Nephrotic syndrome (NS) is a common disorder of childhood. The risk of thromboembolic (TE) phenomena in children with NS is estimated as 1.8–5% with a higher incidence in steroid resistant forms.1,2
Venous thrombosis is the most frequent type of thrombosis in childhood NS and occurs mainly in the deep venous system.3 Kerlin et al.4 reported 39 TE events among 326 NS patients and 29 of them were deep venous thromboses majority of which were seen in lower extremities. Although infrequent other sites like the cerebral venous system may also be affected and this presentation carries increased morbidity and mortality. Herein we present two children with minimal change disease (MCD) who experienced thrombosis of the cerebral sinovenous system.
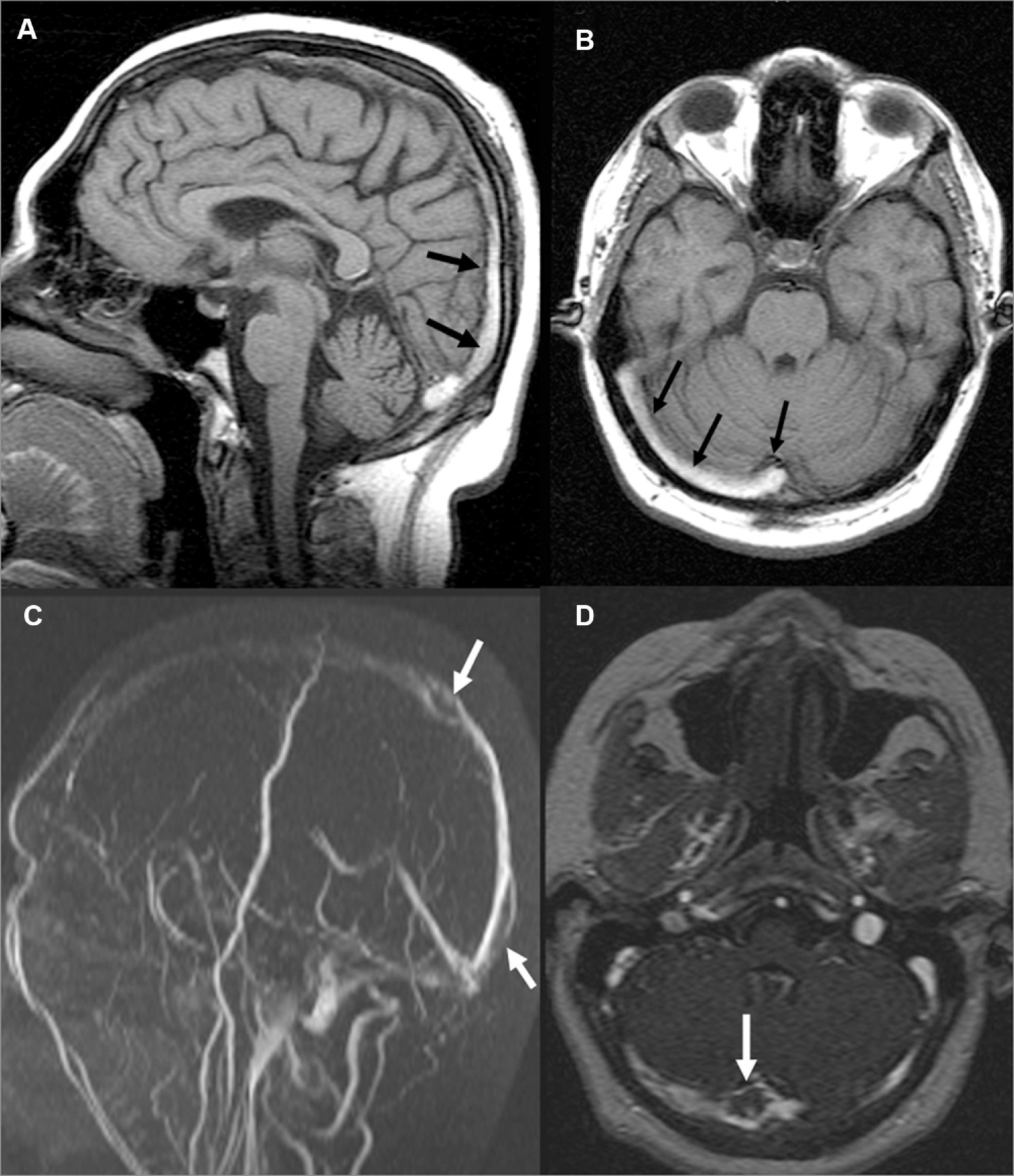
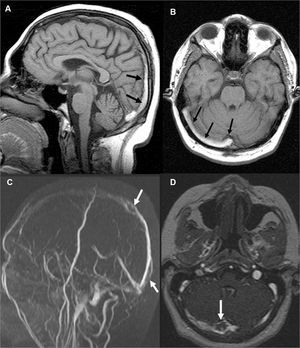
Patient 1A 15-year-old boy was admitted to our clinic with edema and 10kg weight gain in a month. Physical examination (PE) showed generalized edema and ascites. Urinary examination showed 246mg/m2/h proteinuria. Serum albumin level was 0.8g/dl, cholesterol and triglyceride levels were 375mg/dl and 190mg/dl respectively. Hemoglobin (Hb) level was 16.2g/dl. Renal biopsy was compatible with MCD. He was put on 60mg/day prednisone treatment and remission was achieved on the 22nd day. Steroid was used as 60mg/day for a month and tapered over 3 months. The day after cessation of prednisone generalized edema, headache and vomiting started. Laboratory investigations showed severe proteinuria, 1060mg/m2/h and a serum albumin of 0.8g/dl. His Hb level was 21.6g/dl and hematocrit (htc) 63.8%. He was put back on 60mg/day prednisone and intravenous fluid, albumin replacement, acetylsalicylic acid therapy were started. Cranial computed tomography (CT) was normal. Next day PE revealed lateral gaze palsy of the right eye. Cranial magnetic resonance imaging (MRI) and MR venography (MRV) were performed which showed subacute superior sagittal, right sigmoid and transverse sinus thromboses (Fig. 1A and B). Immediate anticoagulation with heparin was started. Investigations for inherited thrombotic risk factors were negative. On the third day of admission lateral gaze became normal. Two weeks later a repeat MRV showed partial recanalization of the thrombi (Fig. 1C and D). Remission of NS was achieved on the 35th day of steroid treatment, then the dose was decreased and the patient was put on cyclosporine. He had complete neurological recovery and did not experience recurrence of NS or thrombosis during the two-year follow-up.
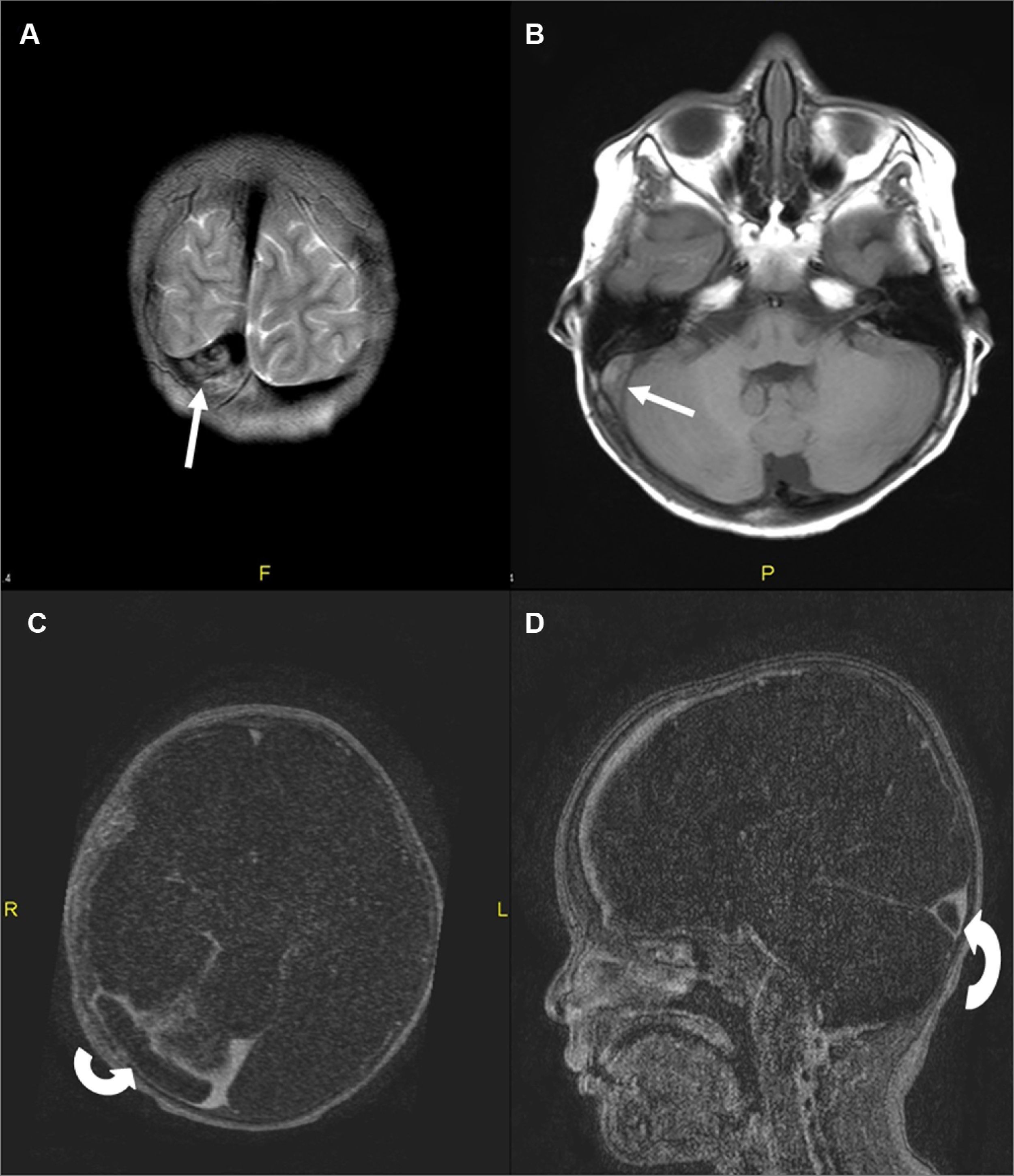
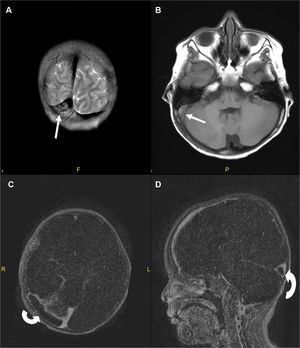
Patient 2A 2.5-year-old boy with no significant past medical history presented to our clinic with puffiness of the eyelids, edema of legs and decreased urine output. He had gained 2kg of weight in a week time. Physical examination revealed facial and pitting edema on extremities in addition to abdominal distension. Laboratory investigations showed Hb 14.9g/dl, htc 45.9%, platelet count 406,000/μL, total protein 3.7g/dl, albumin 1.4g/dl, serum cholesterol 382mg/dl and normal renal function tests. Urinary examination revealed heavy proteinuria; 244mg/m2/h. Serum C3 and C4 levels were normal. Nephrotic syndrome was diagnosed and the patient was put on 2mg/kg prednisone treatment. On the 4th day of treatment the patient complained of headache. Cranial CT was normal. On the 5th day he developed right 6th cranial nerve palsy. Magnetic resonance imaging and MRV showed thromboses in the superior sagittal, right transverse and sigmoid sinuses extending into the jugular system (Fig. 2). Intravenous hydration, low molecular weight heparin (LMWH) were started immediately. Screening for inherited thrombophilias was negative. On 10th day patient's headache subsided, focal neurological signs resolved. Remission was achieved on the 14th day of steroid treatment. The patient was discharged on steroid and LMWH. He had complete neurological recovery and has not experienced any complication during follow-up for 6 months.
Coronal T2-weighted (A) and transverse T1-weighted (B) MR images show hyperintense thrombus in transverse and sigmoid sinuses (arrows). Contrast-enhanced MR angiography axial (C) and sagittal (D) reformatted images demonstrate thrombus as hypointense filling defects in right transverse sinus (curved-arrows).
Cerebral sinovenous thrombosis is a rare but serious complication of NS with few isolated reports in the literature. Its incidence in children has been reported as 0.67/100.000 by the Canadian registry.5 The most frequent site reported for thrombus in CSVT patients is the superior sagittal sinus followed by the straight and the transverse sinuses.6 Appropriate imaging is necessary for timely diagnosis. In daily practice cranial CT is usually the preferred modality; however, it may miss CSVT in nearly 40% of patients.5 Magnetic resonance imaging with MRV is considered as the best method for the diagnosis and follow-up of pediatric CSVT.6
The hypercoagulable state in NS is due to several potential mechanisms; urinary loss of anticoagulant proteins, especially antithrombin (AT) III, increased procoagulatory activity, increased platelet aggregation and thrombocytosis.7 Hyperlipidemia may also be an additive factor.1 Other factors include hemoconcentration, diuretic use, severe hypoalbuminemia and indwelling catheters. Thrombosis in NS is mainly a secondary phenomenon but all children should be checked for hereditary thrombotic disorders. Our patients had no family history for TE events and thrombophilia panel testing was negative in both. Kerlin et al.4 recently reported TE events in 6.6% of patients with primary NS and showed severity of proteinuria, adolescent age (>12 years), and history of TE disease correlate well with TE risk. Our patients had MCD with heavy proteinuria and very low serum albumin levels during the attack. Hemoconcentration was a striking finding in one of our patients. The first patient was an adolescent; however, the second case was a 2.5-year-old boy. Thromboembolic complications are known to be more prevalent early in the disease course.8 A median time of 70.8 days from NS diagnosis to the first TE is recently reported in concordance with previous reports, 61% of the events occurring in the first 3 months just as in our patients.4
In the absence of major intracranial hemorrhage anticoagulation therapy is the preferred treatment in children with CSVT.9 There is no current consensus over the prophylactic use of anticoagulation and in daily practice it is not used unless patient has a thrombosis history.
Our cases highlight the importance of clinical suspicion and early diagnosis in NS patients with any neurological symptom. Careful physical examination, appropriate imaging, acute anticoagulation and proper treatment of the NS would reduce morbidity and prevent life threatening complications.