Dear Editor,
Haemodialysis (HD) constitutes the first option of Renal Replacement Therapy (RRT) in incident patients, and the second in prevalent patients, according to the SEN (Spanish Society of Nephrology) record of 2006.1 According to the 2006 Renal Patients Registry in Extremadura,2 87.07% of incident patients and 52.55% of prevalent patients on RRT were on HD.
In the province of Caceres, HD is the first RRT option in incident patients (85.7%) and prevalent patients (51.8%). Given that Vascular Access (VA) conditions the effectiveness of HD, the morbidity and mortality (major cause of hospital admission) and their quality of life, makes the creation of a proper VA urgent.
In order to review the current VApractice in our province and compare it to that from Spain, Europe and the United States and to evaluate the level of compliance with the quality standards recommended in the SEN3 and the K/DOQI Vascular Access for HD Guidelines,4 we have carried out a retrospective, observational study of VAin incident and prevalent HD patients in 2007.
A multicentre study published in 2001 by the Vascular Access Work Group is used as the main reference for VA practice at the national level5 and at the international level, the DOPPS study,6 which examines the trends in VA use in Europe and in the United States.
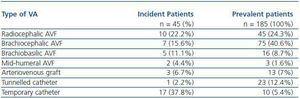
We found that during 2007, of the 45 HD patients that started treatment (incident population), 28 (62.2%) patients had permanent VA (53% native AVF, 7% graft and 2% permanent catheter) and 17 (37.8%) had no vascular access (table 1).
When compared with the National, European and North American references, the report on vascular access from 2001 revealed that 56% of patients started HD with a definitive VA and 44% with a temporary catheter.
According to DOPPS, in the United States 60% of patients began HD with venous catheters (59% tunnelled and 41% temporary); that is, 75% of all HD patients had definitive VA. Whereas in Europe, 31% of patients commenced HD with a catheter, 25% of them tunnelled and 23% had no definitive VA at the start of HD.
The vascular access in HD guidelines of the SEN recommend, as a quality indicator, that 80% of the patients that start HD should have a permanent VA. Regarding this target, our province is under achieving. When we examined the different types of definitive VA in use in our province, we found 53% of patients have a native AVF, 7% have a graft and 2% have tunnelled catheters (table 1). The Spanish study of the VA group does not offer comparative data and, according to the DOPPS, in Europe 66% started HD with a native AVF, 2% with a graft and 8% with tunnelled catheters, while in the United States, only 15% used a native AVF, 24% grafts and 25% tunnelled catheters.
The K/DOQI guidelines of 2006 recommend a native AVF rate of 50% or greater in incident patients as the clinical standard. In this regard, our province complies with this guideline.
Concerning the temporary VA, 17 patients started HD with a catheter: one subclavian, 9 femoral andseven jugular and they were used during an average time of 11, 34 and 64 days, respectively.
The K/DOQI guidelines recommend that temporary jugular catheters should not be left in place for more than a week, and less than 5 days for femoral catheters. The VA guidelines of the SEN advise that femoral catheters should not be left in place for more than seven days, and although they do not address the jugular catheters, they recommend that if the catheter is going to be left in place for more than four weeks, it should be tunnelled.
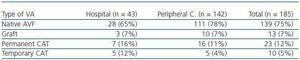
Regarding the VA in the prevalent population, as of 31 December 2007 of the 185 patients that were on HD, 139 (75%) had a native AVF, 13 (7%) grafts, 23 (12%) permanent catheters and 10 (6%) temporary catheters (table 1). When we analysed separately the practice in the hospital and in the satellite renal units (table 2), we can see that the percentage of native AVF is much greater in the peripheral centres, while the use of central venous catheters is greater in the hospital. This is most likely due to the fact that older patients and those with greater comorbidity are hospital-based.
The SEN Report on vascular access of 2001 stated that 80% of the patients had native AVF, 9% grafts and 11% catheters. Data from the DOPPS study show that in the United States there was a greater use of grafts (58% ) and, 24% native AVF, 10% permanent catheters and 7% temporary catheters. Whilst in Europe 80% of patients had native AVF, 10% prosthesis, 6% tunnelled catheter and 2% temporary catheter. The VAguidelines of the SEN from 2005 propose, as a quality indicator, that the majority of the patients use a native AVF for dialysis, recommending a rate of at least 80%. Our province is below this target achieving 75% native AVF in our HD population, that is 78% in peripheral centres and 65% in hospital.
Regarding the tunnelled catheters, the SEN guidelines consider as quality criteria the minimization of their use as a permanent access, recommending < 10%. In our province, 12% had this type of VA (16% in hospital and 11% in peripheral centres).
The multicentre Spanish study does not differentiate between permanent and temporary catheters, and thus this information is not available at a national level. Regarding DOPPS, in Europe the use of tunnelled catheters was found in 6%, and in the United States, 10% of HD patients.
Our study reveals that currently the VA situation in our province is not adequate, with an elevated percentage of patients that begin HD with temporary access that is left in place longer than recommended. Regarding prevalent patients, the rate of native fistulae is below the recommended standard set in the clinical guidelines. However our number of permanent catheters is above target, especially at the hospital level. To improve appropriate VA rates at the start of HD, a multidisciplinary approach is needed between Primary Care, referring patients early, and nephrologists and vascular access surgeons. Regarding patients that are already on dialysis, a periodic evaluation is needed of their vascular access to detect potentially repairable malfunctions that might result in the loss of the access site and that would compromise future vascular sites, and to limit the use of temporary catheters.
Table 1. Types of vascular access in incident and prevalent patients
Table 2. Types of vascular access in prevalent patients in the different centres