Lupus nephritis (LN) is known to be one of the most serious complications of SLE and it is a major predictor of poor prognosis. Despite the improvement in understanding the pathophysiology of lupus nephritis and greater improvement in diagnostic approaches, lupus nephritis patients have poorer outcomes.
ObjectivesStudy the relation between renal resistive index (RRI) and renal function and histopathological parameters in lupus nephritis (LN) patients. Also to investigate the usefulness of RRI in predicting response to treatment.
Patients and methodsThis study included 126 patients who were split into two groups (group 1: 101 LN patients and group 2: 25 SLE patients without renal affection); and 100 healthy controls (group 3). The RRI was measured for all participants through a colored Doppler ultrasound examination. LN patients underwent renal biopsy and received their therapy and were followed up for 6 months.
ResultsThe RRI was significantly greater in the LN group (mean±SD; 0.64±0.07) than in SLE patients without nephritis (0.5884±0.04) (P<0.0001). The RRI was greater in LN class IV (P<0.0001). RRI significantly correlated with the chronicity index (r=0.704, P<0.0001), activity index (r=0.310, P=0.002), and serum creatinine (r=0.607, P<0.0001) and negatively correlated with eGFR (r=−0.719, P<0.0001). Almost eighty-five percent (84.8%) of LN patients responded to induction therapy. RRI was significantly greater in the nonresponder group (mean±SD, 0.73±0.02) than that in the responder group (0.63±.07) (P<0.0001). All non-responders to induction therapy while only 29.8% of responders had an RRI of ˃0.7. RRI, according to regression analysis was a significant predictor of response to treatment in LN patients.
ConclusionRRI was significantly greater in the LN group and significantly correlated with kidney function and histopathological parameters. RRI can predict response to induction therapy in LN patients.
Se sabe que la nefritis lúpica (NL) es una de las complicaciones más graves del LES y es un importante predictor de mal pronóstico. A pesar de la mejora en la comprensión de la fisiopatología de la nefritis lúpica y una mayor mejora en los enfoques de diagnóstico, los pacientes con nefritis lúpica tienen peores resultados.
ObjetivosEstudiar la relación entre el índice de resistencia renal (IRR) y la función renal y parámetros histopatológicos en pacientes con nefritis lúpica (NL). También investigar la utilidad del RRI en la predicción de la respuesta al tratamiento.
Pacientes y métodosEste estudio incluyó a 126 pacientes que se dividieron en 2 grupos (grupo 1; 101 pacientes con NL y grupo 2; 25 pacientes con LES sin afección renal); y 100 controles sanos (grupo 3). El RRI se midió para todos los participantes a través de un examen de ultrasonido Doppler color. Los pacientes con NL se sometieron a una biopsia renal y recibieron su terapia y fueron seguidos durante 6 meses.
ResultadosEl RRI fue significativamente mayor en el grupo NL (media±DE; 0,64±0,07) que en los pacientes con LES sin nefritis (0,5884±0,04) (P<0,0001). El RRI fue mayor en LN clase IV (P<0,0001). RRI se correlacionó significativamente con el índice de cronicidad (r=0,704, P<0,0001), el índice de actividad (r=0,310, P=0,002) y la creatinina sérica (r=0,607, P<0,0001) y se correlacionó negativamente con eGFR (r=−0,719, P<0,0001). Casi el ochenta y cinco por ciento (84,8%) de los pacientes con NL respondieron a la terapia de inducción. El RRI fue significativamente mayor en el grupo que no respondió (media±DE, 0,73±0,02) que en el grupo que respondió (0,63±0,07) (P<0,0001). Todos los que no respondieron a la terapia de inducción, mientras que solo el 29,8% de los que respondieron tuvieron un RRI de ˃0,7. RRI, según análisis de regresión fue un predictor significativo de respuesta al tratamiento en pacientes con NL.
ConclusiónRRI fue significativamente mayor en el grupo NL y se correlacionó significativamente con la función renal y los parámetros histopatológicos. RRI puede predecir la respuesta a la terapia de inducción en pacientes con NL.
Systemic lupus erythematosus (SLE) is one of the autoimmune diseases with multi-organ involvement, predominantly affects females in their reproductive age, and is characterized by remission and exacerbation courses.1–3 Lupus nephritis (LN) is a serious complication that affects about 40% of SLE patients,4 usually within 5 years of diagnosis, with a progression rate to chronic renal failure of 4.3–10.1%.5 Despite the improvement in understanding the pathophysiology of LN and greater improvement in diagnostic and therapeutic approaches, LN patients have poorer outcomes.6,7
A renal biopsy is known to be the gold standard for the diagnosis of LN because it gives information and details about the pattern and severity of kidney affection as well as the exclusion of other mimics of LN.6,8 Each of these factors weighs heavily on treatment choices.6,9 However, kidney biopsy is an invasive technique and it is contraindicated in some situations such as bleeding tendency.10 One study found that LN patients were five out of seven patients with severe bleeding following renal biopsy.11 During the course of the disease, multiple biopsies may be required to optimize treatment strategies.6,8,12
Grey abdominal ultrasound (US) examination is frequently the initial step in evaluating kidneys in many clinical situations from urinary abnormalities to kidney failure.2,13 US examination is simple, cheap, and non-invasive. However, renal US has some drawbacks, image acquisition, and interpretation are operator dependent.13
Doppler US examination is a non-invasive technique for studying kidney microcirculation. The renal resistive index (RRI) is considered one of the most important parameters in kidney Doppler US which is calculated utilizing the following equation: [(peak systolic velocity−end-diastolic velocity)/peak systolic velocity].13 It gives information about arterial compliance, peripheral resistance, and pulsatility, reflecting renal vascularity and parenchyma health status.13–16 Renal factors including renal interstitial and venous pressures have a significant impact on RRI.17 Increased RRI values could be a sign of renal scarring, which would then cause local renal vascular resistance to increase. Many investigators reported an increase in the RRI value in many renal diseases like obstructive nephropathy, acute renal transplant rejection, renal vein thrombosis, renal artery stenosis, chronic kidney disease, acute kidney injury as well as many parenchymal kidney diseases.2,18–20 Many previous studies which included heterogeneous populations (IgA nephropathy, diabetic nephropathy, kidney amyloidosis, LN) detected a significant association between RRI and tubulointerstitial and vascular abnormalities16,19,21,22 as well as glomerular lesions.2,16 To date, the usefulness of RRI in predicting response to treatment and prognosis of LN is controversial.
The goal of this study is to investigate the value of the RRI in the detection of renal affection in patients with SLE and to correlate between the RRI and kidney function parameters and histopathological parameters in LN patients. Also, this cohort study aimed to determine whether the RRI is a reliable predictor of therapy response.
Patients and methodsThis cohort study included 126 patients diagnosed as SLE patients who were admitted to the internal medicine department from January 2021 to March 2022. Also, 100 sex and age-matched healthy people who agreed to participate in this study were enrolled. The diagnosis of SLE was according to the 2019 European League Against Rheumatism/American College of Rheumatology Classification Criteria of systemic lupus erythematosus.23 The study included three groups as follows:
Group 1 included 101 LN patients.
Group 2 included 25 SLE patients without renal affection.
Group 3 included 100 sex and age-matched healthy people.
Group 2 and Group 3 were considered the control groups, while the LN group represented the study group. Patients with end-stage renal disease, obstructive nephropathy, diabetes mellitus, renal artery stenosis, hepatic diseases, heart failure, renal vein thrombosis, existing intra renal A-V fistula, other types of glomerulonephritis, and other autoimmune diseases were excluded. Ethical approval was obtained from the ethics committee of the Faculty of Medicine (IRB no. 17200343), ###. Before participating in our study, all patients and healthy controls provided their informed consent. The protocol of the study was registered in “ClinicalTrials.gov” under code NCT03958851. All participants were subjected to:
- 1.
History taking and physical examination.
- 2.
Laboratory investigation: urine analysis, serum creatinine (S Cr), blood urea nitrogen (BUN), estimated glomerular filtration rate (eGFR) measured by CKD-EPI Equation 2021,24 24h urinary protein excretion, complete blood counting (CBC) and serum albumin (Alb). These investigations were taken at the beginning of the study for all participants to distinguish the three groups of the study and every month for 6 months for the LN group.
- 3.
Doppler US was performed by a single radiologist utilizing the same machine (SONACEX6). It was performed for all participants (patients and controls). Doppler US for patients with LN was performed during hospital admission before the renal biopsy maneuver. The participants were examined in a supine or lateral position to make the US beam parallel to the direction of the blood flow in the intrarenal arteries. Waves were captured in the interlobar arteries or arcuate arteries throughout the study. The lowest pulse repetition frequency that would not produce artifacts was used to accept waveforms. The PSV, EDV, and RRI were calculated by the machine automatically. Three measurements from each kidney were taken and the average value was calculated to give the mean RRI for every participant.
- 4.
Renal biopsy was taken only for LN patients according to the recommendation of the American College of Rheumatology Guidelines 2012.25 Pathologists examined and reported on the kidney biopsy samples following the 2018 Revision of the International Society of Nephrology/Renal Pathology Society Classification for Lupus Nephritis.26
- 5.
The LN group was followed up for 6 months receiving the standard induction therapy as KDIGO guidelines 2012, 2021 recommended12,27 to monitor the outcomes of the induction therapy in patients with pathological RRI (RRI˃0.7) in comparison to those with RRI <0.7. In accordance with KDIGO guidelines 2021,12 complete response was defined as a decrease in proteinuria to less than 0.5g per day and improvement or stabilization of kidney function after 6 months from starting the induction therapy. Partial response was defined as a decrease in proteinuria by ≥50% of baseline proteinuria and improvement or stabilization of kidney function after 6 months partial responses. Response failure was considered when the previous criteria were not met after six months.
- 6.
Data interpretation and analysis: Version 23 of the statistical package for social sciences (SPSS) was used to interpret and analyze the data. Continuous data were described in terms of mean±standard deviation (±SD), however categorical data were expressed as frequencies and percentages. Student t-tests and Mann–Whitney U tests were used to compare quantitative variables for normally distributed data and non-normally distributed data, respectively. To compare three normally distributed quantitative variables, a one-way ANOVA test with post hoc analysis was utilized. Three non-normally distributed quantitative variables were compared using the Kruskal–Wallis test. The chi-square test was utilized to compare categorical data. The Exact test was utilized when the expected frequency was <5. Spearman's correlation and Pearson's correlation were used to identify the strength and direction of the association between ordinal and continuous variables. Logistic regression analysis was used to analyze the relationship between one dependent nominal variable and independent variables. Receiver operating characteristic (ROC) curve analysis was used to detect the best cut-off values of RRI to distinguish the lupus nephritis group from controls. P<0.05 was regarded as significant. If the P value was less than 0.000, it is reported as P<0.0001.
This study included 126 patients who were split into two groups (group 1: 101 LN patients and group 2: 25 SLE patients without renal affection); and 100 healthy controls (group 3). The mean±SD age of all study subjects was 27.45±4.7 years. The mean±SD BMI was 25.15±2.4.
Group 1 included 92 females (91.1%) and 9 males (8.9%), the mean±SD age of those patients was 27.79±5.63 years and the mean±SD BMI was 24.98±2.96. The median duration of the disease (SLE) was 6 months. The mean±SD serum creatinine was 196.8±201.9 (Table 1).
Demographic and laboratory findings of all enrolled cases (226).
| Lupus nephritis | SLE without nephritis | Healthy control | P-value | |
|---|---|---|---|---|
| Age* | 27.79±5.63 | 27.28±5.09 | 27.15±3.42 | 0.617 |
| Gender** | 0.646 | |||
| Male | 9 (8.9%) | 2 | 13 | |
| Female | 92 (91.1%) | 23 | 87 | |
| BMI | 24.98±2.96 | 25.79±1.46 | 25.15±1.88 | 0.320 |
| RRI* | 0.6428±.07 | 0.5884±0.04 | 0.5802±0.02 | <0.0001 |
| Duration of SLE (months)*** | 26.9±38.6 | 13.96±6.5 | – | 0.343 |
| Serum creatinine (μmol/L)**** | 196.8±201.9 | 69.72±8.57 | 59.32±5.79 | <0.0001 |
| eGFR (ml/min/1.73)* | 60.4±39.6 | 107±12.5 | 122.38±7.23 | <0.0001 |
| Hemoglobin (g/dl)* | 9.6±1.8 | 12.6±0.73 | 12.4±0.81 | <0.0001 |
| Serum albumin (g/L)* | 27.0±5.5 | 38.28±1.62 | 39.79±2.58 | <0.0001 |
| 24h urinary protein excretion (g/day)****mean±SD | 3.789±2.394 | 0.112±0.014 | 0.100±0.019 | <0.0001 |
| Median and range | 3.100 (0.883–14.400) | 0.112 (0.082–0.136) | 0.098 (0.040–0.130) | |
BMI: body mass index; eGFR: estimated glomerular filtration rate by 2021CKD-EPI creatinine equation; RRI: renal resistive index.
Group 2 included 25 SLE patients without renal affection: 22 females (88%) and 3 males (12%), with a mean±SD age of 27.28±5.09 years. The mean±SD BMI was 25.79±1.46. The median duration of the disease (SLE) was 15 months. The mean±SD serum creatinine was 69.72±8.57 (Table 1).
Group 3 (the healthy controls) included 13 males (13%) and 87 females (87%). The mean±SD age of healthy controls was 27.15±3.42 years. The mean±SD BMI was 25.15±1.88. The mean±SD serum creatinine is 59.32±5.79 (Table 1).
Age, gender, and BMI were not statistically significantly different between the study groups (Table 1). However, serum creatinine and 24h proteinuria were significantly greater in the LN group than in other groups (P<0.0001) also, eGFR, hemoglobin, and serum albumin were significantly lower in the lupus nephritis group than in other groups (P<0.0001) (Table 1).
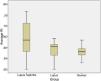
Renal resistive index in different groupsThe mean±SD RRI was greater in LN patients (0.64±0.07) compared to SLE patients without nephritis (0.5884±0.04) and healthy controls (0.5802±0.02) (P<0.0001) as was shown in Fig. 1. No significant difference in the mean RRI between group 2 and group 3 was present (P=0.479).
In LN patients: forty-one patients had RRI ˃0.7 (40.6%). A Tukey post hoc test revealed that the mean RRI in LN patients was greater in LN patients with eGFR <60ml/min/1.73 than in patients with normal eGFR (P<0.0001). RRI ˃0.7 was significantly greater in LN patients with eGFR <60ml/min/1.73 than in patients with normal eGFR (P<0.0001).
RRI and renin–angiotensin–aldosterone system inhibitors (RAASi)Out of the 101 LN patients, 65 patients (64.4%) received RAASi drugs while 36 (35.6%) did not due to reasons such as low eGFR, intolerance, or complications. The RAASi drugs used were ACEi like ramipril, ARBs as valsartan, and aldosterone receptor antagonists like spironolactone, with variable doses as tolerated. None of the controls (SLE patients without nephritis and healthy individuals), received RAASi drugs. The mean RRI was significantly lower in LN patients who received RAASi drugs (0.6±0.05) compared to those who did not (0.71±0.03; P<0.0001). However, there was no significant difference in mean RRI between RAASi-using LN patients (0.60±0.05) and non-RAASi-using SLE patients without nephritis (0.59±0.04; P=0.191).
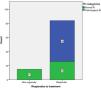
The biopsy results of lupus nephritis patientsThe biopsy results of the LN group (101 patients) revealed that 47 patients (46.5%) had class IV LN, 26 patients (25.7%) had class V LN, 6 patients had mixed class IV and V (5.9%), 11 patients (10.9%) had class III LN, 4 patients (4%) had mixed class III and V, 2 patients had class II LN (2%), 4 patients (4%) had mixed class II and V and only 1 patient had class VI LN. The chronicity index can range from 0 to 12, but in the biopsy results of our study, it ranged from 0 to 8, with a median of 2. Similarly, the activity index had a score ranging from 0 to 24, but in our study results, it ranged from 0 to 22, with a median of 5 out of 24. One-way ANOVA revealed a statistical difference in mean RRI between different histopathological classes of LN. A Tukey post hoc test revealed that the mean RRI was greater in class IV than in other classes (after exclusion of the only one case with class VI) (P<0.0001). Forty-one patients (40.6%) had pathological RRI (RRI˃0.7), thirty-five patients of them had class IV LN, four patients had class III LN, one patient had class V LN and one patient had class VI LN. So pathological RRI was significantly common in class IV as shown in Fig. 2 (P<0.0001).
Correlation between the renal resistive index and other histopathological and laboratory parameters (Table 2)A strong positive correlation between RRI and the chronicity index was detected. A moderate positive correlation between RRI and glomerulosclerosis, interstitial fibrosis, and tubular atrophy was found. A weak positive correlation between the RRI and the activity index was present. There was a moderate positive correlation between RRI and serum creatinine and blood urea nitrogen. A strong negative correlation between RRI and eGFRwas present. There was a moderate negative correlation between RRI and hemoglobin. There is no statistically significant correlation between RRI and age, duration of the disease, 24h urinary protein excretion, and serum albumin.
Correlation between renal artery resistive index (RRI) and continuous variables.
| Variable | Correlation coefficient (r) | P-value |
|---|---|---|
| Age | −0.007 | 0.941 |
| Duration of the disease | 0.019 | 0.85 |
| eGFR | −0.719 | <0.0001 |
| Activity index | 0.310 | 0.002 |
| Chronicity index | 0.704 | <0.0001 |
| Glomerulosclerosis | 0.605 | <0.0001 |
| Interstitial fibrosis | 0.629 | <0.0001 |
| Tubular atrophy | 0.629 | <0.0001 |
| Fibrous crescent | 0.272 | 0.006 |
| Hemoglobin level | −0.471 | <0.0001 |
| 24h urinary protein excretion | −0.068 | 0.497 |
| Serum albumin | −0.126 | 0.210 |
eGFR: estimated glomerular filtration rate.
The cut-off value for renal artery resistive index to differentiate lupus nephritis patients from controls was >0.58 with a sensitivity of 70.3%, specificity of 57.56%, and area under the curve (AUC) 0.734 (95% CI: 0.664–0.804, P<0.0001) as shown in Fig. 3.
Follow up after 6 months of treatment according to KDIGO guidelinesSixity three patients (62.4%) received steroids along with cyclophosphamide as induction therapy while thirty-eight patients (37.6%) received steroids plus mycophenolate mofetil (MMF) as induction therapy. Two out of 101 LN patients (1.9%) died within 2 months after starting treatment one due to pulmonary embolism and the second died due to severe pneumonia. Ninety-nine LN patients completed this cohort 84 patients of them (84.8%) responded to induction therapy and achieved either complete (60 patients) or partial remission (24 patients) after 6 months. Fifteen patients (15.2%) were non-responders to treatment, and three of them needed regular hemodialysis.
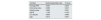
Follow-ups of patients revealed significant improvement in serum creatinine, BUN, eGFR, and hemoglobin, and 24-h proteinuria and serum albumin after induction therapy with P<0.0001 except in BUN P=0.011 as shown in Table 3.
Laboratory investigations (pre and post-treatment in lupus nephritis group).
The mean RRI in the nonresponders to induction therapy group was 0.73±0.02 and significantly greater than that of the responder's group (0.63±.07; P<0.0001). All non-responders to induction therapy had an RRI of ˃0.7 while 29.8%of responders had an RRI of ˃0.7 (P<0.0001) as shown in Fig. 4. The mean RRI was significantly greater in the patients who received cyclophosphamide (0.67±0.06) than those who received MMF (0.59±0.05; P<0.0001).
The chronicity index was significantly greater in the non-responders to induction therapy group than in the responder group (P<0.0001). Nine out of fifteen nonresponder patients (60%) had a chronicity index of ˃6/12, while only two out of eighty-four responder patients (2.4%) had a chronicity index of ˃6/12. But, there is no statistically significant difference in activity index between the non-responders to the induction therapy group and the responder group (P=0.347).
Univariate regression analysis revealed that high RRI, low eGFR and high chronicity index were significant predictors of poor response to treatment in LN patients as shown in Table 4. However, multivariate analysis, shown in Table 5, revealed that RRIs, chronicity index, and age were the only predictors of response to induction therapy in LN patients.
Possible predictors of response to induction treatment in lupus nephritis patients.
| Variable | Univariable odds ratio | 95% CI | P-value | |
|---|---|---|---|---|
| Lower | Upper | |||
| Average RRI | 0.000 | 0.000 | 0.000 | 0.007 |
| Chronicity index | 0.397 | 0.267 | 0.591 | 0.000006 |
| Activity index | 0.998 | 0.879 | 1.133 | 0.972 |
| eGFR | 1.107 | 1.047 | 1.171 | 0.0004 |
| 24h proteinuria | 1.00 | 1.00 | 1.00 | 0.362 |
| Serum albumin | 1.031 | 0.928 | 1.146 | 0.565 |
eGFR: estimated glomerular filtration rate at the beginning of induction therapy; RRI: renal resistive index.
Multivariate regression analysis of possible predictors of response to induction treatment in lupus nephritis patients.
| Variable | MultivariableOdds ratio | P-value |
|---|---|---|
| Average RRI | 0.000 | 0.036 |
| Chronicity index | 0.380 | 0.031 |
| Activity index | 0.866 | 0.261 |
| eGFR | 1.106 | 0.145 |
| LN classes | 0.865 | 0.880 |
| Age | 0.612 | 0.027 |
eGFR: estimated glomerular filtration rate at the beginning of induction therapy; RRI: renal resistive index; LN: lupus nephritis.
Few researchers examine RRI's role as a severity marker in patients with LN. To date, the usefulness of RRI in predicting response to treatment and prognosis of LN is controversial.
In this study, The mean serum creatinine was significantly greater in the LN group than in SLE patients without renal affection and healthy controls. This finding is consistent with earlier studies.2,28 and may be explained by the fact that 68% of the LN group biopsy results indicate LN class III and IV, and commonly patients with these classes have lower eGFR values.12,29
In this work, The RRI was significantly greater in the LN patients in comparison with SLE patients without nephritis and healthy controls. This finding is similar to many previous studies.2,28,30,31 This can be explained that RRI is affected by renal factors like increased renal interstitial pressure based on the idea that structural alterations in the kidney affect renal vascular resistance.17
In this study, the cut-off value for the RRI to differentiate lupus nephritis patients from controls was >0.58 with a sensitivity of 70.3%, specificity of 57.56%, and area under the curve (AUC) 0.734 (95% CI: 0.664–0.804, P<0.0001). El-Wakil et al. found that RRI at a cutoff of 0.77 (95% CI: 0.59–0.95, P=0.019) can differentiate between LN and the controls (healthy individuals and SLE patients without nephritis).28
In this work, RRI values in the LN patients were significantly greater in the LN patients with a lower level of eGFR (eGFR<60ml/min/1.73) than in patients with normal eGFR. Also, RRI ˃0.7 was more prevalent in LN patients with eGFR <60ml/min/1.73 than in LN patients with normal eGFR. This finding is in line with many previous studies2,22,31 and can be explained by the fact that patients with low eGFR had increased renal vascular resistance either due to increased interstitial pressure due to acute inflammation or advanced scarring of the renal parenchyma.
The use of RAASi drugs has been linked in several studies to a decrease in RRI values in individuals with a variety of renal diseases, however, the strength of this impact may differ according to the underlying disease, the drug type, and the dosage taken.32–35 In our study the mean RRI was significantly lower in LN patients who received RAASi compared to those who did not. However, there was no significant difference in mean RRI between RAASi-using LN patients and non-RAASi-using SLE patients without nephritis. The observed difference in RRI between RAASi users and non-users among LN patients could be primarily attributed to renal factors like increased interstitial pressure rather than the hemodynamic effects of RAASi drugs.
In the current study, the RRI is positively correlated with serum creatinine and BUN and negatively correlated with eGFR in concordance with many previous studies.2,19,30,31
In this study, there was a positive correlation between the RRI and chronicity index, interstitial fibrosis, and tubular atrophy. These results are nearer to the findings of Gao et al., who reported that LN patients with intermediate renal cortical fibrosis had RRIs that were considerably greater than those with a mild degree of fibrosis.30 But, the authors paid attention only to fibrotic scores. Our study findings differ from Conti et al., who reported no significant association between RRI and tubulointerstitial lesions.2 This discrepancy may be due to differences in study populations, as patients in our study had higher mean serum creatinine values, lower eGFRvalues, higher mean values for 24h urinary protein excretion as well as higher mean values for the chronicity index. Also, we found a positive correlation between RRI and activity index and this finding is in concordance with earlier work.2,31
Very few studies evaluated the relationship between RRI and histopathological classes. In our study, the most common LN class in biopsy results was class IV (46.5%) followed by class V (25.7%). This is a logical finding as class IV LN patients usually present with aggressive renal disease and patients with class V LN present with marked proteinuria,29 so a renal biopsy is usually recommended for those patients to confirm the diagnosis and determine the treatment strategy.
The mean RRI value was significantly greater in patients with class IV LN compared to patients with other LN classes. Forty-one patients (40.6%) had pathological RRI (RRI˃0.7), and the vast majority of them (87.8%) had LN class IV. These findings suggest that RRI may be a useful marker for classifying LN classes. Our study findings were in line with Conti et al. findings,2 who reported an association between higher RRI and LN class IV. They reported that RRI ˃0.7 was exclusively in class IV.2 Another recent study reported that pathological RRI is more common in class IV, V, and VI lupus nephritis than in other classes.31 Strong innate and cellular immune responses in class IV LN lead to the deposition and/or production of immune complexes in the subendothelial space. Cellular infiltration, the proliferation of intrinsic cells, and disruption of the glomerular capillary loop by cellular and fibrous crescents characterize the histopathologic lesions in class IV LN.26 This marked inflammatory process in class IV LN increased interstitial pressure and affect renal vascular resisitance.
To the best of our knowledge, no earlier work reported the value of RRI in predicting the response of LN patients to induction therapy. In our study, the RRI was significantly greater in the non-responders to induction therapy group than in the responder group (P<0.0001). Patients who received cyclophosphamide as part of their induction treatment protocol had considerably higher RRIs. This can be explained by that the patients who had low eGFR and had highly active lesions in the biopsy usually received cyclophosphamide in the induction therapy regimen. All non-responders to induction therapy had an RRI of ˃0.7 while only 29.8% of the responders had an RRI of ˃0.7. Many previous studies carried out on non-homogenous renal populations supported that RRI ˃0.7 was a predictor of poorer prognosis.15,36
The chronicity index was significantly higher in the non-responder to induction therapy group than in the responder group indicating irreversible chronic tissue damage. However, the activity index was not greater in the non-responder patients may be due to advances in treatment options or genetic variation.37
Univariate regression analysis revealed that high RRI, low eGFR and high chronicity index were significant predictors of poor response to treatment in LN patients. However, the multivariate regression analysis demonstrated that RRI, chronicity index, and age were found to be significant predictors of response to induction therapy. This suggests that when controlling for the impact of other independent variables, only RRI, chronicity index, and age remain predictors of treatment response in LN patients. A high chronicity index reflects irreversible tissue damage, increased interstitial pressure, vascular resistance, and increased RRI, all of which contribute to poorer treatment response. These results were consistent with Contreras et al.’s study,38 which reported that increased serum creatinine, as well as a high chronicity index, were linked to an increased risk of chronic renal failure or mortality in LN patients. Additionally, many researchers reported that older age at the time of diagnosis is associated with poorer outcomes and progression to end-stage renal disease.39,40
One of the drawbacks of the Doppler US examination is operator dependence. However, with the availability of modern and accurate devices, the improvement in radiologists’ experience in using this diagnostic modality, and the widespread use of Doppler US in medical fields, have minimized the operator dependence drawback of using Doppler US. All of these factors have raised the likelihood that the research on this emerging topic will be reproducible.
ConclusionRRI was significantly greater in the LN group and significantly correlated with serum creatinine, BUN,eGFR, chronicity index, and activity index. The most common LN class in biopsy results was class IV followed by class V. RRI was significantly greater in the LN class IV. RRI ˃0.7 was significantly common in class IV. Pathological RRI and chronicity index were significantly greater in the LN patients who did not respond to induction therapy than in the responders. So, RRI can predict response to induction therapy in LN patients.
Authors’ contributionsSamir Kamal Abdul Hamid: designed the study and interpreted the data.
Ashraf Elshazly: supervised the implementation and drafted the manuscript.
Yasser Abd Elmaugood Faisal: recruited patients, collected and analyzed data.
Kawsar Abdel Halim M.saleh: doing RRI measurement for study subjects and acquisition of data.
Mai Mostafa Aly: result interpretation and discussion, final approval of the version to be published.
All authors contributed to writing and editing the final manuscript.
FundingFor this work, the authors were not funded.
Conflict of interestThe authors have no competing interests to disclose.