Telemedicine used in nephrology has demonstrated non-inferiority to traditional care and acceptance by healthcare professionals and patients; however, cost effectiveness was less commonly reported. We aim to describe our centre's experience with virtual consultations (VCs) and estimate cost reduction, as well as assess general practitioners’ (GPs) perspectives.
MethodsRetrospective study of the patients referred for VC between January 2020 and December 2022 at Unidade Local de Saúde de Santo António (ULSSA). We analyzed patients’ demographics, including distance to hospital and autonomy, and estimated economic savings related to nephrologist's time, patient transport and lost workdays. To assess GPs’ perspective, we administered a brief, closed-question survey to GPs to assess awareness, use, and satisfaction with VCs.
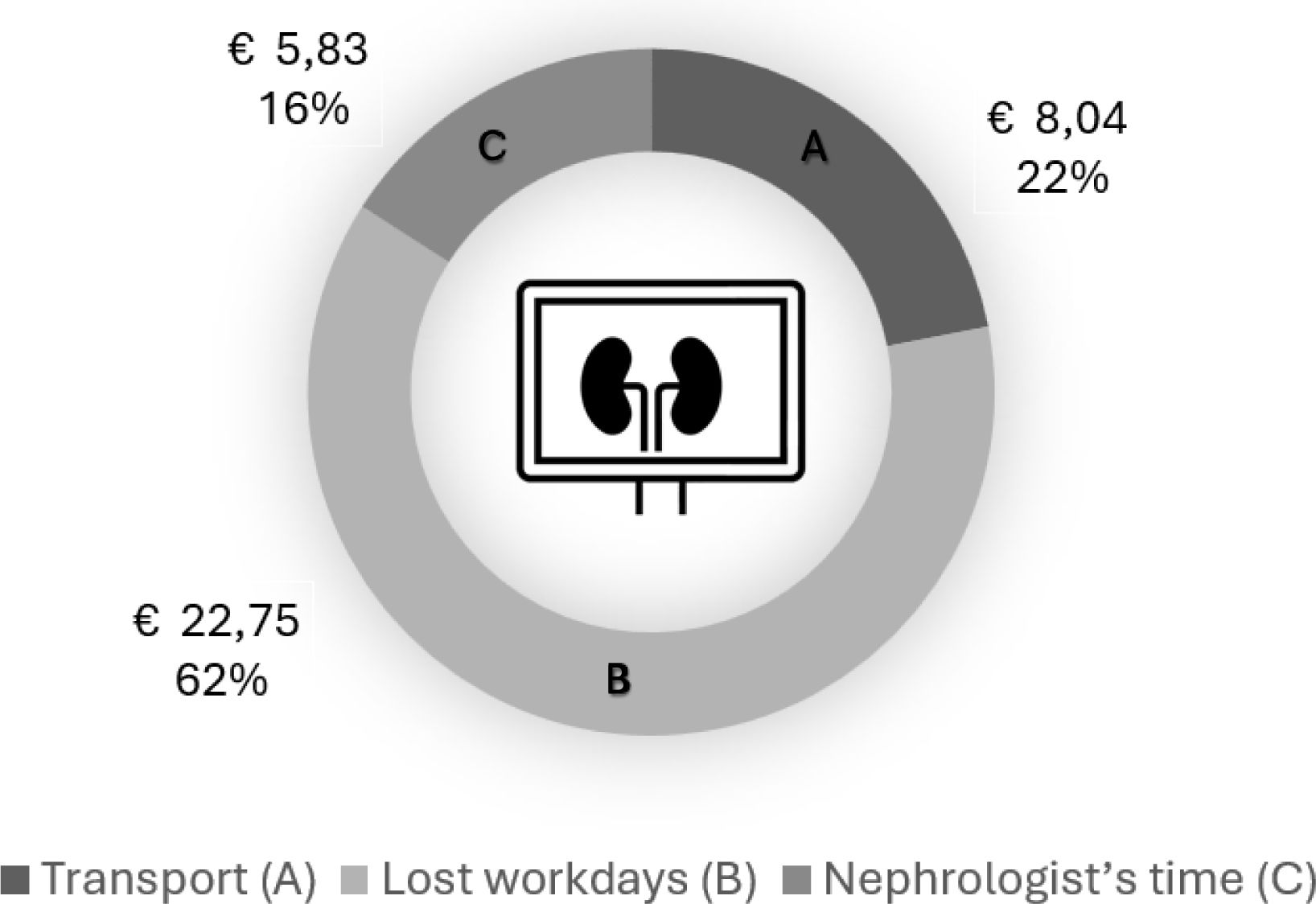
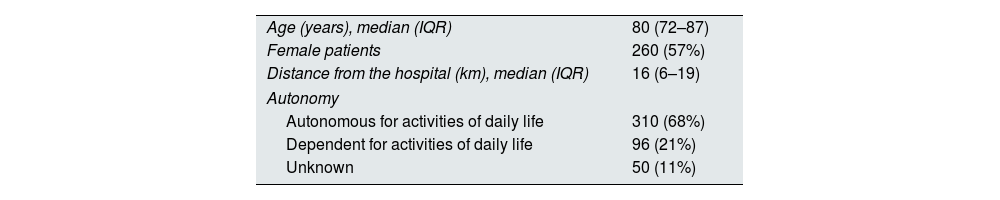
ResultsA total of 456 patients were included, of which 260 (57%) were female and median age was 80 years old (IQR 72–87). Distance from the hospital varied between one and 540km, with a median distance of 16km (IQR 6–19). Estimated total savings were €16,697.89, equivalent to €36.62 per patient per consult. The nephrologist time cost was estimated at €966.11 for virtual consultations compared with €3622.92 for initial face-to-face consultations, resulting in a time-related cost reduction of €2656.81. Forty-seven GPs of a total of 236 GPs (20%) completed the survey; from the responders, 28% had used VCs and 77% reported satisfaction with the response. Prescription guidance was the most identified strength of VC. Lack of awareness was the main barrier to use.
ConclusionsIn this single-center experience, VCs reduced costs and travel burden while being acceptable to GPs. However, many GPs were unaware of this pathway, underscoring the need for promotion and integration in primary-care workflows. Future multicentre studies should evaluate clinical outcomes including avoidable face-to-face visits, hospitalizations, time to advice) and include patient and nephrologist perspective.
La telemedicina utilizada en nefrología ha demostrado no inferioridad a la atención tradicional y aceptación por parte de los profesionales de la salud y los pacientes; sin embargo, la relación costo-efectividad se informó con menos frecuencia. Nuestro objetivo es describir la experiencia de nuestro centro con las consultas virtuales (CV) y estimar la reducción de costos, así como evaluar las perspectivas de los médicos generales.
MétodosEstudio retrospectivo de los pacientes remitidos para CV entre enero de 2020 y diciembre de 2022 en la Unidad Local de Salud de Santo António (ULSSA). Se analizaron los datos demográficos de los pacientes, incluida la distancia al hospital y la autonomía, y se estimaron los ahorros económicos relacionados con el tiempo del nefrólogo, el transporte de pacientes y los días de trabajo perdidos. Para evaluar la perspectiva de los médicos de cabecera, administramos una breve encuesta de preguntas cerradas a los médicos de cabecera para evaluar el conocimiento, el uso y la satisfacción con las CV.
ResultadosSe incluyeron un total de 456 pacientes, de los cuales 260 (57%) eran mujeres y la mediana de edad era de 80años (RIC: 72-87). La distancia desde el hospital varió entre uno y 540km, con una distancia mediana de 16km (RIC: 6-19). El ahorro total estimado fue de 16.697,89€, equivalente a 36,62€ por paciente y consulta. El costo del tiempo del nefrólogo se estimó en 966,11€ para las CV, en comparación con 3.622,92€ para las consultas presenciales iniciales, lo que resultó en una reducción de costos relacionados con el tiempo de 2.656,81€. Cuarenta y siete médicos de cabecera de un total de 236 médicos de cabecera (20%) completaron la encuesta. De los encuestados, el 28% había utilizado CV y el 77% informó satisfacción con la respuesta. La guía de prescripción fue la fortaleza más identificada de CV. La falta de conciencia fue la principal barrera para el uso.
ConclusionesEn esta experiencia de un solo centro, los CV redujeron los costos y la carga de viaje, al tiempo que fueron aceptables para los médicos de cabecera. Sin embargo, muchos médicos de cabecera desconocían esta vía, lo que subraya la necesidad de promoción e integración en los flujos de trabajo de atención primaria. Los estudios multicéntricos futuros deben evaluar los resultados clínicos, incluidas las visitas presenciales evitables, las hospitalizaciones, el tiempo hasta el asesoramiento, e incluir la perspectiva del paciente y del nefrólogo.
Chronic kidney disease (CKD) affected nearly 700 million individuals globally in 2017 and accounted for an estimated 1.2 million deaths, a number projected to rise to between 2.2 and 4.0 million by 2040.1 In 2022, end-stage kidney disease had an incidence of 243 per million people in Portugal, the second highest in Europe,2 taking a heavy toll on the national healthcare budget and leading to the approval in 2023 of the 2023–2026 National Strategy for the Promotion of Kidney Health and Integrated Care in CKD.3 In this document, telehealth is highlighted, particularly telemonitoring, with the objective of having at least 30% of the Portuguese nephrology departments implement remote monitoring program and digital tools of communication and education for patients.3 Despite growing recognition of telehealth's value, there are few publications about telehealth in Portuguese nephrology.4
Telehealth is a broad term used to describe all health related activities involving digital tools, including self-management applications,5 whilst telemedicine was defined by the World Health Organization as “the delivery of care services, where distance is a critical factor, by all healthcare professionals using information and communication technologies”.6 Recent interest in telemedicine in nephrology comes from the rising number of CKD patients and the need to improve access to specialist care, particularly in remote areas, with countries such as Canada, Australia and India being at the frontline for geographic reasons.7–10 More recently, the coronavirus 19 pandemic accelerated the adoption of telemedicine globally, as confinement measures highlighted its additional benefits, such as reducing infection risk.8,11 Other advantages of telehealth include cost reduction, sustainability and patient empowerment.7,12
One telemedicine tool frequently described is “virtual consultations” (VCs) or “e-consultations”. This term is applied with slight variations across literature it may simply be defined as electronic clinician to clinician communication.13 A definition that comes close to the program developed at Unidade Local de Saúde de Santo António (ULSSA) is the use of virtual clinics for triage and CKD management and to provide remote advice.14 In this study, we analyzed the characteristics of patients referred to this modality and the associated cost savings. To assess general practitioners’ (GPs) perspectives on this approach, we also developed and distributed a survey. Additionally, we examined the differences between GPs who were aware of the program and those who were not.
MethodsClinical model and study designUnidade Local de Saúde de Santo António is a Portuguese tertiary center with a catchment population of approximately 729,000. Although primarily responsible for this region, the hospital also receives referrals from outside its designated area, as patients may choose their center of care. The nephrology department includes a General Nephrology Clinic (GNC) that receives referrals from both primary care- via GP-other hospital clinics, post-emergency department visit and post inpatient discharge. Whilst all the hospital referrals are directed to face-to-face clinic, the electronic platform used by GPs for referrals offers the option of VCs, which requires informed consent of both GP and patient.
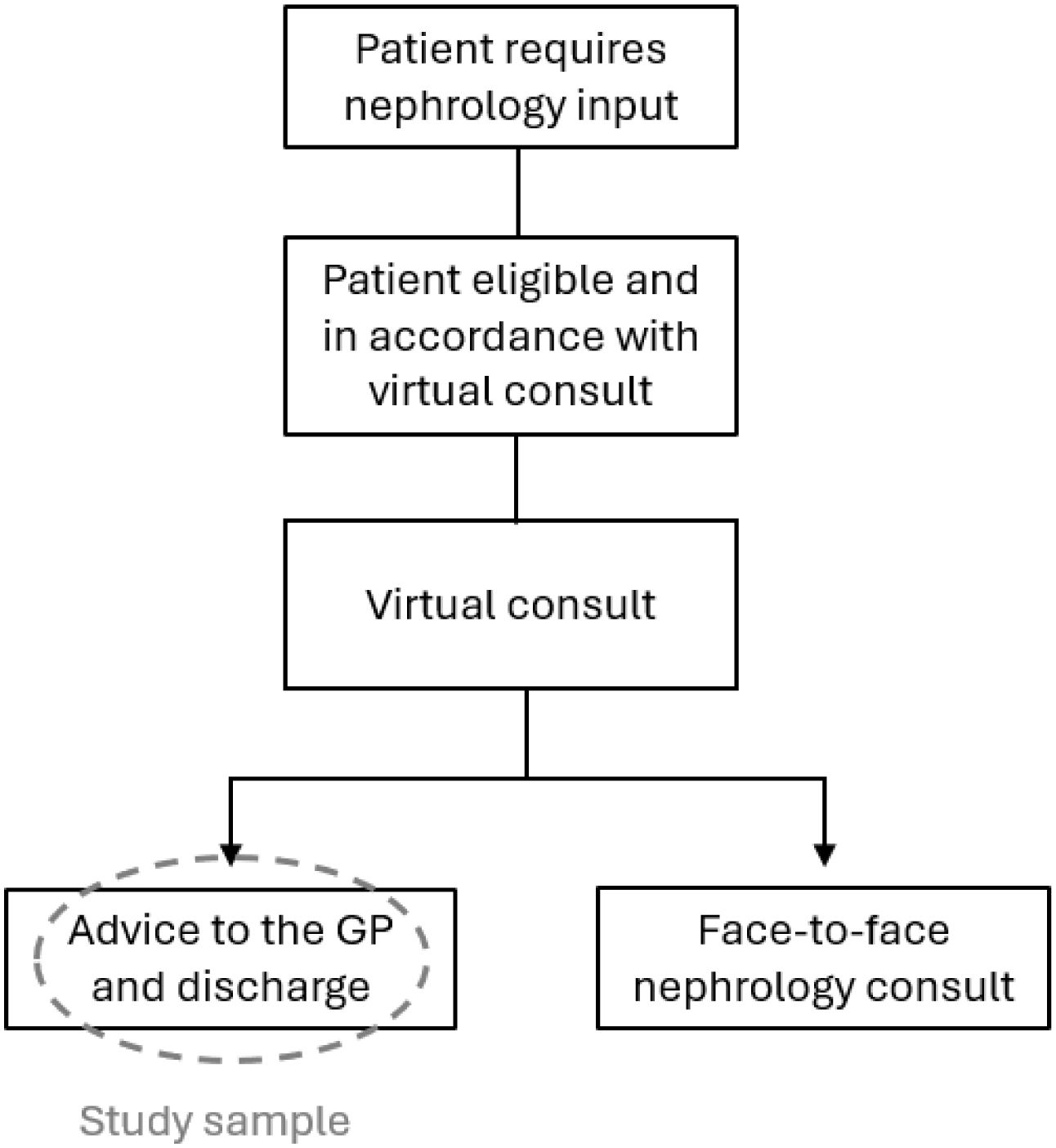
When VC is selected with informed consent from both GP and patient, a nephrologist reviews the patient's electronic health record (EHR) and either returns structured advice to the GP with recommendations to primary-care management and criteria to re-referral or converts to a face-to-face appointment (Fig. 1).
In terms of the digital platforms used and its’ technicalities, two key aspects enabled the VC project at ULSSA. Firstly, the platforms were the ones used at primary care centers and at ULSSA, nullifying costs with development, maintenance, security and encryption protocols, and concerns with user experience, systems interoperability and confidentiality issues. When making the referral, the option for VC, if it was available at the desired hospital and specialty, was on the form filled by the GP. The second key aspect was the “Registo de Saúde Eletrónico”, a national platform that integrates the EHR from the different hospitals and primary care centers, allowing complete health record review by the nephrologist and the communication of recommendations to the GP. The use of platforms that physicians were familiar with and the embedment of VC option in the existing GPs’ workflow eliminated the need to learn a new electronic system and additional work to make a VC referral.
This retrospective study reviewed the patients referred by the GP to the GNC that were managed through VC between January 2020 and December 2022. Other inclusion criteria were to be at least 18 years old, and to have an address registered in the EHR. We extracted demographic data (age, sex, address) autonomy (independent vs dependent), and travel distance (from registered address to ULSSA). Data were anonymised prior to analysis.
We estimated cost savings from patient transport, nephrologist time, and lost workdays. We based transport cost on the government stipulated price per km for transport of non-urgent patients at the time – 7.50€ for dislocations of 20km or less and 0.51€ per km after 20km. Distance between the patient's address and the hospital was based on Google Maps®.
We assessed whether the patients were able to come to clinic by themselves based on the EHR. This determination was established by either on explicit documentation or inferred from clinical notes – such as indications that the patient was bedbound, housebound, or fully dependent in activities of daily living, as reflected in recorded in frailty scales. Considering autonomy and the retirement age in Portugal in 2021, we determined how many patients were working at the time. The cost of a lost workday was estimated according to the average Portuguese wage in 2021 – 128,950€, as reported by the Portuguese Statistic Institute – divided by 22 workdays per month. We assumed that all the dependent patients would require a working-age chaperone to accompany them to clinic.
We determined the savings with nephrologist's worktime according to the time attributed to first face-to-face appointments (30min), the time spent by the nephrologist in each VC (approximately eight minutes) and the starting salary legislated by the Portuguese government for a specialist nephrology in 2021 (€15.89 per hour).
General practitioners surveyA brief, closed-question survey was designed with three sections and administered via Google Forms® to the GPs in the ULSSA catchment area, in a total of 236 medical doctors. The questionnaire consisted of three parts, the first recorded age, sex, years of practice and whether the GP had used the ULSSA's nephrology VCs before. Doctors who had used the system were taken to Section Two and asked about their experiences. Those who had not used the system were directed to Section Three where they were asked to indicate the reasons for not using it. Survey answers were timestamped but not linked to the e-mail address or identifying information, ensuring full anonymity.
The survey was intentionally brief and contained only closed questions, to stimulate a higher response rate. Although a longer questionnaire with open questions or a semi-quantitative design might provide a deeper understanding of the GPs’ perspectives, it would be more time and energy consuming, making it safe to assume a lower response.
AnalysisOur primary objective was to estimate the cost savings associated with nephrologist's work, patient transport and lost workdays. Additionally, we aimed to characterize key patient demographic and clinical features, as well as travel distance associated with hospital visits.
Regarding the GPs’ survey, we sought to assess their general perspective of VC and to evaluate whether there were differences between the GPs that used and did not use this tool. Since most GPs who had not used VC were simply unaware of its possibility, it was logical to study the differences between those who were aware of VC and those who were not.
Statistical analysisFor descriptive statistics, we used median (IQR) for continuous variables and absolute number (%) for categorical variables. Cost saving calculation was detailed above. For inferential statistics, we used Chi-square test for categorical variables and two tails t-test for continuous variables, considering a p<0.05 statistically significant. Data analysis was performed with Microsoft Excel®.
EthicsThe study was approved by the ULSSA's Ethics Committee and conducted in Declaration of Helsinki. Approval reference: 2025.172 (141-CAC/141-CE).
ResultsPatients’ characteristics and economic impact analysisA total of 456 patients were evaluated via VC, comprising 260 females (57%). Patient's age ranged from 22 to 100 years old, with a median age of 80 (IQR 72–87). After EHR review, 310 patients (68%) were classified as autonomous and for 50 patients (11%), autonomy status could not be determined. Since 310 of the 406 patients were clearly independent and 96 were not, we inferred that among the 50 patients with unknown status, 38 were likely autonomous and 12 were likely dependent. Travel distance to the hospital ranged between one and 540km, with a median of 16km (IQR 6–19). The cost nephrologist's work for the 456 VC was €966.11, whereas the cost of 456 first face-to-face consults would have been €3622.923 – reduction of €2656.11. The estimated total cost savings was €16,697.89 with an average cost saving of €36.62 per patient (Table 1) (Fig. 2).
Description of the study population and cost analysis.
| Age (years), median (IQR) | 80 (72–87) |
| Female patients | 260 (57%) |
| Distance from the hospital (km), median (IQR) | 16 (6–19) |
| Autonomy | |
| Autonomous for activities of daily life | 310 (68%) |
| Dependent for activities of daily life | 96 (21%) |
| Unknown | 50 (11%) |
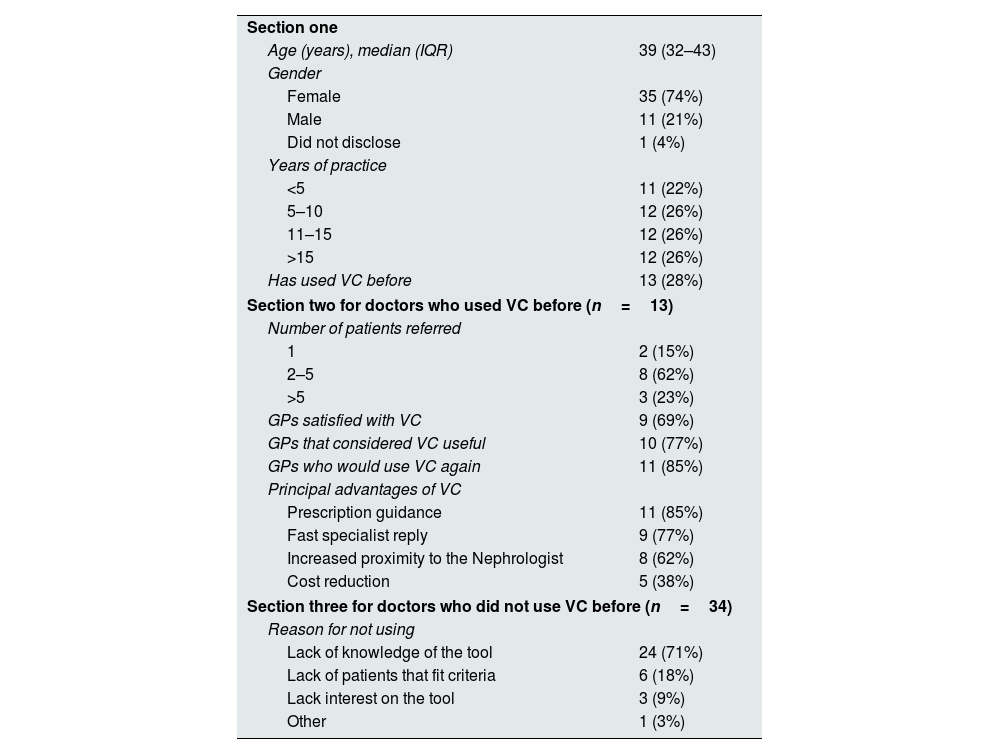
The survey was sent to 236 GPs, 47 GPs responded (74% female; median age 39 years, (IQR 32–43). Eleven doctors (22%) had less than five years of experience and 12 (26%) had more than 15 years of experience (Table 2).
Description of the surveys’ results.
| Section one | |
| Age (years), median (IQR) | 39 (32–43) |
| Gender | |
| Female | 35 (74%) |
| Male | 11 (21%) |
| Did not disclose | 1 (4%) |
| Years of practice | |
| <5 | 11 (22%) |
| 5–10 | 12 (26%) |
| 11–15 | 12 (26%) |
| >15 | 12 (26%) |
| Has used VC before | 13 (28%) |
| Section two for doctors who used VC before (n=13) | |
| Number of patients referred | |
| 1 | 2 (15%) |
| 2–5 | 8 (62%) |
| >5 | 3 (23%) |
| GPs satisfied with VC | 9 (69%) |
| GPs that considered VC useful | 10 (77%) |
| GPs who would use VC again | 11 (85%) |
| Principal advantages of VC | |
| Prescription guidance | 11 (85%) |
| Fast specialist reply | 9 (77%) |
| Increased proximity to the Nephrologist | 8 (62%) |
| Cost reduction | 5 (38%) |
| Section three for doctors who did not use VC before (n=34) | |
| Reason for not using | |
| Lack of knowledge of the tool | 24 (71%) |
| Lack of patients that fit criteria | 6 (18%) |
| Lack interest on the tool | 3 (9%) |
| Other | 1 (3%) |
Only 13 GPs (28%) had used VCs before, most had referred between two and five patients (n=8; 62%) and nine (77%) were satisfied with VCs. Among the GPs who had used VCs, the most frequent selected advantage was prescription guidance (n=11, 32%) and cost reduction was the least recognized benefit, mentioned only by five GPs (15%) (Table 2).
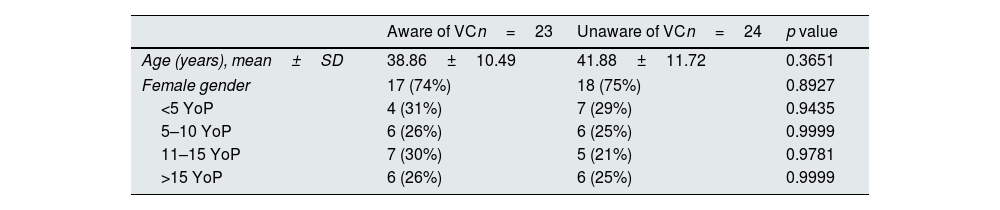
The most frequent reason for never using VCs was being unaware of it, corresponding to 24 of the 34 GPs that had not use it (71%). Given the considerable number of GPs who were unaware of the tool, we compared gender, age, and years of practice between those who were aware of it, regardless of whether they had used it, and those who were not. No statistically significant difference in age, gender or years of practice was found between the two groups (Table 3).
Comparison between GP who were aware and unaware of VC.
| Aware of VCn=23 | Unaware of VCn=24 | p value | |
|---|---|---|---|
| Age (years), mean±SD | 38.86±10.49 | 41.88±11.72 | 0.3651 |
| Female gender | 17 (74%) | 18 (75%) | 0.8927 |
| <5 YoP | 4 (31%) | 7 (29%) | 0.9435 |
| 5–10 YoP | 6 (26%) | 6 (25%) | 0.9999 |
| 11–15 YoP | 7 (30%) | 5 (21%) | 0.9781 |
| >15 YoP | 6 (26%) | 6 (25%) | 0.9999 |
YoP: years of practice.
We analyzed data from the nephrology VC at ULSSA, characterizing the referred patients and evaluating cost savings with nephrologist's worktime, hospital transport and lost workdays. We also surveyed GPs to understand their perspectives and compared the ones who were aware of this tool with the ones who were not.
Regarding the patients referred for VCs, most were older than 72 years and living within 20km of the hospital. We estimate savings of €36.62 per patient. These findings support that VCs allow for cost reduction in a population that lives close to the hospital and includes people of working and of advanced age.
Forty-seven GPs answered the survey. Despite all having access to VCs, only 13 (28%) had used it before and 24 (51%) were not unaware of it. There were no statistically significant differences in gender, age or years of practice between the doctors who were aware and unaware of this tool. Overall, GPs expressed satisfaction with VCs. The most valued benefit was receiving guidance on prescription, while cost reduction was considered the least important. These results suggest that VC is valued by GPs. However, in Portugal, the tool remains underrecognized and consequently underutilized and that effort should be put into promoting this consultation option. Due to the small sample size, we cannot rule out the possibility of differences between the GPs who are aware of this tool and those who were not.
Population: age, autonomy and distance to the hospitalOur study population differs from those in other studies: we had an older population who lived closer to the hospital.7,15–17 While largely focused on remote populations, particularly through video and telephone consultations, demonstrating non-inferiority to traditional care,15,18,19 the benefits of telemedicine in nephrology for patients living close to the hospital have been less emphasized. Our population was older; therefore, reduction of travel was just as important, especially considering increased frailty patients and those house or bedbound. On the other hand, for the patients of active age minimizing lost workdays is fundamental, regardless of distance to the hospital. Other benefits in both groups are avoidance of the anxiety associated with hospital visits and the psychological burden of managing a condition that requires hospital-based care.
This study included patients referred from most of Portugal's mainland, as demonstrated by the distance to center (between one and 540km), allowing for the inclusion of different backgrounds, including urban a rural, health literacy and general patient background. For this reason, we believe this is representative of the Portuguese population and that our VC model could be adapted to other Portuguese hospitals, especially considering the use of already in place digital platforms. Nevertheless, it would require a redistribution of the nephrologists’ time and roles. The extrapolation of these findings to other countries would require careful analysis of the healthcare systems, population's needs and characteristics, digital platforms and digital concerns, which is outside our scope.
Cost savingsWe estimate total savings of €36.62 per patient. Tan et al.18 compared cost with travel between video and face-to-face consults, finding a reduction of around $9.0 (approximately €7.82). AlAzab et al.20 based cost saving estimation associated with video consultations performed at a closer location to patients’ homes on patient survey, concluding that each face-to-face appointment would cost the patient on average JD73.0 (approximately €88.50); the cost per video consult is not indicated. George et al.7 studied the implications of a single nephrology consultation in an Indian population, including distance traveled, loss of productivity and need of chaperone, concluding that each visit costed the patient INR1350 (approximately €13.50). Mark et al.21 compared costs between face-to-face and virtual clinic follow up considering medical, nursing, pharmacy, administrative and other miscellaneous costs estimating minimum savings of £111.56 (approximately €128.67) per patient attendance associated with virtual clinic and £32.26 (approximately €37.21) for patients who only required advice to the GP. Other authors assessed the savings associated with virtual platforms of communication between GPs and Nephrologists with contradictory results: Van Gelder et al.19 found it to be more expensive than traditional care (€453.86 vs €433.74), whilst Scherpbier-de Haan et al.22 describe a cost reduction of €493 per referral. The variability of VC's characteristics between studies, country's context and cost analysis probably justifies the substantial differences between studies, nonetheless the cost reduction is not negligible in any of them. The fact that Van Gelder et al.19 found traditional care less expensive indicates that not all VC models are cost effective and suggests that further cost analysis is needed to determine which ones are.
Mark et al.21 study's savings of around €37.21 per patient that required only GP advice is probably the most comparable to our study. Considering that their analysis didn’t include lost workdays or travel expenses and that ours didn’t consider cost with nursing staff, administration and pharmacy, it is understandable that both underestimate the real cost per patient per consult and are indicative of higher savings with these types of VCs.
While reimbursement is a frequent topic in other papers in this area,12,23,24 Portugal healthcare follows a mostly Beveridge healthcare model, reducing the importance of this theme, and reinforcing the importance of cost reduction as a whole.
GPs perspectivesMost of GPs were satisfied with VCs (n=9, 77%), however to a lower extent than found in other series with similar platforms: a London virtual clinic had 96% satisfaction rate,25 an American one had 86.6% satisfaction rate.26 This may be due to more pronounced or perceived barriers by GPs in Portugal, such as increased workload, fear of substandard care and confidentiality issues, and suggests that further research, with stronger methodology and higher number of participants, in needed to confirm this and adapt our programs to our GPs’ needs.
For the GPs who used VC before, the most valued characteristic was prescription guidance. Schettini et al.26 found it to be a quick reply. Other studies with structured interviews and surveys name other advantages, such as improved access to specialist care, even for disadvantaged groups, educational opportunity, better communication between primary care and nephrologists, avoidance of unnecessary hospital referrals and visits and reassurance of a care plane.25,27,28 Given the methodology chosen, some of the advantages found by other studies were not evaluated in our study, leading us to believe that further studies are required for our GP's population.
The identification of prescription guidance as the most important aspect helped recognize an area of GPs’ education that might be improved. On the other hand, only five of the 13 GPs considerer cost savings important, perhaps because throughout medical training and practice cost efficiency is not a predominant concern in Portugal, which is a topic that also merits education reinforcement.
GPs unawarenessA search for “telemedicine” on PubMed, between 2009 and 2019 retrieved 23,890 papers, a number that grew to 42,750 between 2020 and July 2025. However, more than half of the GPs that answered the survey were not aware of nephrology VCs, which, considering the estimated cost reduction and growing literature was unexpected and poses as an opportunity for improvement. One option would be to use a software that identifies the patients who may need nephrological input and direct them automatically to a VC, yet authors exploring this found it increased the already overworked GPs’ workload.27 The involvement of GPs in the design of telenephrology tools might help integrate them in the existing workflow and increase usage.
LimitationsThis study has several limitations. First, regarding the characterization of VCs, it was a retrospective and descriptive analysis that did not include a direct comparison with face-to-face care, and cost analysis required necessary simplifications. Concerning the survey, selection bias is unavoidable, and we lacked data on non-responders. Only a small number of GPs replied, most of whom had not used the nephrology VC service. This suggests that the sample may not be representative of the GPs who have used the tool, especially considering that the number of VC referrals in our study exceeded those reported in other studies.22,29,30 Nonetheless, the survey provided valuable insight into the characteristics of GPs unfamiliar with nephrology VCs.
Future perspectivesIn this study, cost analysis was the main concern however, telemedicine and VC impact on patients’ outcomes, including hospital admissions and early diagnosis, merits investigation. We believe that our VC model contributed not only for the improvement of patient outcome by reducing waiting time from referral to nephrologist input and avoiding unnecessary hospital contact for those who did not need it, but also by reducing indirect health costs and leading to a more cost-efficient resource management.
A detailed analysis of patients referred for VC – such as comorbidities and reason for referral- and of the outcome of the VC – like advice given to the GP, need for later nephrology referral – would help tailor the existing VC model to our population and develop GP educational tools, further reducing the need for nephrology consults and empowering GPs. Additionally, our data contemplates only patients reviewed by VC and managed with advice to the GP, the patients that required a face-to-face consult were not included; by reviewing this group it would be possible to determine the number of unnecessary face-to-face referrals avoided and further understand the health and economic gains associated with VC.
Although we have included GPs perspectives in our analysis, the other two key elements of this equation- nephrologists and patients- were left out. Along with GPs’, patients’ views on different VC designs have been extensively analyzed, including confidence in VC, VC advantages, preferred methodology, overall satisfaction, concerns with risk of infection, loss of productivity, engagement in their own health, economic impact.7,8,31–33 The nephrologists seem to be the most neglected group, with their views being considered in less studies, and demonstrating access to the entire patient record, reduced time needed for each patient and reduction of unnecessary face-to-face consults being valued, whilst loss of patient contact, difficulty breaking bad news and patient's mistrust being pointed as barriers.25,34 Alongside with the analysis of patient's outcome, it would be important to comprehend our patients insights and opinions of this modality. As for the nephrologists, their intake and suggestions predictably would improve the current modus operandi of VC. Conciliating data of GPs’, patients’ and nephrologists’ perspectives of VC, in each region's context, would lead to the development of a personalized VC design that would expectedly translate into better health outcomes and economic value.
ConclusionNephrology virtual consultations can reduce costs and travel burden while being acceptable to GPs. Program visibility and primary-care engagement are crucial. Referral to VC by a Nephrologist lead to cost reduction associated with nephrological care, as well as reduced the difficulty of transport in an elderly population and the loss of productivity in a working one, regardless of distance to the hospital. These findings demonstrate value in this telenephrology tool. Although GP satisfaction was overall good, it was lower than the one found in other studies. Surprisingly, a considerable number of GPs were unaware of the availability of this tool, suggesting that further work for its dissemination and use is required. Future studies about clinical outcomes, patient and nephrologist's perspectives are required to further improve the already existing telenephrology tools, in particular VCs. Prospective multicentre studies should evaluate clinical outcomes and cost-effectiveness across diverse settings.
Conflict of interestThe authors declare no conflict of interest.