This study focuses on the main complication associated with peritoneal dialysis, peritonitis. Its relevance derives from its high morbidity, the negative effect it has on the peritoneum as a dialysis membrane and its financial cost.
MethodsAnalytical, non-interventional, observational cohort study, whose main objective is the analysis of peritonitis in patients on peritoneal dialysis in Andalusia from 1 January 1999 to 31 December 2017, with a total of 2904 peritonitis cases. The database used is the Andalusian Autonomous Transplant Coordination Information System (SICATA).
ObjectivesTo ascertain how the rate of peritonitis is evolving in our community, analyse descriptive data pertaining to patients and peritonitis, ascertain the course of these infectious complications and analyse the factors that influence these cases of peritonitis and their outcomes: germ, hospitalisation and date.
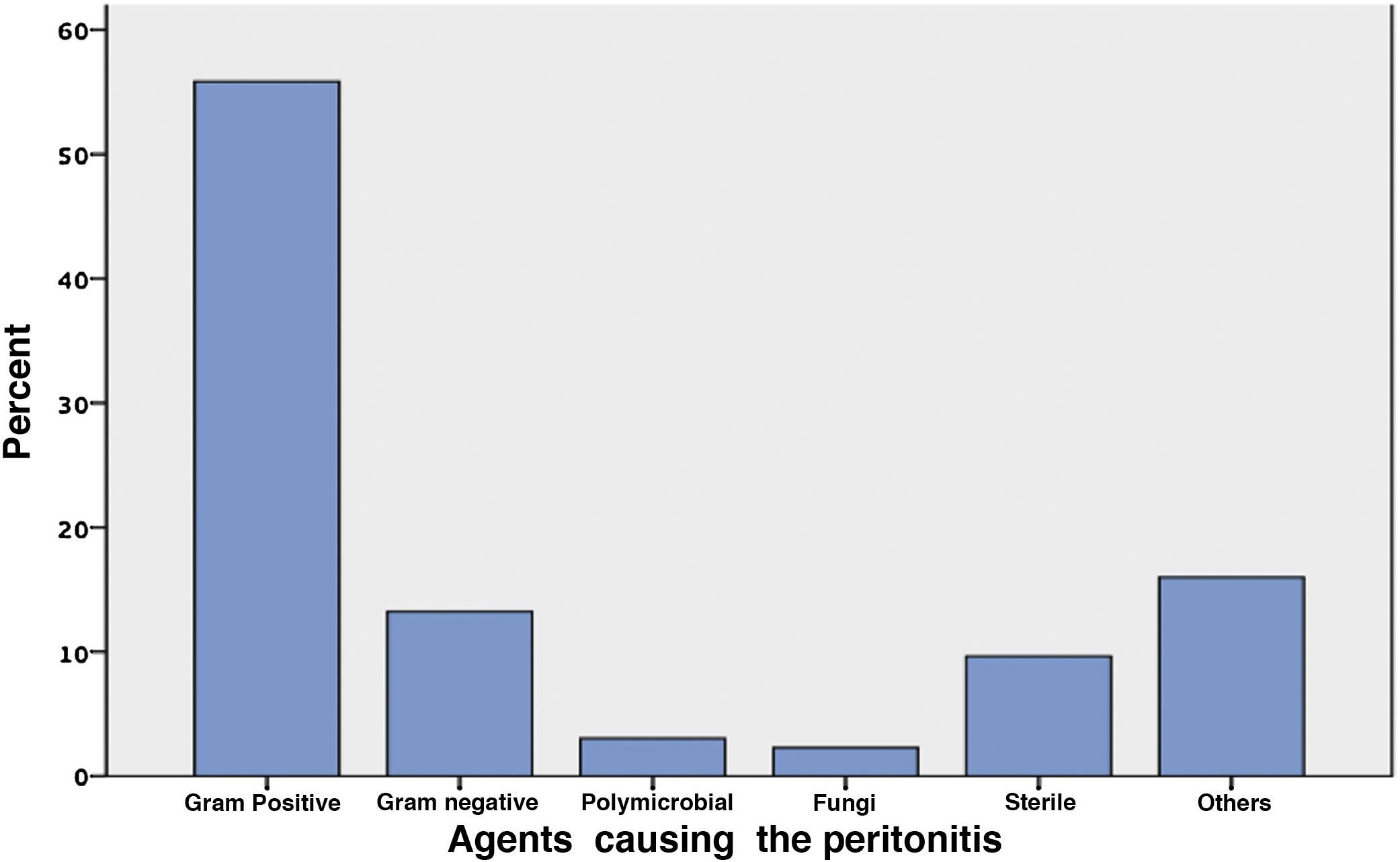
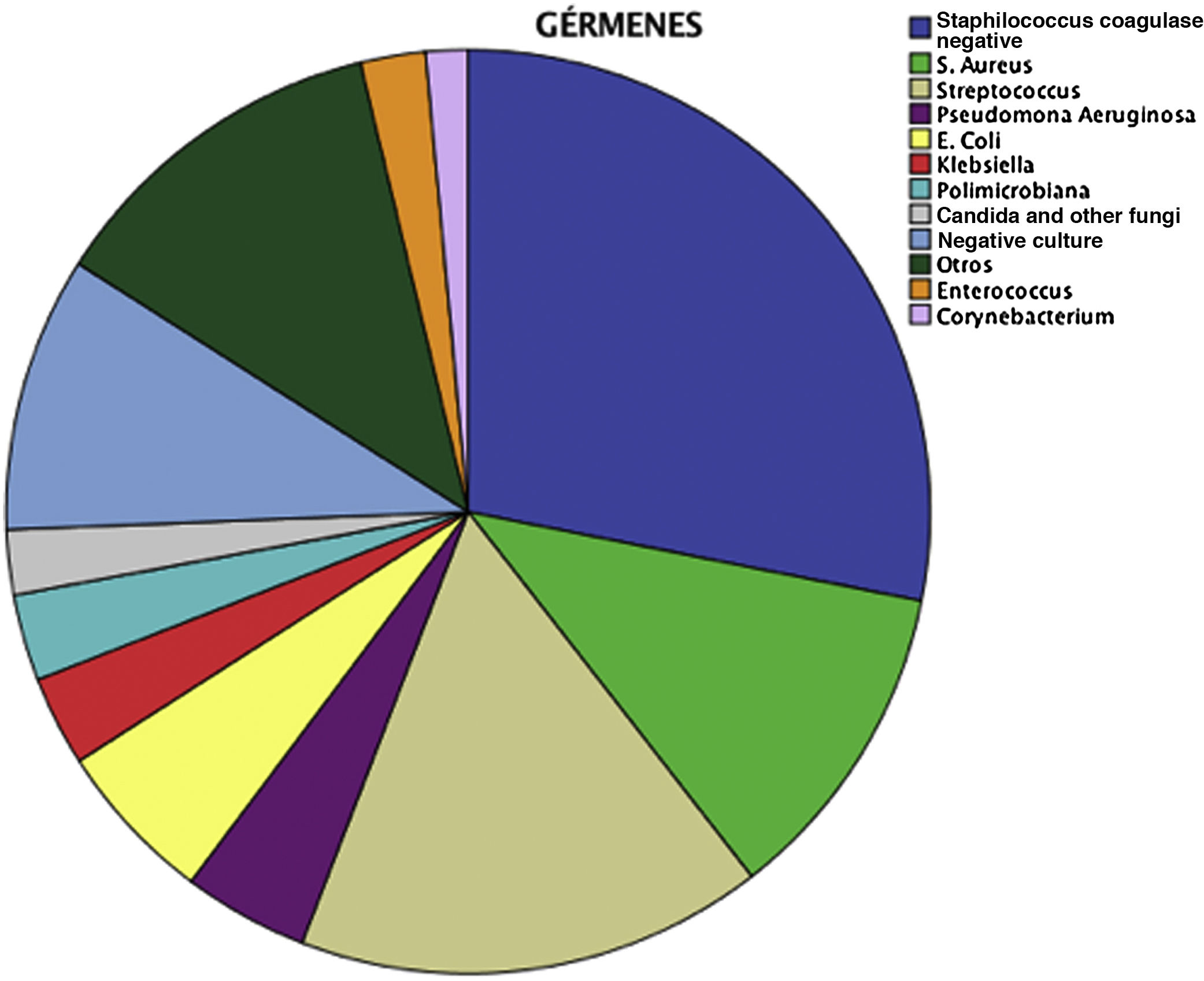
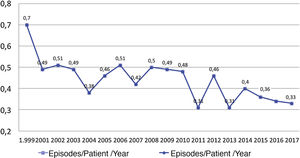
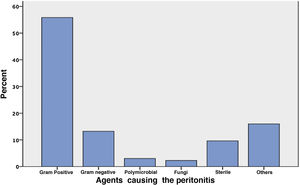
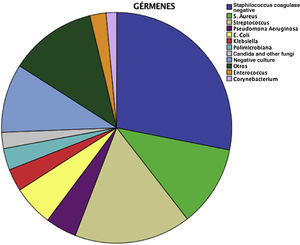
ResultsThe rate of peritonitis decreased progressively during the study period, from 0.7 peritonitis per patient in 1999 to 0.33 at the end of the period. Most infections were treated on an outpatient basis (72.5%). The most common germs were Gram-positive (55.9%), including coagulase-negative staphylococci (28.1%). Most cases of peritonitis progressed to healing (77.8%). The factors that significantly influence the need for hospitalisation and peritonitis progression were the causative germ and associated exit site infection.
ConclusionsIn our population, the rate of peritonitis decreased progressively during the study period, meeting guideline recommendations.
Este estudio se centra en la principal complicación asociada a diálisis peritoneal, la peritonitis. Su relevancia deriva de su elevada morbilidad, el efecto negativo que provoca en el peritoneo como membrana de diálisis y de coste económico que ocasiona.
MétodosEstudio observacional de cohortes, analítico, no intervencionista, cuyo objetivo principal es el análisis de las peritonitis en pacientes en diálisis peritoneal, en Andalucía en el periodo: 1 de enero de 1999 a 31 de diciembre de 2017, con un total de 2.904 peritonitis. La base de datos utilizada es la del Sistema de Información de la Coordinación Autonómica de Trasplantes de Andalucía (SICATA).
ObjetivosConocer la evolución de la tasa de peritonitis en nuestra comunidad, analizar datos descriptivos relacionados con los pacientes y las peritonitis, conocer la evolución de estas complicaciones infecciosas y analizar los factores que influyen en estas peritonitis y en su evolución: germen, hospitalización y fecha.
ResultadosLa tasa de peritonitis ha disminuido progresivamente durante el periodo de estudio desde 0,7 peritonitis por paciente en 1999 hasta 0,33 al final del periodo. La mayoría de las infecciones se tratan de manera ambulatoria (72,5%). Los gérmenes más frecuentes fueron los grampositivos (55,9%), y entre ellos, los estafilococos coagulasa negativos (28,1%). La mayoría de las peritonitis evolucionan a la curación (77,8%). Los factores que influyen de manera significativa en la necesidad de hospitalización y en la evolución de la peritonitis son el germen causal y la presencia de infección del orificio de salida asociado.
ConclusionesEn nuestra población, la tasa de peritonitis ha disminuido progresivamente durante el periodo de estudio, alcanzando las recomendaciones de las guías.
- -
Peritonitis is one of the main complications of peritoneal dialysis.
- -
In the population studied, the rate of peritonitis has progressively decreased during the study period.
- -
Most cases are treated as outpatient.
- -
The need for hospitalization and evolution depend on the germ and association with the peritoneal catheter exit-site and tunnel infections. (ESI)
Despite technical advances that have reduced the rate of peritonitis in peritoneal dialysis (PD) it continue to be the main complication in these patients. Peritonitis is an important cause of morbidity, mortality, high costs, a obstacle to the selection of PD and the main cause of failure of the technique and transfer to hemodialysis (HD).1–4
The main sources of information on peritonitis are based on large national registries of patient cohorts, with a long-term follow-up that allow the analysis of the different variables that may influence the risk and their consequences.5–12
Therefore, the nephrology community continues to show the great attention in the prevention and treatment of PD-related infections.
ObjectivesThis article presents the first results of a global project, without precedent in our community, of all PD-related peritonitis in the region of Andalusia (south of Spain), from January 1, 1999 to December 31, 2017, with the intention to initiate a line of research and analysis which will provide information on different features of peritonitis: rate, demographics, clinical characteristics, microbiological aspects, as well as the factors that may influence both the risk and the evolution of peritonitis.
The main objective is to analyze the evolution of the rate peritonitis during the entire follow-up period. As a secondary objective, is to examine the influence of the type of germ and the presence of catheter exit-site infections (ESI) on the need of hospitalization and clinical evolution of the patient.
Patients and methodsStudy designObservational cohort study, multicenter, which includes all hospitals that perform PD in Andalusia during a period of 19 years (1999–2017). It includes the demographic data of the incident patients in such a period (n = 2904), as well as the characteristics of the technique. The total number of peritonitiss episodes registered and analyzed has been 2,656.
All data have been obtained from the Information System of the Autonomous Coordination of Transplants of Andalusia (SICATA).
This registry includes all patients treated with PD in our community. The inclusion of patients in this registry is of a mandatory official nature and patients provide consent for the analysis of the data.
VariablesIt includes patient related variables and characteristics of peritoneal dialysis: date of birth, sex, etiology of chronic kidney disease, date of initiation of peritoneal dialysis, cause of inclusion in peritoneal dialysis, type of catheter, method of implantation of the catheter, modality of PD [CAPD / APD], use of icodextrin and type of buffer in the PD solution. The variables related to peritonitis were: date of peritonitis, association with catheter exit-site infections (ESI), evolution of peritonitis (classified into four categories: cure, recurrence, catheter removal, death), days of hospitalization, and microbiological data: isolated germ.
Statistical methodsThe data have been analyzed using the statistical software package IBM statistics SSPS V24 (year 2016), using measures of central tendency and dispersion (means, standard deviation), for quantitative variables, and frequencies for qualitative variables; for inferential statistics the data is compared using the χ 2 test and Student's t test, according to the types of variables, risk determination and 95% confidence intervals.
The rate of peritonitis is calculated as the number of peritonitis per patient per year. The total months at risk has been calculated in each patient and the number of peritonitis was divided by total months.
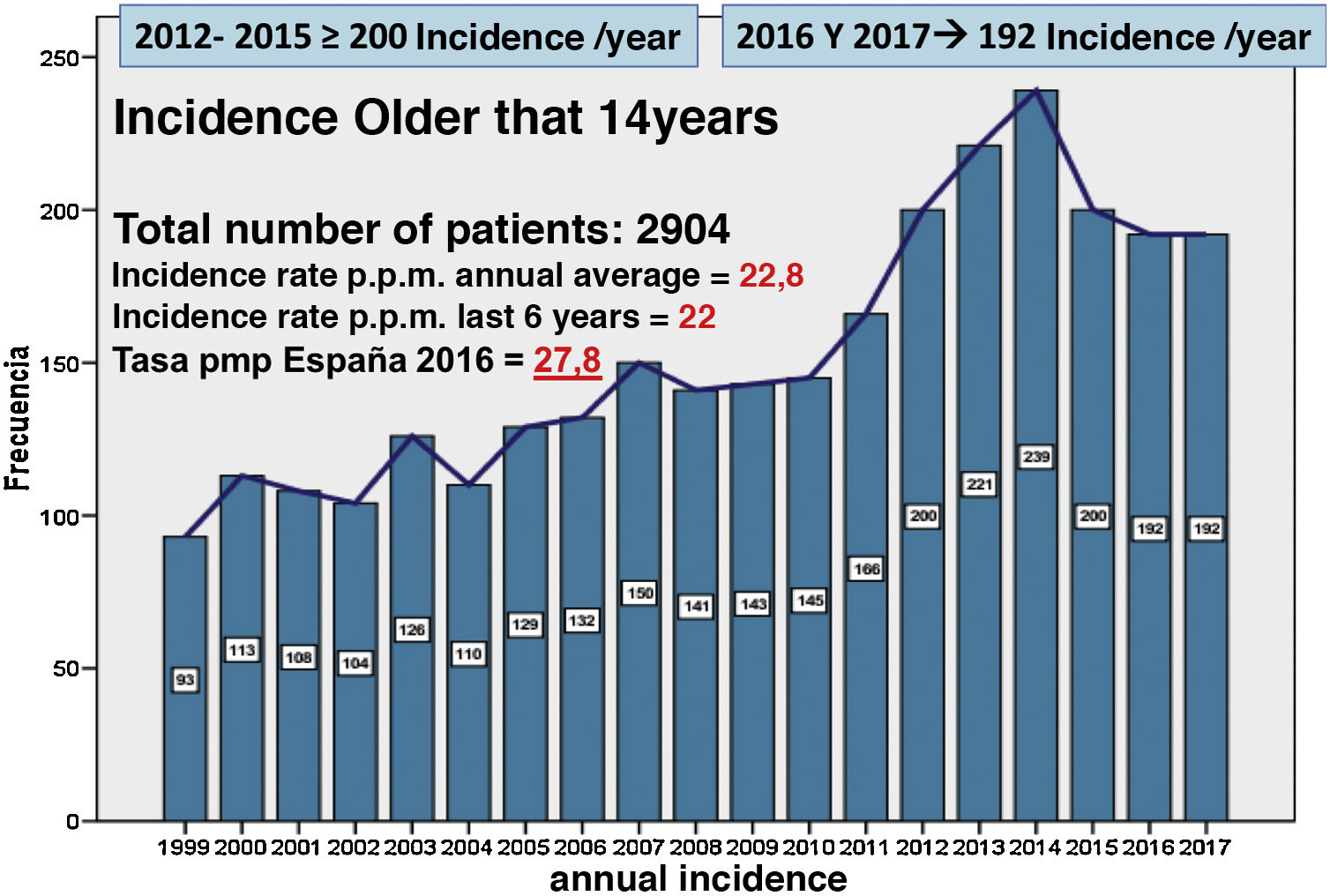
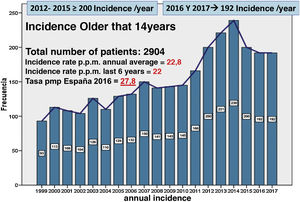
ResultsDemographic and technical dataThere were 2904 patients treated with PD in Andalusia between January 1, 1999 and December 31, 2017 (Fig. 1). The annual incidence has increased twofold, from 93 patients at the beginning of the registry, to 192 in the year 2017. The highest incidences have taken place in the years 2012–2015, with more than 200 patients per year, decreasing in the last two years to 192 incident patients. The average annual incidence rate of patients per million inhabitants has been 22.8 and in the last six years has been 22.
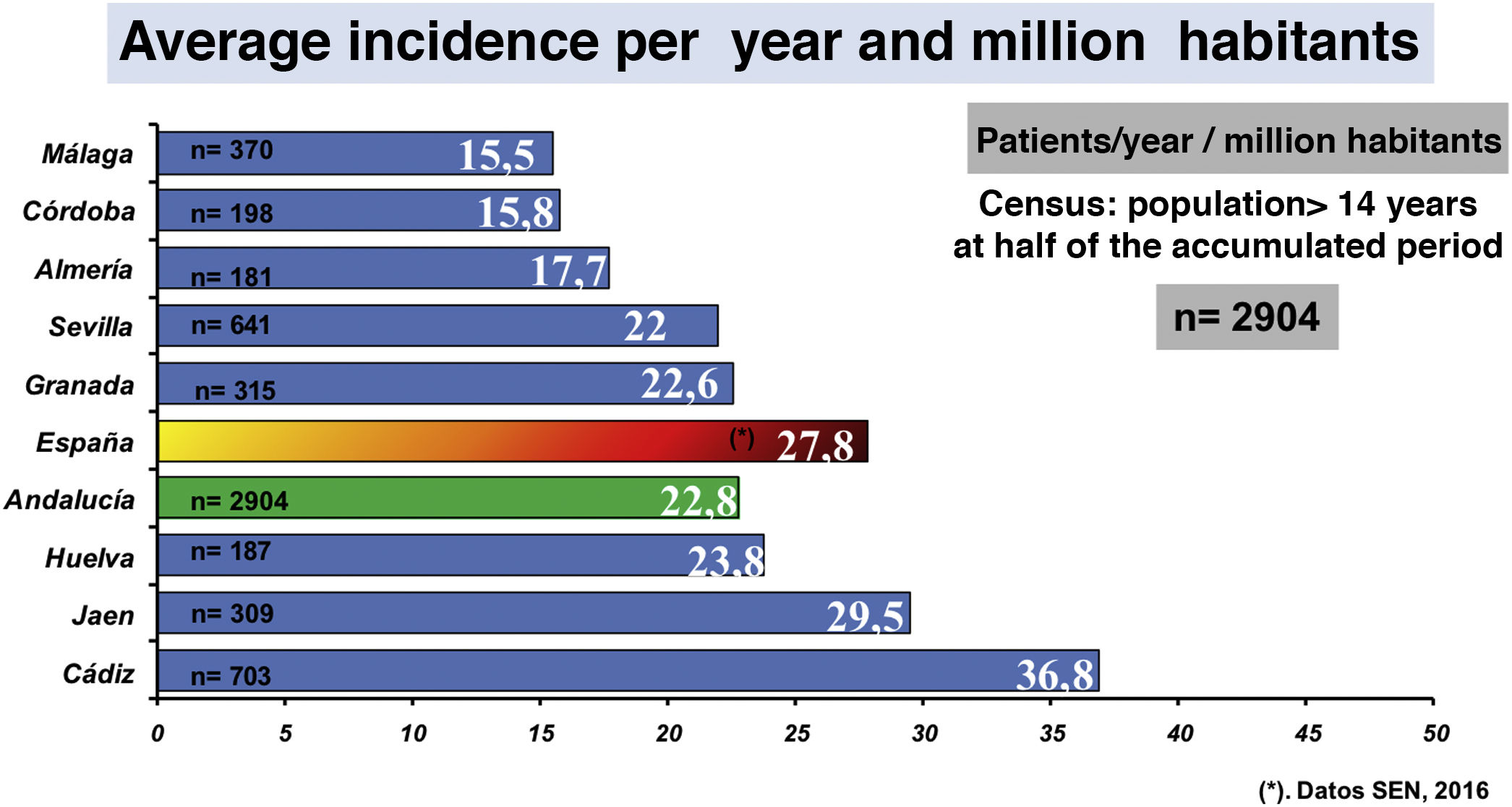
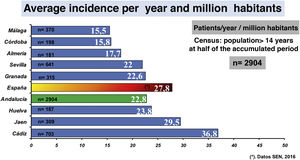
The distribution by provinces and per million inhabitants of incident patients on PD in the period 1999–2017 (patient/year/million habitants). The data ordered from highest to lowest is : Cádiz: 36.8; Jaén: 29.5; Huelva: 23.8; Granada: 22.6; Seville: 22; Almeria 17.7; Cordoba 15.8; Malaga 15.5 (Fig. 2). The average for Andalusia is 22.8 patient/year/million-habitants.
Men are predominant (60.2%). The average age is 56.68 years (SD 16.2). It should be mentioned that 41.7% of patients started PD between the ages of 61 and 80. The main causes of end-stage kidney disease (ESRD) in these patients were: glomerulonephritis (22.7%) and diabetic nephropathy (19.8%).
The most frequent catheter implanted was the Swan Neck type (52.9%), followed by the straight two-cuff Tenckhoff catheter (20.3%).
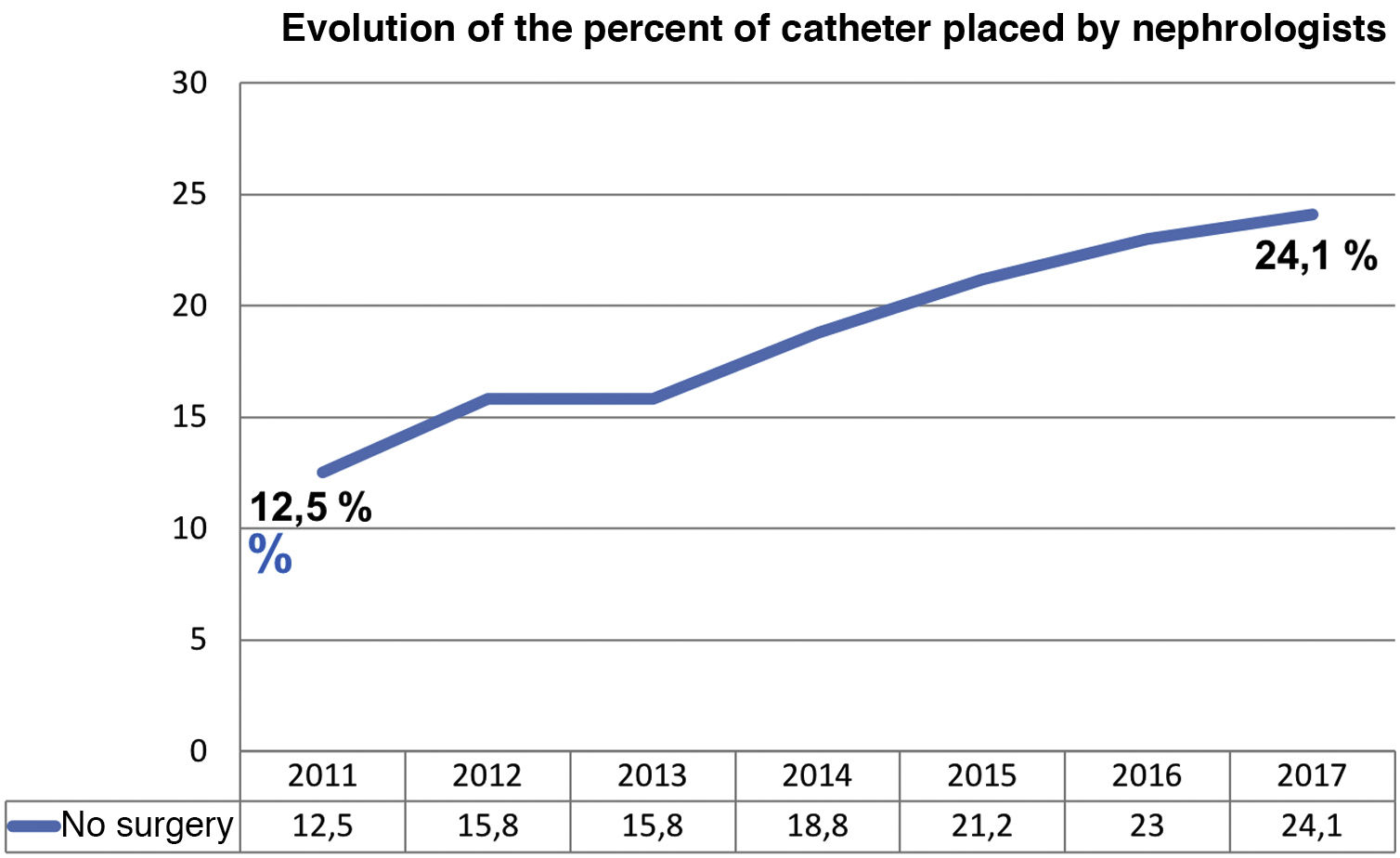
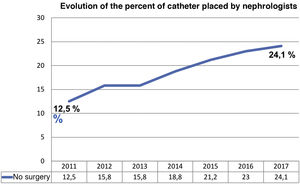
The implantation was performed surgically by laparoscopic technique in 75.9% of the cases and the location was predominantly paramedial (81.3%). In recent years, there has been an increase in catheters placed by the nephrologist using percutaneous technique, increasing from 11.5% of catheters in 2011 to almost a quarter of the total in 2017 (24.1%) (Fig. 3).
The use of automatic peritoneal dialysis (APD) has doubled during the study period, from 23.5% in 2000 to 42.2% in the last year.
In addition, the use of icodextrin solutions has increased (36% before 2009, up to 49.3% in 2017) and solutions with bicarbonate as a buffer have also increased, (56.2% before 2009 to 90% of cases in 2017).
Results in peritonitisThe sample comprises 2656 episodes of peritonitis presented in the PD population of Andalusia, during the years 1999–2017.
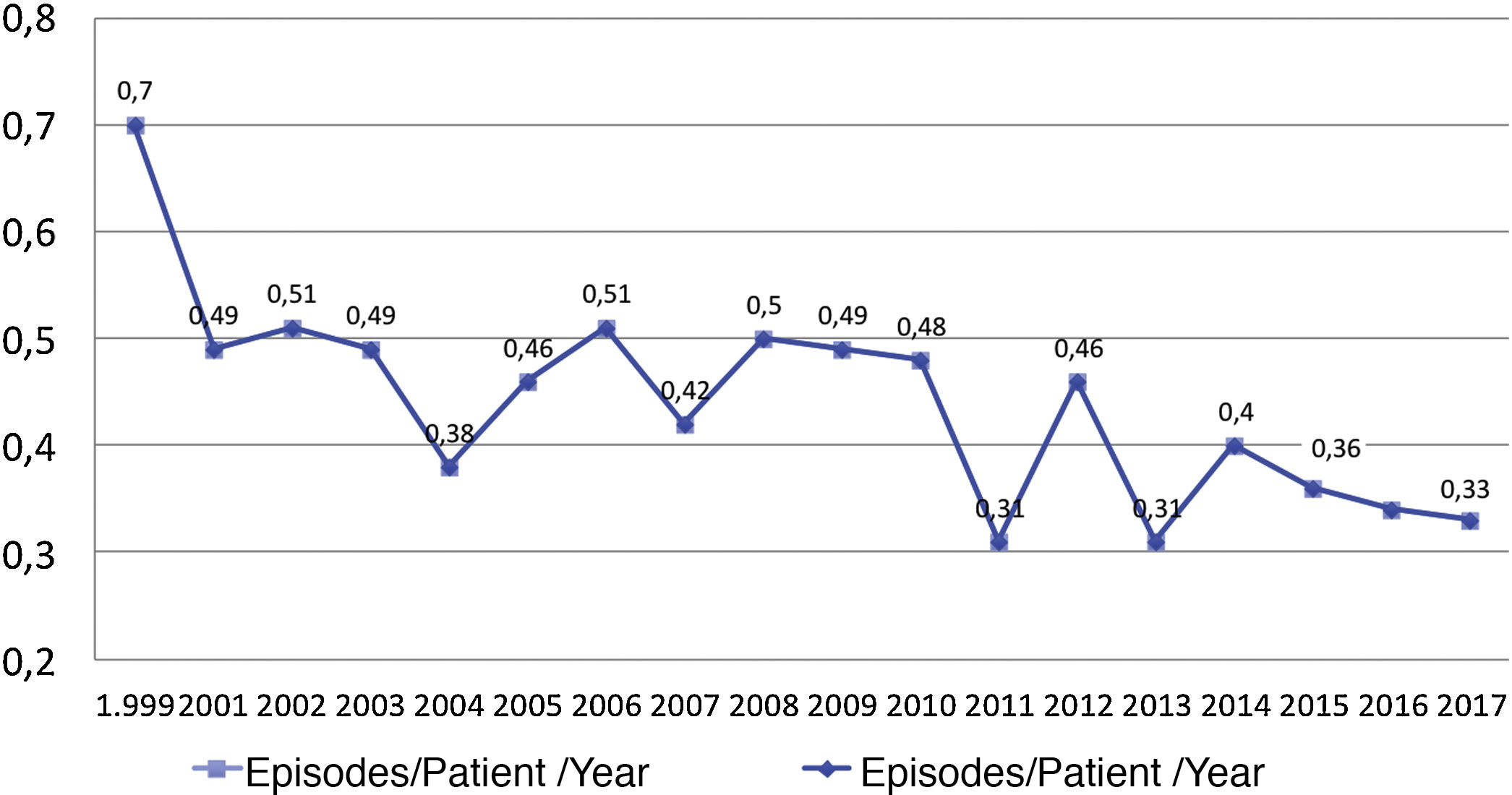
The peritonitis rate has decreased by half since the beginning of the study, from 0.7 peritonitis per patient year in 1999 to 0.33 in 2017 (Fig. 4).
Throughout the entire period, a 27.5% of patients (n = 730) required hospitalization for peritonitis. The mean number of days of hospitalization was 5.7 days (SD 8.4).
Exit site infection (ESI) associated with peritonitis occurred in 10.5% of patients.
Regarding the etiological agent of peritonitis, gram-positive bacteria were the most frequent (55.9% of cases), gram-negative bacteria in 13.2%, and polymicrobial
infection in 3%. The remaining cases were fungi (2.3%), sterile (9.6%) and other unclassified germs (16%) named in the data base as mycobacteria and others (Fig. 5)
The most frequent etiological agent was coagulase negative staphylococci (28.1%), followed in frequency by Streptococcus sp. (16.4%) (Fig. 6).
In polymicrobial peritonitis, the causative agent most frequently registered was E. coli (29.2%) and the second most frequent is Streptococcus sp. (twenty-one%).
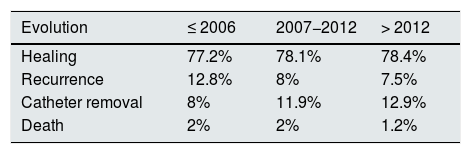
Regarding the evolution of peritonitis, the majority of cases are cured (77.8%). Recurrences occur in 9.6% of cases. In 10.8% it was necessary to remove the peritoneal catheter and in 1.8% of the cases it progressed to the death of the patient due to peritonitis.
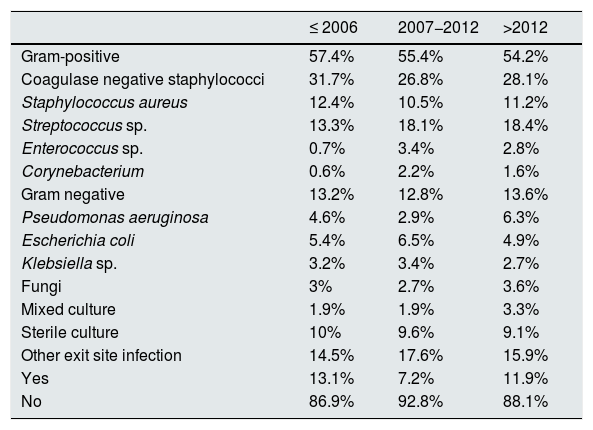
To evaluate whether there have been differences over these 19 years, in terms of the frequency and severity of peritonitis episodes, we have divided the total follow-up time into three periods, analyzing the type of isolated germ, the association with peritoneal catheter exit-site infection (ESI) and the evolution of the episode. The periods were divided taking into account that around 2004 appeared more biocompatible dialysis solutions as compared with the previous ones.
The periods studied were from 1999 to 2006 (36.8% of peritonitis), from 2007 to 2012 (37.8% of peritonitis) and from 2013 to 2017 (with 25.3% of peritonitis).
No significant differences have been found between periods, in terms of the large taxonomic groups of germs (gram-positive, gram-negative or fungi, p > 0.05), although in the more specific analysis looking at specific germs, significant differences are observed in some cases (Table 1).
Differences between the periods evaluated regarding the types of germs and the presence of exit-site infection.
| ≤ 2006 | 2007−2012 | >2012 | |
|---|---|---|---|
| Gram-positive | 57.4% | 55.4% | 54.2% |
| Coagulase negative staphylococci | 31.7% | 26.8% | 28.1% |
| Staphylococcus aureus | 12.4% | 10.5% | 11.2% |
| Streptococcus sp. | 13.3% | 18.1% | 18.4% |
| Enterococcus sp. | 0.7% | 3.4% | 2.8% |
| Corynebacterium | 0.6% | 2.2% | 1.6% |
| Gram negative | 13.2% | 12.8% | 13.6% |
| Pseudomonas aeruginosa | 4.6% | 2.9% | 6.3% |
| Escherichia coli | 5.4% | 6.5% | 4.9% |
| Klebsiella sp. | 3.2% | 3.4% | 2.7% |
| Fungi | 3% | 2.7% | 3.6% |
| Mixed culture | 1.9% | 1.9% | 3.3% |
| Sterile culture | 10% | 9.6% | 9.1% |
| Other exit site infection | 14.5% | 17.6% | 15.9% |
| Yes | 13.1% | 7.2% | 11.9% |
| No | 86.9% | 92.8% | 88.1% |
Regarding the evolution of peritonitis, we found a significant improvement throughout the periods studied (p < 0.01) (Table 2).
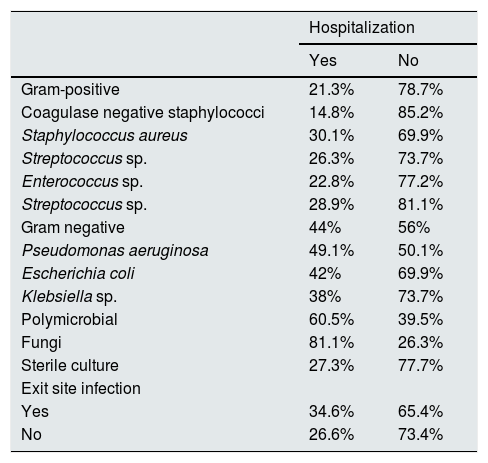
An analysis was carried out to assess the possible influence of the germ (studied according to gram-positive, gram-negative, polymicrobial bacteria, fungi, or sterile cultures, and also according to the specific germs), and the presence of exit site infection that requires patient hospitalization due to peritonitis (Table3).
Hospitalization rates based on the germ and the presence of exit site infection.
| Hospitalization | ||
|---|---|---|
| Yes | No | |
| Gram-positive | 21.3% | 78.7% |
| Coagulase negative staphylococci | 14.8% | 85.2% |
| Staphylococcus aureus | 30.1% | 69.9% |
| Streptococcus sp. | 26.3% | 73.7% |
| Enterococcus sp. | 22.8% | 77.2% |
| Streptococcus sp. | 28.9% | 81.1% |
| Gram negative | 44% | 56% |
| Pseudomonas aeruginosa | 49.1% | 50.1% |
| Escherichia coli | 42% | 69.9% |
| Klebsiella sp. | 38% | 73.7% |
| Polymicrobial | 60.5% | 39.5% |
| Fungi | 81.1% | 26.3% |
| Sterile culture | 27.3% | 77.7% |
| Exit site infection | ||
| Yes | 34.6% | 65.4% |
| No | 26.6% | 73.4% |
p < 0.01 for both analysis.
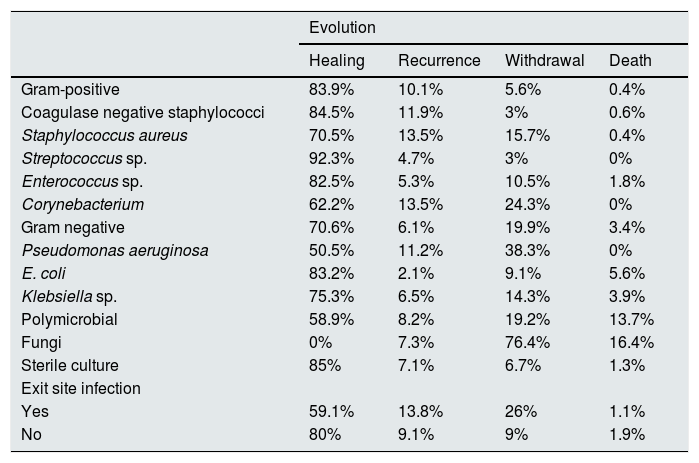
Finally, an analysis was performed to determine the influence of the germ and the presence of exit site infection on the evolution of peritonitis. As shown in Table 4, both the type of germ and the accompanying infection of the exit site influence the results. It should be highlighted that relapses or withdrawals of the catheter are more frequent in infections due to Staphylococcus aureus, Corynebacterium and Pseudomonas aeruginosa. A negative outcome, including the death of the patient, occurs in polymicrobial infections and, above all, in fungal infections. Peritonitis related to catheter infections also has a worse outcome.
Possible evolutions of peritonitis depending on the type of germ and the presence of exit orifice infection.
| Evolution | ||||
|---|---|---|---|---|
| Healing | Recurrence | Withdrawal | Death | |
| Gram-positive | 83.9% | 10.1% | 5.6% | 0.4% |
| Coagulase negative staphylococci | 84.5% | 11.9% | 3% | 0.6% |
| Staphylococcus aureus | 70.5% | 13.5% | 15.7% | 0.4% |
| Streptococcus sp. | 92.3% | 4.7% | 3% | 0% |
| Enterococcus sp. | 82.5% | 5.3% | 10.5% | 1.8% |
| Corynebacterium | 62.2% | 13.5% | 24.3% | 0% |
| Gram negative | 70.6% | 6.1% | 19.9% | 3.4% |
| Pseudomonas aeruginosa | 50.5% | 11.2% | 38.3% | 0% |
| E. coli | 83.2% | 2.1% | 9.1% | 5.6% |
| Klebsiella sp. | 75.3% | 6.5% | 14.3% | 3.9% |
| Polymicrobial | 58.9% | 8.2% | 19.2% | 13.7% |
| Fungi | 0% | 7.3% | 76.4% | 16.4% |
| Sterile culture | 85% | 7.1% | 6.7% | 1.3% |
| Exit site infection | ||||
| Yes | 59.1% | 13.8% | 26% | 1.1% |
| No | 80% | 9.1% | 9% | 1.9% |
p < 0.01 for both analyses.
This is a multicenter retrospective observational study of peritonitis. The main complication in PD patients in the Andalusian community during the period of year 1999–2017.
As compared with hemodialysis, the number of patients in peritoneal dialysis in Andalusia is scarce (mean incidence of 22 patients/million inhabitants/year). However, it should be noted that there has been a progressive increase, doubling the annual incidence at the end of the follow-up period. In addition, the incidence of PD is very heterogeneous among the different provinces of the region; Cádiz and Jaén are above the average, and the figures are similar to the national average.13 As in the rest of the national and international PD registries, our patients are mainly distributed between the 40–60 and 60–80 age groups.14 Other demographic and technical data to highlight is that similar to other published studies, the glomerulopathies and diabetes mellitus are the main causes of ESRD, and the proportion of catheters implanted by the nephrologist has increased.15,16 During the follow-up period there has been an increase in the use of APD (currently around 40%) and biocompatible solutions (currently greater than 90%).17–19
The rate of peritonitis has been reduced progressively during the study period, from 0.7 peritonitis per patient/year to less than half 0,33 peritonitis per patient/year at the end of the study period, which is already lower than the target recommended by the International Society of Peritoneal Dialysis (ISPD) in years 2016 and 2017 on peritonitis and catheter-related infections, that should not exceed f 0.5 episodes per patient per year.20
Similar results on a favorable evolution over time have been presented in other registries, such as the group by Szeto et al. (from 1.10 to 0.46 episodes/patient/year) between 1994 and 2003.21
Rates of peritonitis varies between countries or geographical areas; some have the rates recommended by ISPD, and similar to Andalusia, such as Portugal, the United States, Canada and France, with rates of 0.39, 0.37, 0.33 and 0.36 peritonitis/patient/year, respectively. However others, have had higher peritonitis rates, such as Scotland, Turkey, and Israel, with rates of 0.62, 0.77, and 1.66, respectively. And some other registries present peritonitis rates below ours, such as Japan (0.17), Australia (0.24) and China (0.20),21–30 which suggests to insist on the strategies related to the technique that can reduce infections and be closer to the low the rates achieved by these countries.
Another important finding is the significant improvement in the rate of curation in more recent years. It is also important to take into account the arrival of more biocompatible solutions since 2004, with less glucose degradation products (GDP) and with bicarbonate as a buffer, or with osmotic agents such as icodextrin to reduce the load of glucose, that in general offer a better protection for the peritoneal membrane. We have not performed statistical analysis on the effect of the new PD solutions on the rate of peritonitis, however we consider that this should be evaluated in future analysis. In a systematic review of the Cochrane,31–33 these “new solutions” are related with a lower proportion of individuals who experience peritonitis or with global rates of peritonitis. The suggested explanation for this finding is the improvement of the host's peritoneal defense mechanisms, since there was considerable experimental evidence that neutral pH and fluids with low GDP significantly improved the viability and function of peritoneal mesothelial cells, leukocytes. and macrophages. As a limitation of this the meta-analysis, they point out the heterogeneity of the studies on which it is based, so this statement remains uncertain and so performing more randomized and well-designed studies is justified.
We have observed a progressive reduction in exit-site infections linked to peritonitis, and this could be related with a better training of the patient received by specialized nursing, however this possibility has not been the subject of statistical analysis in our study, since this information it is not included in our database. Other authors have analyzed the positive effect of a more thoroughly training on the care of the peritoneal catheter implement by the specialized nurses.34
Finally, it has been analyzed whether the type of germ and the presence of infection of the exit site has an influence on the need for hospitalization and on the evolution of peritonitis:
- -
Peritonitis caused by gram-positive germs is the most frequent and shows a better prognosis with respect to other microbiological groups and this has been reflected in the literature. Among these gram-positive, the coagulase-negative staphylococcal peritonitis is the most frequent, and it is usually related to manual contamination. These germs can present as recurrent peritonitis, in which case it is necessary to suspect that there is colonization of biofilm in the catheter, or loss of sterility in the procedure by the patient. Occasionally, if it is not resolved with strategies dedicated to correct the manipulation of the catheter or destroy the biofilm, it may be necessary to remove the catheter.35 As shown in the study the peritonitis caused by S. aureus, has a worse evolution than the others previously mentioned, since in a greater proportion they are associated with infection of exit site of the catheter, with a higher rate of catheter removal.
- -
Gram-negative peritonitis has a higher risk of loss of the catheter and death of the patient.36 Among these, those produced by Pseudomonas sp. they are usually more severe and mostly associated with exit site infection. As found in our analysis, most of these patients required hospitalization, and even removal of the catheter.37
- -
Finally, fungal peritonitis is a very serious complication, requiring hospitalization of the patient, removal of the catheter, and transfer of the patient to hemodialysis, and is associated with a higher rate of death.38,39
Peritonitis continues to be a complication that may require catheter removal and transfer of the patient to hemodialysis. It can and even cause death in the worst cases.
In the population studied, the rate of peritonitis has decreased progressively during the study period, achieving and even improving the recommendations given by the guidelines.
Most cases are treated on an outpatient basis. However, sometimes it may require hospitalization depending on the type of germ and the association with exit site infection. Likewise, these factors significantly modify the evolution.
Although the results of the study are encouraging, peritonitis should not be forgotten and put all our efforts in continuing to improve and find effective measures to prevent the appearance of peritoneal infections.
This line of investigation of peritonitis related to the PD technique in Andalusia is still open, with objectives and analysis beyond this report.
FinancingThis work has not received any type of funding.
Conflict of interestsThe authors declare that they have no conflict of interest.
Please cite this article as: de la Espada Piña V, Ganga PLQ, Junquero JMG, Fosalba NA, Girón FF, Huete MJE, et al. Dos décadas de análisis de las peritonitis en diálisis peritoneal en Andalucía: aspectos epidemiológicos, clínicos, microbiológicos y evolutivos. Nefrologia. 2021;41:417–425.