquina Fresenius Medical Care 4008-S, con las líneas sanguíneas de HD en configuración normal e invertida, y sin la necesidad de generar un bolus de temperatura. El dispositivo Twister® se utilizó para revertir las líneas sanguíneas sin necesidad de desconectarlas de las agujas ni de detener la bomba sanguínea. El QA se determinó durante la primera hora de 2 sesiones consecutivas de HD (ambos valores se promediaron). La presión arterial media (PAM) (presión diastólica + 1/3 de la presión del pulso) se calculó simultáneamente con el QA. Paralelamente, el flujo sanguíneo de la FAVI se determinó durante la misma semana en todos los pacientes mediante el método Delta-H utilizando el monitor Crit-Line III (HemaMetrics, USA) durante la HD (inversión manual de las líneas). Resultados: El QA medio fue 1132,5 ± 515,4 ml/min (intervalo, 446-2233 ml/min). El coeficiente de variación para medidas duplicadas de QA fue 6,8 ± 4,7%; la PAM no influyó en la reproductibilidad de la TGT (96,1 ± 13,7 vs. 96,6 ± 12,8 mmHg, p = 0,72). Sin diferencias al comparar el QA de pacientes diabéticos (n = 6, 966,4 ± 340,7 ml/min) y no diabéticos (n = 24, 1174,4 ± 548,3 ml/min) (p = 0,39). El QA fue similar tanto para los pacientes con PAM < 100 mmHg (n = 18, 1101,0 ± 552,7 ml/min) como para los pacientes con PAM ≥ 100 mmHg (n = 12, 1180,4 ± 473,3 ml/min) (p = 0,69). No hemos objetivado ninguna correlación entre el QA medio y: edad (r = 0,09, p = 0,62), tiempo en HD (r = 0,06, p = 0,76), PAM (r = –0,21, p = 0,27), índice Kt/V (r = 0,12, p = 0,51), distancia entre las agujas (r = –0,17, p = 0,37) y duración de la FAVI (r = –0,01, p = 0,96). El tiempo medio empleado para determinar el QA por la TGT utilizando el accesorio Twister® (5,9 ± 1,9 min) fue significativamente inferior en relación con el método Delta-H (26,8 ± 1,9 min) o con la TGT (n = 35, 8,9 ± 3,5 min, inversión manual de las líneas) aplicada por Wijnen et al. (Kidney Int 2007;72:736) (para ambas comparaciones, p < 0,001). El QA medio obtenido mediante la TGT fue similar al flujo sanguíneo medio determinado con el método Delta-H (1138,4 ± 502,3 ml/min) (p = 0,83). Los valores del flujo sanguíneo de la FAVI obtenidos mediante la TGT se correlacionaron significativamente con los determinados por el método Delta-H (r = 0,963, p < 0,001). Conclusiones: 1) La TGT es un método válido y reproducible para calcular el QA durante la HD. 2) El dispositivo Twister® es eficaz para reducir el tiempo empleado en determinar el QA mediante la TGT. 3) Los valores de flujo sanguíneo de la FAVI obtenidos mediante la TGT y el método Delta-H se correlacionaron significativamente. 4) Se ha evidenciado una independencia entre la función de la FAVI y la presión arterial del paciente.
Introduction. Periodic blood flow (QA) measurement is the preferred way for arteriovenous fistula (AVF) surveillance in chronic hemodialysis (HD) patients. Objectives. 1) Assess the efficacy of the temperature gradient method (TGM) on the QA determinations using the Twister™ device and to compare the functional results with the Delta-H method. 2) Evaluate the effect of blood pressure on the AVF function. Patients and method. We measured the QA non invasively in 30 AVF (24 radial and 6 brachial; mean duration 53.4 ± 78.5 months) during HD in 30 stable patients (mean age 59.9 ± 14.1 years, males 60 %, females 40 %; mean time on HD 37.4 ± 40.6 months, diabetic nephropathy 20 %) by the TGM, described and validated by Wijnen et al (Kidney Int 2007;72:736). The QA was calculated from the temperature values obtained by means of the blood temperature monitor (BTM), integrated into the Fresenius Medical Care 4008-S machine, at normal and reverse configurations of the HD blood lines, with no need for a thermal bolus. The Twister™ device was used for reversing the blood lines without the need to disconnect them from the AVF lines nor to stop the blood pump. The QA was measured within the first hour of two consecutive HD sessions (the values were averaged). The mean arterial pressure MAP (diastolic pressure + 1/3 pulse pressure) was calculated simultaneous with the QA. In addition, the AVF blood flow was also determined during the same week in all patients by the Delta-H method using the Crit-Line III Monitor (ABF-mode, HemaMetrics, USA) during HD (manually switching lines). Results. The mean QA was 1132.5 ± 515.4 ml/min (range, 446-2233 ml/min). The mean coefficient of variation for duplicate QA measurements was 6.8 ± 4.7 %; the MAP was not different when the reproducibility tests were performed (96.1 ± 13.7 versus 96.6 ±12.8 mmHg, p = .72). No significant difference was found when comparing the mean QA between diabetic (n = 6, 966.4 ± 340.7 ml/min) and nondiabetic (n = 24, 1174.4 ± 548.3 ml/min) patients (p = .39). The mean QA was similar for patients with mean MAP < 100 mmHg (n = 18, 1101.0 ± 552.7 ml/min) and for patients with mean MAP >_ 100 mmHg (n = 12, 1180.4 ± 473.3 ml/min) (p = .69). No correlation was found between the mean QA and: age (r = 0.09, p = .62), time on HD (r = 0.06, p = .76), MAP (r = – 0.21, p = .27), Kt/V index (r = 0.12, p = .51), distance between needles (r = – 0.17, p = .37) and AVF duration (r = – 0.01, p = .96). The mean time required to measure QA with the TGM using the Twister™ device (5.9 ± 1.9 min) was significantly shorter compared with the Delta-H technique (26.8 ± 1.9 min) or with the TGM (n = 35, 8.9 ± 3.5 min, manually reversing lines) reported by Wijnen et al (Kidney Int 2007;72:736).) (for both comparisons, p < .001). The mean QA obtained by the TGM was not different when compared to mean ABF determined by the Delta-H method (1138.4 ± 502.3 ml/min) (p=.83).The calculated values of AVF blood flow obtained by TGM were highly correlated with those determined by the Delta-H technique (r = 0.963, p < .001). Conclusions. 1) The TGM is a valuable and reproducible indicator of QA during HD. 2) The Twister™ device is useful to reduce the time for QA measurement by the TGM. 3) The AVF blood flow values obtained by the TGM and the Delta-H technique correlated highly with each other. 4) It has been shown the lack of relationship between the AVF function and the patient’s blood pressure.
Thrombosis is the most common complication in permanent vascular accesses (VA) such as arteriovenous fistulas (AVF) and polytetrafluoroethylene grafts.1 To prevent it and therefore reduce catheter use among prevalent patients on chronic haemodialysis (HD), we must develop structured programmes for VA surveillance in the HD units.2 In addition to addressing non-anatomical causes of thrombosis, these programmes consider the use of different screening methods for early diagnosis of significant VA stenoses associated with elective corrective procedures such as angioplasty and/or revision surgery.1-3
According to the latest version of the KDOQI guidelines, non-invasive screening methods based on indirect measurement of the VA blood flow (QA) are the methods of choice for regular VA surveillance.1 Since 1995, it have been described several of these methods and some of them have subsequently applied in daily clinical practice, such as ultrasound dilution, Delta-H or termodilución.4 Some Some of these techniques have been proven effective in providing an early diagnosis of significant stenosis and reducing the rate of VA thrombosis.5,6
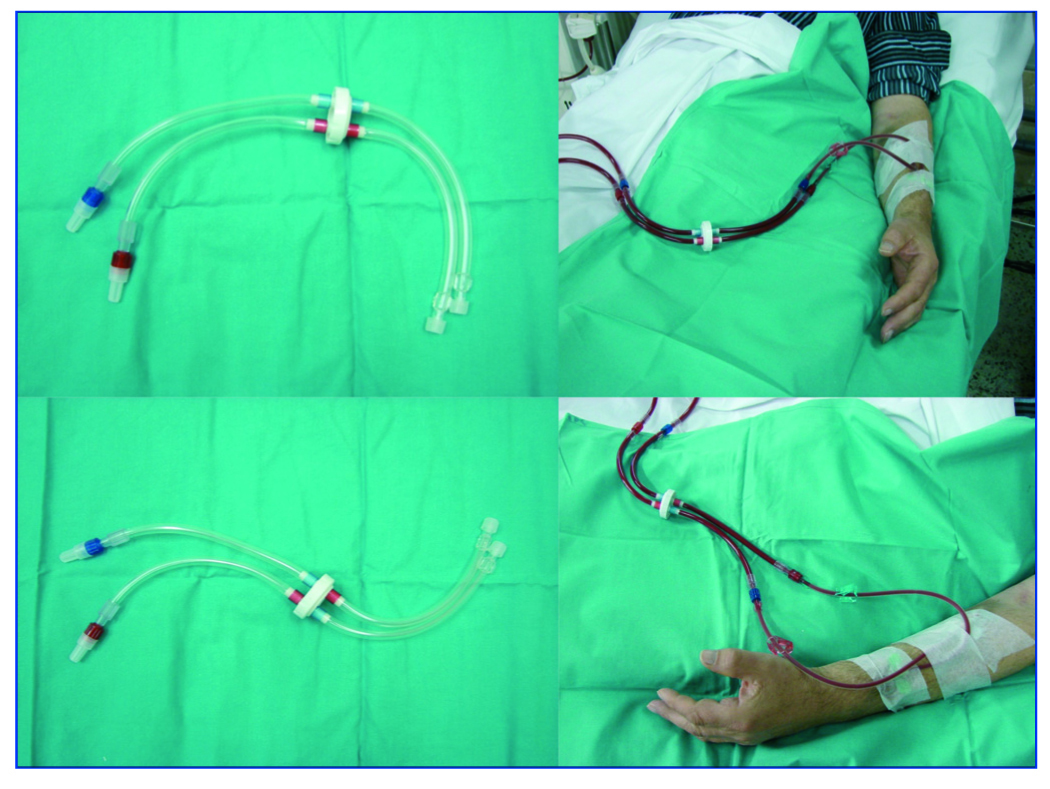
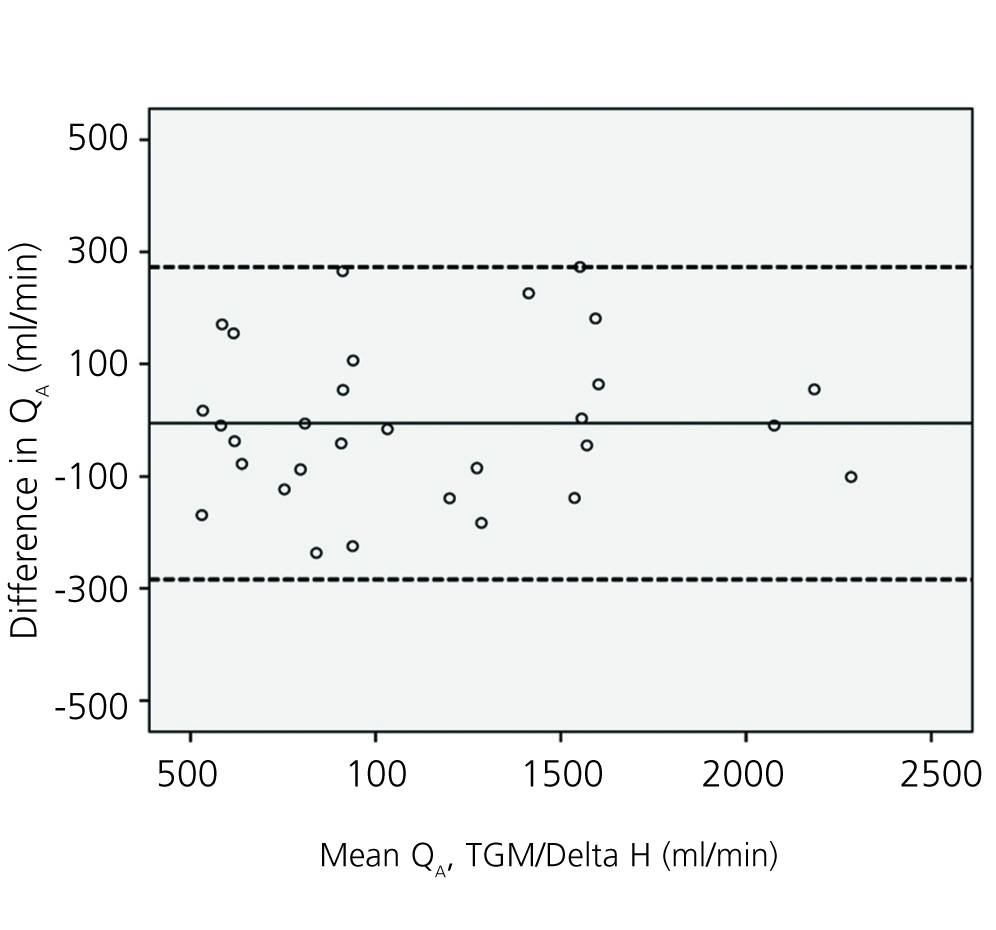
The temperature gradient method (TGM) was described and validated by Wijnen et al in 2007 by comparison against the ultrasound dilution method.7 This method allows us to calculate the QA from the temperature values obtained by means of the blood temperature monitor (BTM) with the HD blood lines in the normal and reversed positions.7 The use of a specialised device named Twister™ (Fresenius Medical Care), which is placed between the HD needles and the blood lines, can simplify the QA determination by shortening the time needed to reverse the HD blood lines (Figure 1).
On the other hand, no reliable study on VA function can overlook a variable as important as the patient’s blood pressure. In this regard, some authors have highlighted the direct relationship between the mean arterial pressure (MAP) and the QA of the VA, meaning that changes in the MAP can affect the VA function.8,9
This is an observational, cross-sectional, comparative study of the TGM with the following objectives:
1) Evaluate TGM efficacy in measuring the QA at the AVF during HD.
2) Determine whether placement of the TwisterTM shortens the time needed to determine QA.
3) Undertake a comparative functional study of TGM and the Delta-H method.
4) Analyse the effect of blood pressure on AVF function.
MATERIAL AND METHOD
Patients
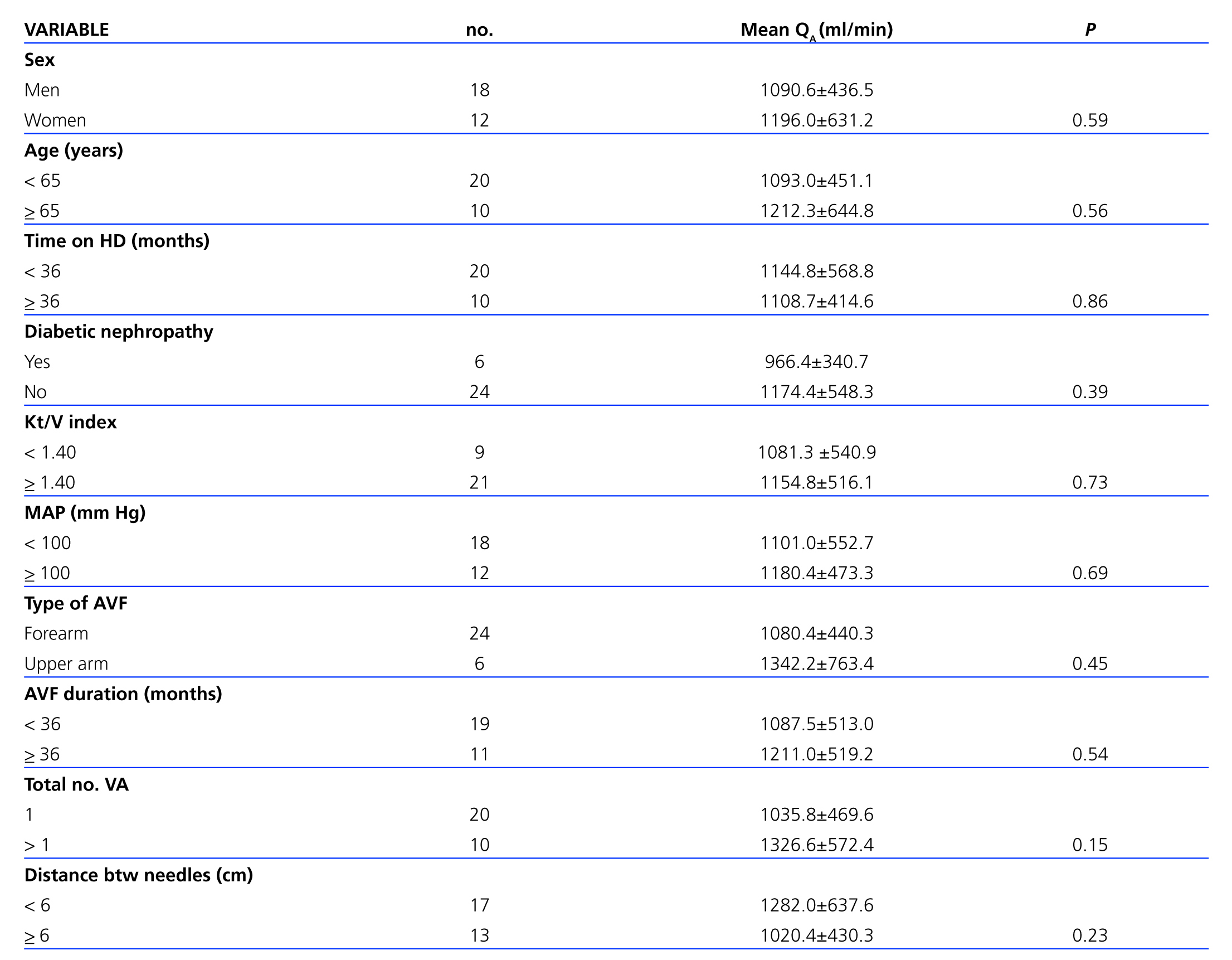
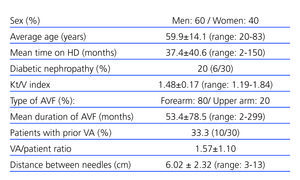
The AVF was evaluated in 30 patients undergoing HD 3 times weekly in the Nephrology Department at Hospital de Mollet. Inclusion criteria for patients were as follows: 1) Age >18 years. 2) In chronic HD programme. 3) Use of the AVF as a permanent VA. 4) Puncture of the AVF with 2 needles during a minimum of 12 consecutive HD sessions. 5) Use of a QB greater than 250ml/min during a minimum of 12 consecutive HD sessions. 6) Informed consent from the patient. The following variables were analysed: sex, age, time on HD, diabetic nephropathy as a cause of renal failure, Kt/V index (by Daugirdas second-generation single-pool model), MAP (diastolic blood pressure +1/3 pulse pressure), type of AVF, duration of AVF, total number of VA and distance between needles. Table 1 summarises the most important clinical characteristics of the patients included in the study.
Method
1) Measuring the QA by means of TGM. The QA was measured by using the BTM sensor incorporated in the 4008 S machine manufactured by Fresenius Medical Care. TGM allows us to calculate the QA from the temperature values obtained with the HD blood lines in the normal and reverse positions, with no need for creating a bolus of temperature. The QA was calculated using the following formula:
QA = (QB,x – UFR) · Tart,x – Tven,x / Tart,n – Tart,x
Where QB,xis the effective blood flow with blood lines in reverse position (ml/min), UFR is the ultrafiltration rate (ml/min), Tis thert,ntemperature of the arterial line with blood lines in normal position, Tart,xis the temperature of the arterial line with blood lines in reverse position, and Tven,xis the temperature of the venous line with blood lines in reverse position. To correctly calculate the QA, the QB, the UFR and the dialysate temperature (35.5ºC) must remain constant throughout the entire measurement process7. The QA was calculated twice during the first hour of 2 consecutive HD sessions, and these two values were weighed. The MAP was also measured also in both HD sessions along with the QA.
2) Twister™ device. This accessory measuring 37.5cm in length has a dial-shaped rotating mechanism in its centre. On 1 side it connects to the blood lines, and on the other side, to the 2 needles puncturing the AVF. By simply rotating the mechanism (turning the dial halfway), the blood lines reverse flow direction automatically with no need for disconnecting them from the needles or stopping the haemodialysis pump. At the end of the procedure, turning the dial once more in the opposite direction will instantly re-establish the normal flow direction of the blood lines (Figure 1).
3) Measuring the QA by the Delta-H method. During the same week, the QA was calculated using the Delta-H optodilutional method using the Crit-Line III monitor (ABF-mode, HemaMetrics, USA) in all patients. This method, described and validated by Yarar et al10 is a photometric technique based on the inverse relationship existing between volaemia and haematocrit (Hct). The QAwas also determined during the first hour of the HD session based on the changes recorded in Hct and the scheduled changes in ultrafiltration (from 0.1 to 1.8l/h) with blood lines in normal and reversed positions. Changes in Hct were registered continuously by an optical sensor coupled to a blood chamber inserted between the dialyser and the arterial line. QA was calculated using the following formula:
QA= (UF max.−UF min.) · Hct max. rev. / ¿Hct rev.−¿Hct nor.
Where UF max. is maximum ultrafiltration rate, UF min. is minimum ultrafiltration rate, Hct max. rev. is maximum Hct with blood lines in reverse position, ¿Hct rev. is the change in Hct with the lines reversed and ¿Hct nor. is the change in Hct with blood lines in normal position. Reversing the blood lines was performed manually after momentarily stopping the haemodialysis pump (the TwisterTM device was not used).
Statistical study
Statistical analysis of the data was performed using the SPSS program version 12.0 for Windows. Values were expressed as percentages or mean ± standard deviation. The mean coefficient of variation for duplicate QA measurements was calculated by averaging the quotient of the standard deviation and the mean of the two measurements taken for each patient. The comparative study between the mean QA obtained and the variables specific to both the patient and the AVF, compared 2 by 2, was performed using Student’s t-test for 2 independent samples and the nonparametric Mann-Whitney U test. Pearson’s correlation coefficient was calculated to analyse the correlation between the mean QA at the AVF and the different quantitative variables studied.
The time required to determine QA was calculated as follows, depending on the method used:
1) TGM: Time needed to record the temperature of the arterial line, which are necessary in order to calculate QA, as shown on the BTM display upon beginning the examination, with blood lines in the normal position + time needed for instant reversal of blood lines by using the TwisterTM device + time to stabilise temperature with blood lines in the reversed position (time needed in order to maintain exactly the same temperature during a minimum of 1 minute) + time to record the temperature values shown on the BTM display, which are necessary in order to calculate QA(blood lines in reverse position) + time to automatically revert blood lines to normal blood flow direction using the TwisterTM device. Unlike when the Delta-H method is used, the QA value is not obtained automatically. It must be calculated after completing the examination, using the formula described above.
2) Delta-H method: time elapsed during the first part of the examination, when the measured haematocrit values in relation to scheduled changes in ultrafiltration are automatically recorded, with blood lines in the normal position + time to stop the haemodialysis pump + time to manually invert the blood lines + time to re-start the HD pump + time elapsed during the second part of the examination, when the measured haematocrit values in relation to scheduled changes in ultrafiltration are automatically recorded with blood lines reversed + time to record the QA value displayed on the Crit-Line III monitor + time to stop the HD pump + time to manually revert the blood lines to their normal position + time to re-start the haemodialysis pump.
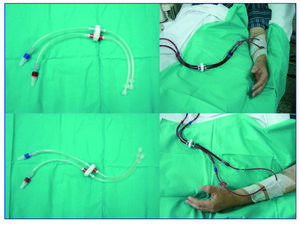
We completed a correlation analysis of the AVF blood flow values measured by Delta-H and by the TGM in the same patient sample. The Bland-Altman graph was drawn so as to provide a visual display of concordance between the two methods. Pvalues <0.05 were considered to be statistically significant.
RESULTS
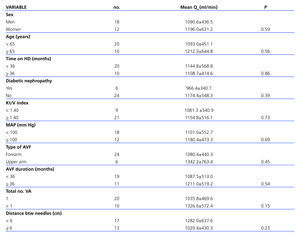
The mean QA at the AVF obtained by TGM was 1132.5±515.4ml/min (range: 446-2233ml/min). The coefficient of variation for duplicate QA measurements was 6.8±4.7%. Table 2 shows the mean values of QA and MAP measured in the 2 consecutive HD sessions. There are no differences between MAP values taken in the first and second sessions (P= not significant).
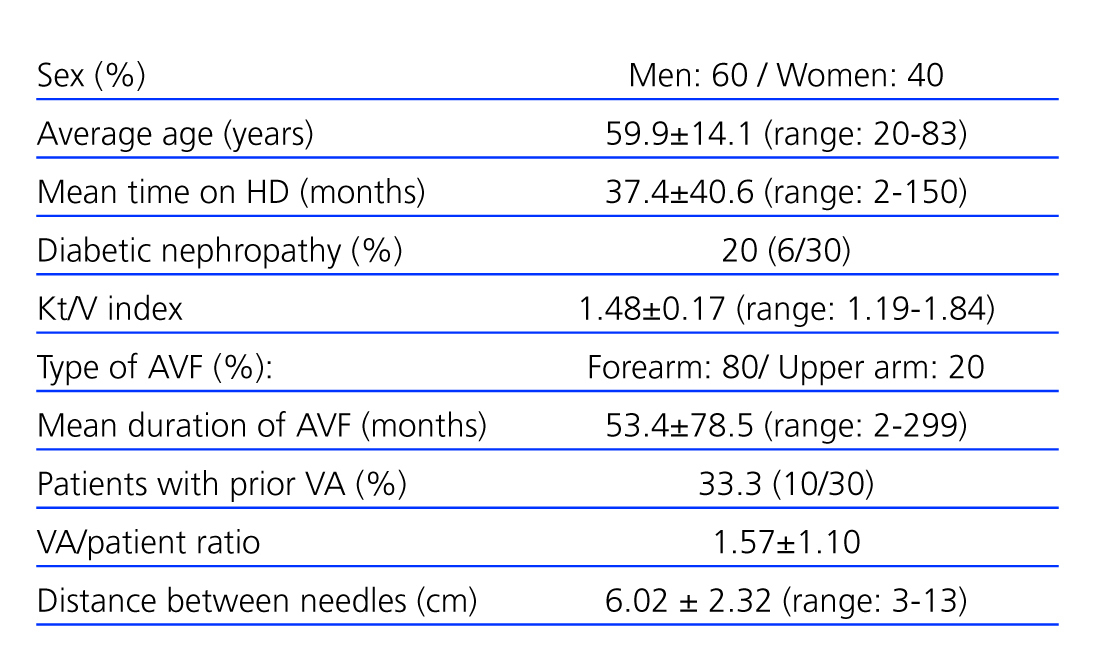
No differences were found when comparing the mean QA in relation to variables of the patient and the AVF shown in Table 3. The QA from the AVF of diabetic patients was less than 1000 ml/min, but this was not significantly different compared to the remaining patients. The mean QA was similar when comparing patients with MAP above or below 100 mmHg. The brachial AVF showed a higher mean QA than the radial AVF, but the difference was not statistically significant. We observed no correlations between mean QA and: age (r=0.09, P=.62), time on HD (r=0.06, P=.76), MAP (r=–0.21, P=.27), Kt/V index (r=0.12, P=.51), distance between needles (r=–0.17, P=.37) or AVF duration (r=–0.01, P=.96).
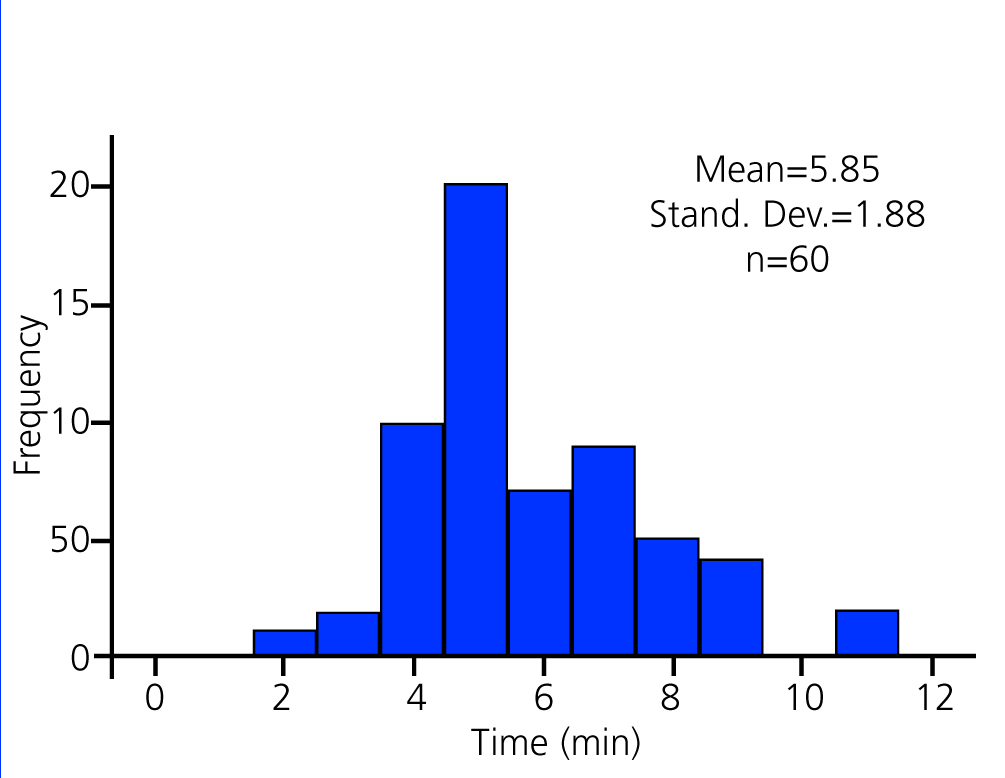
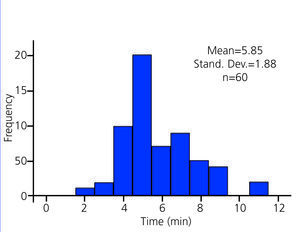
The mean time to obtain the temperature values needed to calculate the QA by the TGM using the Twister™ device, was 5.9 ± 1.9 minutes (range 2-11 minutes) and significantly lower in relation to the Delta method -H applied in this study (Table 4). As shown by the histogram in Figure 2, the time required in most cases (46/60, 76.7%) using TGM ranged between 4 and 7 minutes.
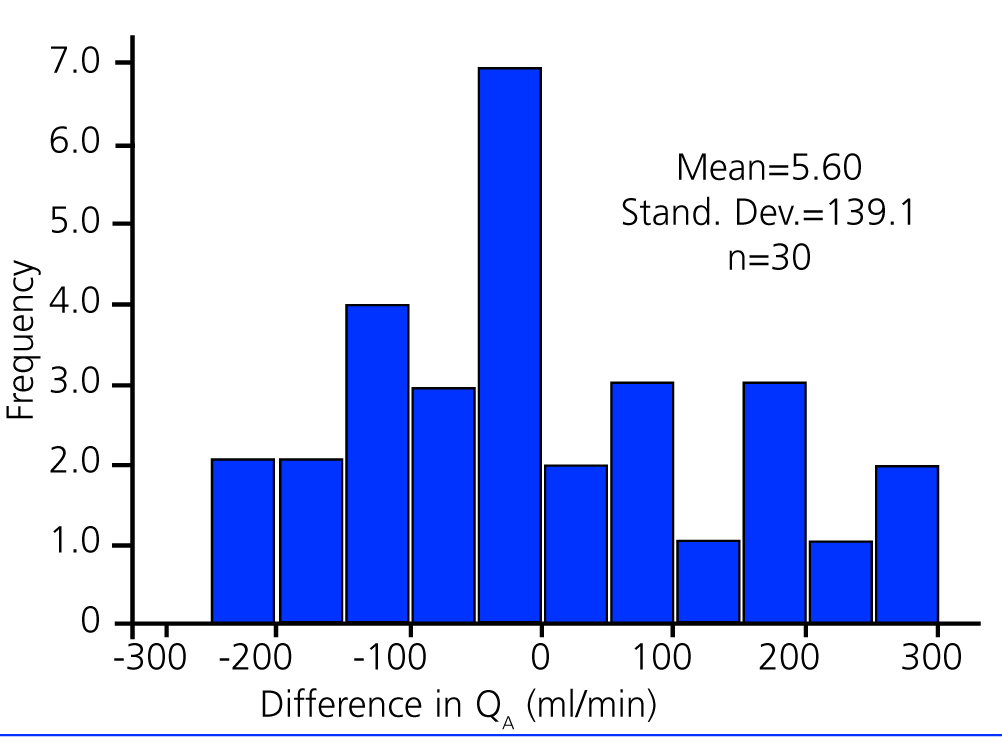
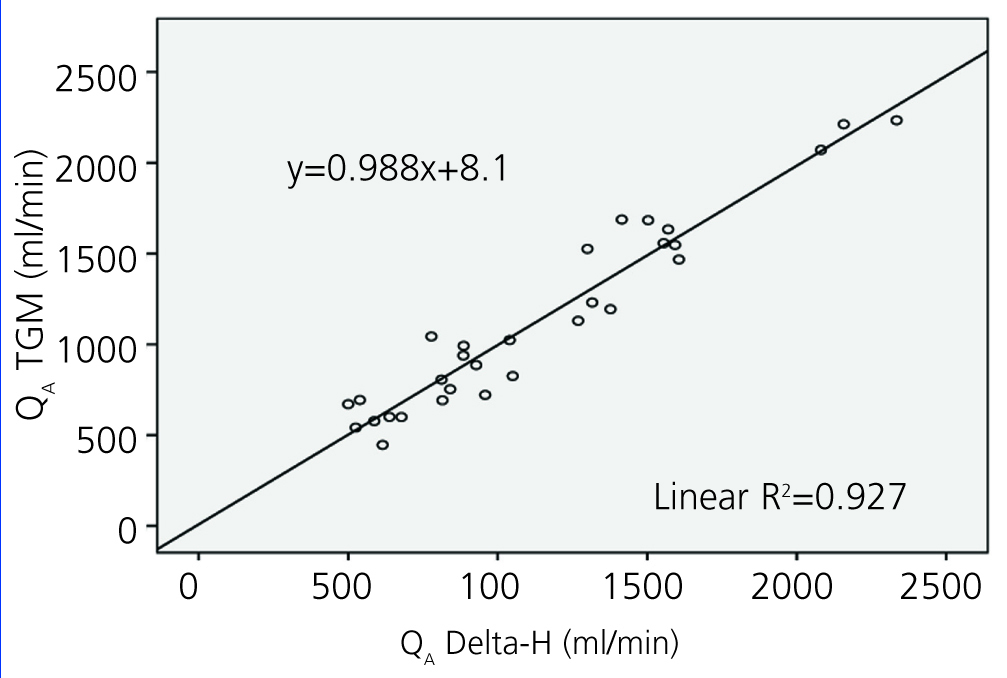
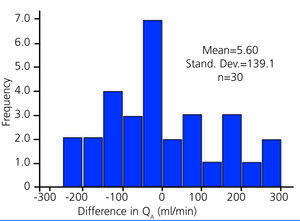
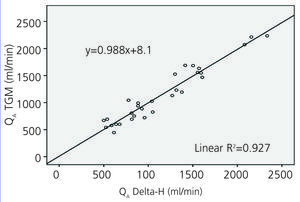
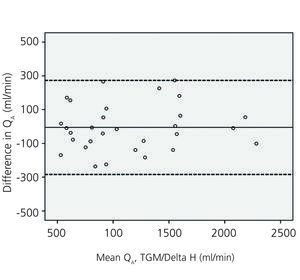
Mean QA calculated by using the TGM (1132.5±515.4ml/min) was similar to that measured using the Delta-H method (1138.4 ± 502.3ml/min) (P=.83). As shown in the histogram in Figure 3, the absolute difference between mean QA values at the AVF taken using both measurement methods was less than 150ml/min in 66.7% of the patients (20/30). Blood flow values at the AVF measured using TGM showed a significant correlation with those taken using the Delta-H method (r=0.963, P<.001) (Figure 4). The Bland-Altman graph in Figure 5 shows concordance between both screening methods, even where mean QA values are equal to or above 2000ml/min (n=3).
DISCUSSION
TGM has been proven an effective means of evaluating AVF function. The QA value obtained by TGM in this study coincides with previously reported values obtained by other non-invasive screening methods for measuring QA.3,11-15 In addition, the QA result reported in the TGM validation cohort study carried out by Wijnen et al (1000±588ml/min) is very similar to the QA calculated in our study.7
In this study, TGM demonstrated optimal reproducibility with a coefficient of variation for duplicate QA measurements of less than 10%. This result allows the TGM’s reproducibility to be compared favourably to that of other methods used in daily clinical practice, such as the Delta-H or ultrasound dilution methods.3,16
Our study found a significant functional correlation between the Delta-H method, which is routinely used in our department, and the TGM. Comparison of QA values at the AVF obtained by both methods revealed no differences. The previously mentioned cohort study by Wijnen et al also reported a significant correlation (r=0.964, P<.05) between QA values obtained using the ultrasound dilution method (mean QA 960±594ml/min) and TGM.7 Therefore, considering their efficacy in obtaining reliable QA values, the TGM and Delta-H methods are equivalent and can be used interchangeably for regular VA monitoring.
Time is money, especially when we consider the current dynamics in many HD units in Spain. Therefore, if we are to ensure the success of the VA surveillance programs, we must to apply a quick method for VA monitoring in the HD room without excessive consumption of time. In this regard, the joint application of the TGM and the Twister™ device allows to obtain the data necessary to calculate the QA of the AVF in significantly less time compared to the Delta-H method (current study) and to the methods that used the BTM to determine the QA such as the thermodilution method and the same TGM with manual switching of HD lines (Table 4).7,17
The direct relationship between the MAP and the QA of the AVF is well-known, and it is expressed as follows: QA=MAP–central venous pressure/AVF resistance18. For example, in the multivariate study from Tonelli et al including 4084 QA measurements by ultrasound dilution in 294 patients with AVF, it was observed that for each 1 mmHg of increase in systolic blood pressure, the QA increased by 1.8 and 2.9 ml/min in distal and proximal AVF, respectively19 Consequently, the results from any study examining AVF function cannot be valid unless they consider blood pressure. The current study analysed the effect of MAP on two fundamental aspects:
1) Reproducibility of the TGM. No differences were found when comparing the MAP values obtained simultaneously with the first and second A measurements. Therefore, the patient's blood pressure did not interfere with the study of the TGM reproducibility.
2) The QA of the AVF. No correlations were found between the MAP and the QA of the AVF, even when MAP values higher or lower than 100 mmHg are considered separately.
Therefore, it has shown a total independence between the AVF function (assessed objectively by calculating the QA) and the MAP in the current study. This result may be explained by the fact that QA measurements were made at the beginning of the HD session, when blood pressure was stable, avoiding subsequent drops in blood pressure secondary to the ultrafiltration scheduled.
In this regard, according to Rehman et al., the MAP is the main factor that determines the QA variations during HD so that, after 90 minutes of the start of the HD session, for every 10% decrease in the MAP, the QA is reduced by 8 %.20
In summary, the main objective of the VA surveillance programs in the HD units is to prevent thrombosis in prevalent patients. To do this, you must have in the HD room an objective screening method of simple application that allows us to know the AV function reliably in the shortest time possible. The TGM associated with Twister™ device meets all these requirements and can help us achieve the goal of reducing the current rate of VA thrombosis.
Acknowledgements
We would like to thank Fresenius Medical Care for providing the TwisterTM device.
Conflicts of interest
The authors affirm that they have no conflicts of interest related to the content of this article.
Figure 1. The TwisterTM device
Figure 2. Time needed to calculate QA using TGM
Figure 3. Absolute difference between mean QA obtained by TGM and by Delta-H
Figure 4. Correlation between QA values at the AVF obtained by TGM and by Delta-H (n=30)
Figure 5. Bland-Altman graph representing the relationship between mean QA obtained by TGM and by Delta-H
Table 1. Characteristics of patients and AVF studied using TGM
Table 3. Relationship between the obtained QA and the variables from the patient and the AVF
11132_19157_27937_en_ref.1113212193_11132_19115_20692_es_11132_tabla2_en.doc
Table 2. QA and MAP values taken during 2 consecutive haemodialysis sessions
11132_19157_27939_en_ref.1113212193_11132_19115_20694_es_11132_tabla4_en.doc
Table 4. Required time to calculate the QA using three methods for AVF surveillance