Chronic kidney disease (CKD) is a common condition worldwide;1 however, it is vastly underdiagnosed as it frequently remains asymptomatic until reaching advanced stages.2 Thus, a recent database study performed in Spain has shown that in adults, the prevalence of identified CKD reaches only 5% of the population, which is far from previous nation-wide, population-based studies.3 The CKD prevalence is expected to increase in the next future, as people will be older and the proportion of hypertension and diabetes, the leading causes of CKD, are growing.2 CKD increases morbidity and mortality, particularly cardiovascular (CV) disease.2,3 The 2019 European Society of Cardiology (ESC) guidelines of dyslipidemia classify severe CKD (estimated glomerular filtration rate [eGFR]<30mL/min/1.73m2), and moderate CKD (eGFR 30–59mL/min/1.73m2), as very high and high CV risk, respectively, without requiring SCORE estimation.4 However, it is well known that the risk of CV outcomes does not only depend on renal function, but also on albuminuria.3 Thus, the Kidney Disease, Improving Global Outcomes (KDIGO) guidelines include both parameters in the stratification of CV disease.5 As 2019 ESC guidelines included eGFR, but not albuminuria for risk stratification, it would be important to analyze the impact of updating SCORE scale with KDIGO CV risk stratification.
For this purpose, data from BIG-PAC®, a database with information from non-selected 1.8 million persons of primary health care centers and referral hospitals within the Spanish national health system were analyzed.1 Adult patients, with ≥1 diagnostic code of CKD or having laboratory results meeting the definition of CKD, were included. CKD stages were defined according to the eGFR (CKD-EPI) and the urine albumin-to-creatinine ratio (UACR) criteria, as follows: CKD stage 1: eGFR≥90mL/min/1.73m2 and UACR ≥30mg/g; CKD stage 2: eGFR 60–89mL/min/1.73m2 and UACR≥30mg/g; CKD stage 3a: eGFR 45–59mL/min/1.73m2; CKD stage 3b: eGFR 30–44mL/min/1.73m2; CKD stage 4: eGFR 15–29mL/min/1.73m2; and CKD stage 5: eGFR<15mL/min/1.73m2.1 CV risk was classified according to SCORE.4 Moreover, this scale was updated by adding the KDIGO criteria into SCORE scale (Table 1).4,5 Categorical variables were described by their absolute and relative frequencies and were compared with the Chi-square test or the Fisher exact test, when appropriate.
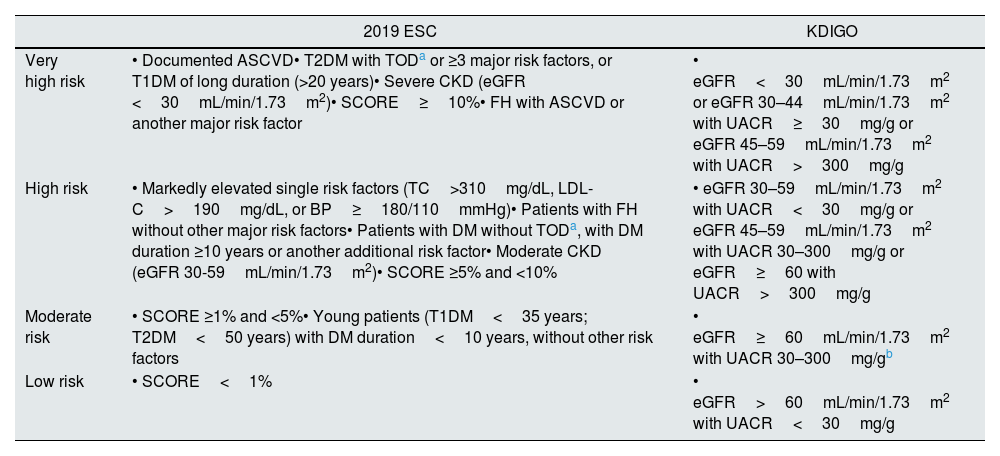
Cardiovascular risk stratification according to 2019 ESC and KDIGO guidelines.
| 2019 ESC | KDIGO | |
|---|---|---|
| Very high risk | • Documented ASCVD• T2DM with TODa or ≥3 major risk factors, or T1DM of long duration (>20 years)• Severe CKD (eGFR <30mL/min/1.73m2)• SCORE≥10%• FH with ASCVD or another major risk factor | • eGFR<30mL/min/1.73m2 or eGFR 30–44mL/min/1.73m2 with UACR≥30mg/g or eGFR 45–59mL/min/1.73m2 with UACR>300mg/g |
| High risk | • Markedly elevated single risk factors (TC>310mg/dL, LDL-C>190mg/dL, or BP≥180/110mmHg)• Patients with FH without other major risk factors• Patients with DM without TODa, with DM duration ≥10 years or another additional risk factor• Moderate CKD (eGFR 30-59mL/min/1.73m2)• SCORE ≥5% and <10% | • eGFR 30–59mL/min/1.73m2 with UACR<30mg/g or eGFR 45–59mL/min/1.73m2 with UACR 30–300mg/g or eGFR≥60 with UACR>300mg/g |
| Moderate risk | • SCORE ≥1% and <5%• Young patients (T1DM<35 years; T2DM<50 years) with DM duration<10 years, without other risk factors | • eGFR≥60mL/min/1.73m2 with UACR 30–300mg/gb |
| Low risk | • SCORE<1% | • eGFR>60mL/min/1.73m2 with UACR<30mg/g |
Modified from original KDIGO as ESC includes 45–59 GFR as high risk category.
ASCVD: atherosclerotic cardiovascular disease; BP: blood pressure; CKD: chronic kidney disease; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate; ESC: European Society of Cardiology; FH: familial hypercholesterolemia; KDIGO: Kidney Disease: Improving Global Outcomes; LDL-C: low-density lipoprotein cholesterol; SCORE: Systematic Coronary Risk Estimation; T1DM: type 1 DM; T2DM: type 2 DM; TC: total cholesterol; TOD: target organ damage.
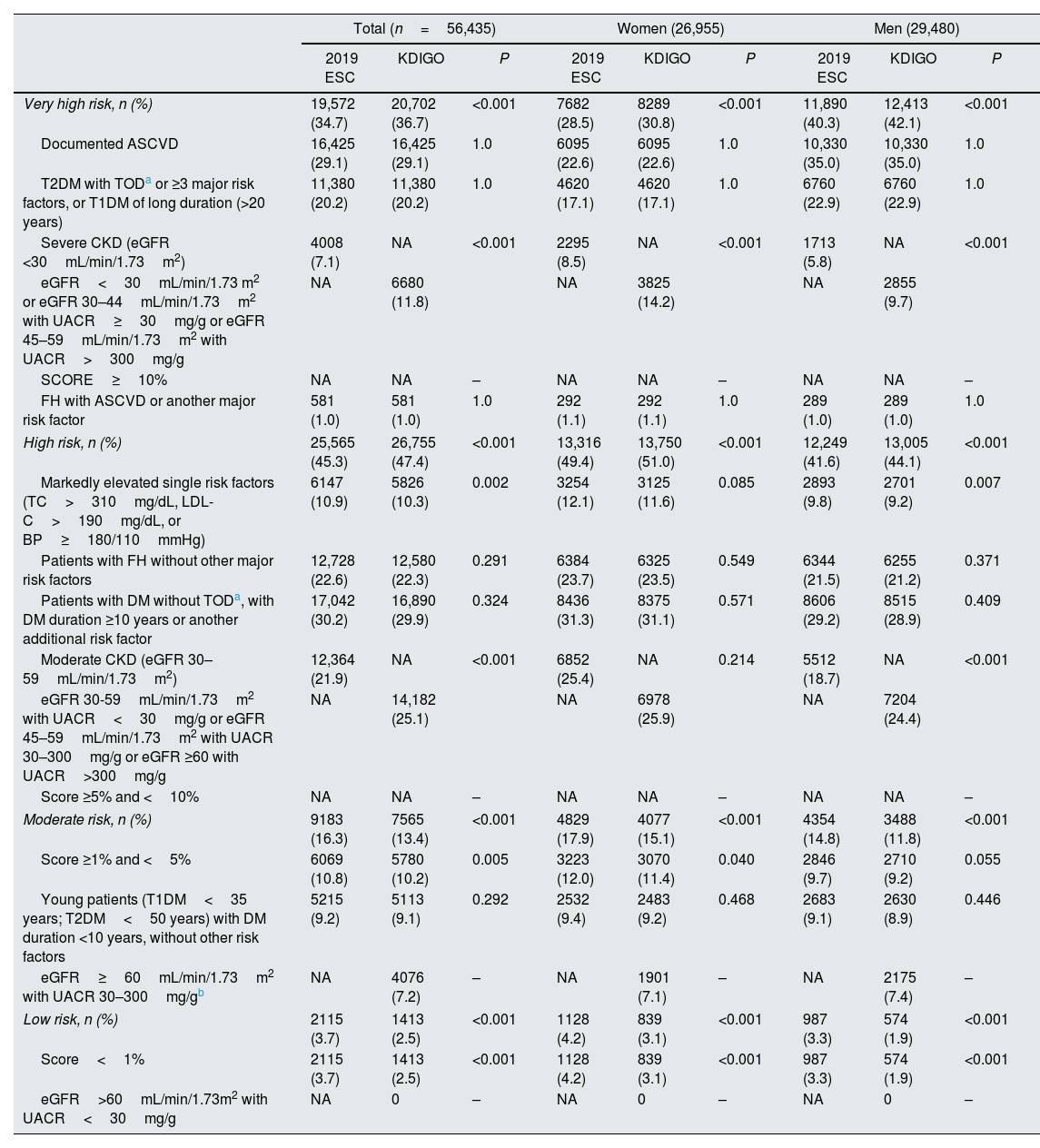
A total of 56,435 (4.91%) patients had CKD, of whom 26,955 (47.8%) were women. According to 2019 ESC guidelines, 34.7%, 45.3%, 16.3% and 3.7% of patients had very high, high, moderate and low CV risk, respectively (80.0% very high/high CV risk). After updating risk stratification with KDIGO criteria, these numbers were 36.7%, 47.4%, 13.4% and 2.5%, respectively; P<0.001 in all cases (84.1% very high/high CV risk). Therefore, the introduction of the KDIGO criteria within the SCORE scale translated into more patients classified as very high and high CV risk patients, respectively (absolute difference: +2.0% and +2.1%; relative difference: +5.8% and +4.6%, respectively; both P<0.001). This occurred in women and men, similarly (Table 2).
Cardiovascular risk stratification of CKD patients according to 2019 ESC guidelines and with the KDIGO modification.
| Total (n=56,435) | Women (26,955) | Men (29,480) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 ESC | KDIGO | P | 2019 ESC | KDIGO | P | 2019 ESC | KDIGO | P | |
| Very high risk, n (%) | 19,572 (34.7) | 20,702 (36.7) | <0.001 | 7682 (28.5) | 8289 (30.8) | <0.001 | 11,890 (40.3) | 12,413 (42.1) | <0.001 |
| Documented ASCVD | 16,425 (29.1) | 16,425 (29.1) | 1.0 | 6095 (22.6) | 6095 (22.6) | 1.0 | 10,330 (35.0) | 10,330 (35.0) | 1.0 |
| T2DM with TODa or ≥3 major risk factors, or T1DM of long duration (>20 years) | 11,380 (20.2) | 11,380 (20.2) | 1.0 | 4620 (17.1) | 4620 (17.1) | 1.0 | 6760 (22.9) | 6760 (22.9) | 1.0 |
| Severe CKD (eGFR <30mL/min/1.73m2) | 4008 (7.1) | NA | <0.001 | 2295 (8.5) | NA | <0.001 | 1713 (5.8) | NA | <0.001 |
| eGFR<30mL/min/1.73 m2 or eGFR 30–44mL/min/1.73m2 with UACR≥30mg/g or eGFR 45–59mL/min/1.73m2 with UACR>300mg/g | NA | 6680 (11.8) | NA | 3825 (14.2) | NA | 2855 (9.7) | |||
| SCORE≥10% | NA | NA | – | NA | NA | – | NA | NA | – |
| FH with ASCVD or another major risk factor | 581 (1.0) | 581 (1.0) | 1.0 | 292 (1.1) | 292 (1.1) | 1.0 | 289 (1.0) | 289 (1.0) | 1.0 |
| High risk, n (%) | 25,565 (45.3) | 26,755 (47.4) | <0.001 | 13,316 (49.4) | 13,750 (51.0) | <0.001 | 12,249 (41.6) | 13,005 (44.1) | <0.001 |
| Markedly elevated single risk factors (TC>310mg/dL, LDL-C>190mg/dL, or BP≥180/110mmHg) | 6147 (10.9) | 5826 (10.3) | 0.002 | 3254 (12.1) | 3125 (11.6) | 0.085 | 2893 (9.8) | 2701 (9.2) | 0.007 |
| Patients with FH without other major risk factors | 12,728 (22.6) | 12,580 (22.3) | 0.291 | 6384 (23.7) | 6325 (23.5) | 0.549 | 6344 (21.5) | 6255 (21.2) | 0.371 |
| Patients with DM without TODa, with DM duration ≥10 years or another additional risk factor | 17,042 (30.2) | 16,890 (29.9) | 0.324 | 8436 (31.3) | 8375 (31.1) | 0.571 | 8606 (29.2) | 8515 (28.9) | 0.409 |
| Moderate CKD (eGFR 30–59mL/min/1.73m2) | 12,364 (21.9) | NA | <0.001 | 6852 (25.4) | NA | 0.214 | 5512 (18.7) | NA | <0.001 |
| eGFR 30-59mL/min/1.73m2 with UACR<30mg/g or eGFR 45–59mL/min/1.73m2 with UACR 30–300mg/g or eGFR ≥60 with UACR>300mg/g | NA | 14,182 (25.1) | NA | 6978 (25.9) | NA | 7204 (24.4) | |||
| Score ≥5% and <10% | NA | NA | – | NA | NA | – | NA | NA | – |
| Moderate risk, n (%) | 9183 (16.3) | 7565 (13.4) | <0.001 | 4829 (17.9) | 4077 (15.1) | <0.001 | 4354 (14.8) | 3488 (11.8) | <0.001 |
| Score ≥1% and <5% | 6069 (10.8) | 5780 (10.2) | 0.005 | 3223 (12.0) | 3070 (11.4) | 0.040 | 2846 (9.7) | 2710 (9.2) | 0.055 |
| Young patients (T1DM<35 years; T2DM<50 years) with DM duration <10 years, without other risk factors | 5215 (9.2) | 5113 (9.1) | 0.292 | 2532 (9.4) | 2483 (9.2) | 0.468 | 2683 (9.1) | 2630 (8.9) | 0.446 |
| eGFR≥60mL/min/1.73m2 with UACR 30–300mg/gb | NA | 4076 (7.2) | – | NA | 1901 (7.1) | – | NA | 2175 (7.4) | – |
| Low risk, n (%) | 2115 (3.7) | 1413 (2.5) | <0.001 | 1128 (4.2) | 839 (3.1) | <0.001 | 987 (3.3) | 574 (1.9) | <0.001 |
| Score<1% | 2115 (3.7) | 1413 (2.5) | <0.001 | 1128 (4.2) | 839 (3.1) | <0.001 | 987 (3.3) | 574 (1.9) | <0.001 |
| eGFR>60mL/min/1.73m2 with UACR<30mg/g | NA | 0 | – | NA | 0 | – | NA | 0 | – |
Modified from original KDIGO as ESC includes 45–59 GFR as high risk category.
ASCVD: atherosclerotic cardiovascular disease; BP: blood pressure; CKD: chronic kidney disease; DM: diabetes mellitus; eGFR: estimated glomerular filtration rate; ESC: European Society of Cardiology; FH: familial hypercholesterolemia; KDIGO: Kidney Disease: Improving Global Outcomes; LDL-C: low-density lipoprotein cholesterol; SCORE: Systematic Coronary Risk Estimation; T1DM: type 1 DM; T2DM: type 2 DM; TC: total cholesterol; TOD: target organ damage.
These data indicate that including albuminuria into SCORE may improve the accuracy of this scale to better stratify CV risk. Of note, preventing strategies for the development and progression of CKD (renal function and albuminuria) with renin–angiotensin system inhibitors, and more recently, with sodium glucose cotransporter-2 inhibitors, have also shown a positive impact on CV disease.6–9 Therefore, an improved CV risk stratification may be helpful to better identify those patients that would benefit more from these therapies. In fact, the 2021 ESC guidelines on CV disease prevention have also include albuminuria in addition to renal function for CV risk stratification.10