Objective: Hypertensive nephropathy is the second most common cause for starting renal repacement therapy in Spain with a steady incidence since 1997. Data on incidence of hypertensive nephropathy previously to dialysis are scanty because they are not registries similar to those used for renal replacement therapy. Design and methods: It have been retrospectively studied the records of our hospital Nephrology outpatients clinic from January, 1991 to December, 2007. Diagnosis was commonly made using clinical criteria in most of cases. There were 60 cases whith proteinuria higher than 1 g/day and so that renal biopsies were performed. Results: During this time 479 (44.0 pmp) patients were diagnosed of hypertensive nephropathy (mean age 66.6 ± 12.1 years and 43.0% were women). Incidence increased from 33.3 pmp (1991) to 76.2 pmp (2006). There was a steady trend to increase incidence since 16.7 pmp in 1991 up to 89.5 pmp in 2007. Mean incidence was 31.8 pmp between 1991 and 1995, 32.1 pmp in the period 1996-2000; and 54.4 pmp from 2001 to 2006. The mean age of incident patients have showed a J curve. 53 subjects (11.6%) have started renal replacement therapy. Survival before starting renal replacement therapy was 96.0 at first year, 85.9% at five years and 81.6% after seven years of follow-up. Conclusions: Incidence of hypertensive nephropathy seems to have increased last years specially in spite of therapeutic improvements the prognosis is still unfavourable. Less rectricted age criteria for submitting patients may have influenced these results.
Objetivo: La nefropatía hipertensiva es la segunda causa más común de entrada en tratamiento renal sustitutivo en España, con una incidencia que parece estable desde 1997. Los datos sobre incidencia de nuevos diagnósticos de nefropatía hipertensiva en consulta son escasos al no existir registros similares a los usados en el tratamiento renal sustitutivo. Diseño y métodos: Se ha revisado retrospectivamente la incidencia de este diagnóstico en la base de datos de la Consulta de Nefrología del Hospital Infanta Cristina de Badajoz entre el 1 de enero de 1991 y el 31 de diciembre de 2007. El diagnóstico se hizo en la mayor parte de los casos por criterios clínicos. En 60 casos se realizó biopsia renal por proteinuria superior a 1 g/24 h. Resultados: Durante ese tiempo fueron atendidos en consulta 5.071 pacientes, de los cuales 479 fueron diagnosticados de nefropatía hipertensiva. La incidencia media de nefroangioesclerosis ha sido 44,0 casos pmp, con una edad media de 66,6 ± 12,1 años, siendo el 43,0% mujeres. Se aprecia una tendencia progresiva desde 16,7 pmp en 1991 hasta 89,5 pmp en 2007. Las tasas medias fueron 31,8 pmp en el período 1991-1995; 32,1 pmp entre 1996 y 2000, y 54,4 en el período 2001-2006. La edad media de los pacientes incidentes a lo largo del período estudiado ha seguido una curva en «J»; 53 pacientes (11,6%) han iniciado tratamiento renal sustitutivo durante estos años. La supervivencia estimada antes de llegada a tratamiento renal sustitutivo fue el 96,0% al año, el 85,9% a los 5 años de seguimiento y el 81,6% a los 7 años de seguimiento. Conclusiones: La incidencia de nefropatía hipertensiva parece tender a crecer significativamente en los últimos años a pesar del perfeccionamiento de los tratamientos preventivos utilizados. La mayor permisividad en la edad para la derivación podría influir en estos resultados.
INTRODUCTION
Nephroangiosclerosis or renal damage of hypertensive origin was first described in 1914 by Volhard and Fahr.1 Various epidemiological studies have demonstrated that high blood pressure (HBP) is one of the main risk factors for the onset and progression of chronic nephropathy.2 It has been estimated that the relative risk of developing chronic nephropathy, where hypertension exists in the absence of other cardiovascular risk factors, is 57% higher.3 If we take into account the magnitude of the prevalence of HT worldwide, hypertensive nephropathy is evidently a public health problem that needs to be addressed.
The incidence of hypertensive nephropathy, measured as the percentage of patients with this diagnosis and corresponding to the total number of patients who initiate renal replacement therapy (RRT), showed a significant increase in Spain at the end of the 1990s. Whereas renal vascular disease was a minor cause of patients initiating RRT in comparison with idiopathic glomerulonephritis4 in 1990, in 1999 it was the most common cause of inclusion in a dialysis programme in patients over 65 years of age (21% of this patient group), according to data published by the Comité de Registro de la Sociedad Española de NEFROLOGÍA (Registry Committee of Spanish Nephrology Society) in collaboration with various Regional Registries.5 The data facilitated in subsequent years does not appear to indicate that this situation has changed much (17% of the total number of cases) and confirms a greater incidence in the over 75 age segment (24.4% of cases receiving RRT).6 This situation is still nothing like that reflected by data from the United States, where it affects nearly 35% of all new patients.7
There is very scanty data on the incidence of hypertensive nephropathy in patients treated in the outpatient nephrology clinics despite the importance of this issue. The aims of this study were to review the annual incidence of hypertensive nephropathy diagnoses in our department during the period from 1991 to 2006 and to evaluate the prognosis for the disease in Spain.
DESIGN AND METHODS
The database of the Nephrology Department of the Infanta Cristina Hospital, in which the final diagnoses of all the patients seen since October 1990 are stored, was reviewed retrospectively. The data search covered the period from 1 January 1991 to 31 December 2007. The incidence of diagnosed cases of hypertensive nephropathy during that period was analysed. In the majority of cases the diagnosis was made using clinical criteria based on a history of HT and/or previous cardiovascular diseases. Other possible renal diseases were excluded using standard diagnostic protocols.8 In cases in which proteinuria was higher than 1g/day a renal biopsy was performed to confirm the diagnosis, as long as the patient had given his/her consent.
The general characteristics of the patients are shown in table 1. Female patients showed a higher body mass index, a greater prevalence of abdominal disease and a greater frequency of renal failure from the outset.
According to figures from the Spanish Institute of Statistics, the population of the province of Badajoz was 676,936 in 1990 and 672,029 in 2008. The population has fluctuated during this period, reaching a minimum of 650,938 people so the incidence per million inhabitants for a health area of approximately 660,000 people from 1991 to 2001 (corresponding to the entire population of the province of Badajoz) was calculated. The Nephrology Unit of the Hospital of Zafra Area, responsible for a health area with a population of approximately 135,000 people, began to operate in 2002 so the incidence rates have been calculated for a population of 525,000 from 2002 to 2007. The few patients referred from the area of Zafra after that date have not been included in the study.
The continuous variables are expressed as the mean (standard deviation). The frequency variables were compared using Fisher’s exact test and the chi-square test. The continuous variables were compared by means of the Student’s t-test for independent samples, after confirming the normality of their distribution using the Kolmogorov- Lilliefors test. The survival of patients was calculated by means of the Kaplan-Meier method, using end-stage kidney disease as the censor variable (creatinine clearance < 15ml/min, stage V of the KDOQI guidelines) or the initiation of renal replacement therapy. The SPSS software programme (version 13.0) was employed for the statistical calculations. The results are expressed as the mean ± standard deviation or median ± standard deviation.
RESULTS
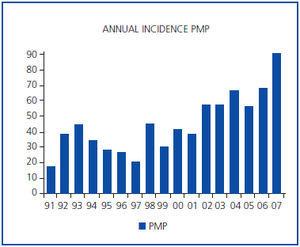
During this time the total number of patients seen for any reason in the department was 5,071. 479 of these were diagnosed with hypertensive nephropathy, in accordance with the criteria described in the previous section. The mean incidence of nephroangiosclerosis throughout the entire period under consideration was 44.0 pmp and the mean age was 66.6 ± 12.1 years. 43.0% of the patients were female and 57.0% were male. In 60 cases the diagnosis of hypertensive nephropathy was confirmed by renal biopsy. A progressive tendency was observed, rising from 16.7 pmp in 1991 to 89.5 pmp in 2007. The mean rates were 31.8 pmp during the period 1991-1995, 32.1 pmp from 1996 to 2000 and 54.4 during the period from 2001-2006 (figure 1).
The mean age of patients with hypertensive nephropathy during the period under study followed a «J» curve distribution (the mean ages per year are presented in figure 2. The mean for the period 1991-1995 was 69.0 ± 13.9 years, which fell during the period 1996-2000 to 65.4 ± 10.6 years (p = 0.039) and increased again during the period 2001-2007 (67.0 ± 11.2 years), but without reaching statistical significance. However, the rates adjusted for age show an increase in the incidence of the disease above the age of 50 and 70 years (table 2). When the incidence was compared differentially for sex, the incidence of male patients grew in the latter period, but failed to reach statistical significance (p = 0.077, chisquare test) (table 2).
The data corresponding to patients who started to receive treatment in the department from 1 January 1990 to 31 December 2001 was used to calculate survival. Altogether there were 378 patients, 53 of whom (14.0%) had reached stage V renal failure or started RRT during this period.
The estimated mean survival was 194.0 ± 16.3 months and the actual mean survival 169.0 ± 18.0 months. The survival curve can be seen in figure 3. The estimated survival was 96.0% after one year, 85.9% after 5 years of follow-up and 81.6% after 7 years of follow-up.
DISCUSSION
Hypertensive or vascular nephropathy is now the second cause of entering RRT in Spain. However, our data suggests that the incidence will be even higher in the years to come, approaching the levels of countries such as the United States. Although the development of the disease does not appear to be rapid or progressive in most cases evaluated in this study, the enormous prevalence of HT and other cardiovascular risk factors in Spain9 means that the number of patients who go on to develop end-stage renal disease will finally be higher than we might expect on the basis of the functional survival of the patients in the study. In spite of everything, it is important to point out that the survival before initiating RRT for the series we studied is better than that observed in the case of diabetic nephropathy, the outcome of which in our department has previously been published.8 However, despite the relatively good prognosis in terms of the progressive tendency of this renal disease, we need to remember the poor prognosis for this patient group with respect to the appearance of a wide range of cardiovascular events.10
Practically no data has been published in Spain about the incidence of vascular nephropathy, apart from data obtained from the records of patients starting RRT. 39% of the patients included in the COPARENAL11 study had been diagnosed with hypertensive nephropathy, but the methodological differences were considerable. This study included patients who met two diagnostic criteria: HT (in other words, a very high percentage of patients seen in the department were excluded) and renal failure (which, in this case, would also exclude a vast number of patients). Included in the statistical figures used in the department, there were many patients who had neither HT nor renal failure.
It is difficult to define the data collection area in the case of the majority of our nephrology services, except when they correspond to a single province, as in our case, and when there is little movement of immigrants into the region and, consequently, few patients who have been referred from other parts of Spain or other parts of the world. Although the health area Badajoz caters for has been divided up throughout the period covered by the present study, from routine records it is easy to determine when a patient is from another health area. Moreover, the closed structure of the health system makes it enormously difficult, when not absolutely impossible, for patients to receive treatment outside of their health area, which has previously been designated by the Spanish Health Service. It is more or less the same for the other province in the region, which, for the same reason, seldom receives patients from other health areas. So we can safely say that the rates of hypertensive renal disease that we have observed correspond to the real figures. This is important because, unlike our region, regions which receive a lot of immigrants of Latin American or African origin may have even higher levels of hypertensive nephropathy, given that these populations are more predisposed to the development of renal disease, according to epidemiological calculations.4 Consequently, the application of this data to the Spanish population in the rest of the country is a reasonable proposal, although we cannot be absolutely certain of its accuracy.
The main limitation of the study lies in the diagnostic criterion for nephroangiosclerosis. As there is no specific marker, such as an association with proteinuria and retinal lesions, which occurs in diabetic nephropathy, the diagnosis of nephroangiosclerosis is made by excluding other renal processes and on the basis of a history of cardiovascular risk or previous cardiovascular disease affecting another part of the body, for example ischaemic coronary heart disease. Ideally, the diagnosis of hypertensive nephropathy would be based on a renal biopsy in all cases, but this would imply the inevitable risk which the performance of the technique entails and a significant increase in workload. Generally speaking, as in our study, biopsy is reserved for patients with intense proteinuria to rule out the diagnosis of glomerulonephritis or when the latter fails to respond sufficiently to hypotensive treatment. However, it may be the case that the opposite miscalculation has occurred; in other words, that cases of renal failure of different origin have been counted as patients with hypertensive nephropathy. However, autopsies on patients who have had a fatal cerebrovascular accident demonstrate a significant lack of nephroangiosclerotic lesions (40%) in comparison with patients who have died as a result of other neurological disorders.12
Microalbuminuria is a phenomenon which is often associated with HT13 and it is believed to precede the development of hypertensive renal disease.14 Patients referred with microalbuminuria have not been included in the diagnoses of hypertensive nephropathy if there was no concomitant renal failure. There are two reasons for this: the first is that the determination of microalbuminuria was virtually unavailable as part of primary care from 1990 to 2000; to include these patients would have introduced bias into the results, given that it would have meant an even greater increase in the incidence of nephroangiosclerosis in these patients, simply as a result of the improvement in the diagnostic techniques at our disposal. The second reason is that microalbuminuria is not a criterion for referral to the nephrology department, except when there is no response to treatment. Therefore, most patients with microalbuminuria are not referred to the department (if they were, there would be more of these patients than patients with proteinuria and/or renal failure).15,16
The true incidence of hypertensive nephropathy must certainly be higher than our study indicates, since the primary inclusion criterion was that patients had been treated at the nephrology department and some patients will not have been referred to the department (at least in the earliest phases of their disease) or will not have wanted to come for various reasons, for example their age or the fact that they live a long way from their health centre. The criteria for referring patients with clinical proteinuria or renal failure have not changed during this period. However, the commotion amongst the medical community caused by the popularity of the concept of “hidden” renal failure and the fact that laboratory reports include glomerular filtration values which are estimated from creatinine levels using formulas derived from the MDRD (Modification of Diet in Renal Disease) study will undoubtedly have had some influence on the increase in the number of patients detected in recent years.17
Age per se, in other words population ageing, may also have affected the results. On one hand, the census shows that the population has aged; on the other, the referral criteria may have been modified, temporally extending the age limits. Nevertheless, it is surprising that the number of cases of nephroangiosclerosis continues to grow when the level of control, knowledge and treatment of HT has improved in Spain.18 This contrasts with statistics which demonstrate a reduction in cardiovascular morbidity and mortality related to other target organs.19 However, it is possible that better control of HT and lower mortality of cardiovascular origin are the cause underlying the increase in the number of patients receiving treatment for hypertensive nephropathy. So a greater number of patients might eventually develop clinical or subclinical renal dysfunction, given that, otherwise, they would have died before any renal injury became evident.
In conclusion, the incidence of hypertensive nephropathy at the nephrology department continues to rise over time, a finding which is probably related to the ageing of the population. However, the rate of progression to renal failure seems to be relatively low, especially in comparison with diabetic nephropathy. It is to be expected that there will be a progressive increase in the numbers of these patients at nephrology departments in the future.
Table 1. General Characteristics
Figure 1. Number of cases of nephroangiosclerosis observed per year.
Table 2. Incidence Distributed according to Age
Figure 2. Mean age of patients diagnosed with hypertensive nephropathy each year.
Figure 3. Statistical Survival Curve until Inclusion in Renal Replacement Therapy or Stage V of the KDOQI Guidelines SURVIVAL UNTIL TCRI in Months (Kaplan-Meier)