Introduction: The use of solutions containing hypertonic glucose (3.86%/4.25%) has been postulated as the method of choice for study the peritoneal function, and permits a better evaluation of the ultrafiltration (UF) capacity. Objective: The aim of our study was to analyze the UF capacity and its relation with the peritoneal permeability and sieving of sodium, performing the peritoneal kinetic study with hypertonic glucose solutions. Patients and methods: We performed 184 peritoneal kinetic studies with hypertonic glucose solutions in stable patients on peritoneal dialysis (PD), with a mean time on PD of 16 ± 22 months. We measured the mass transfer coefficient of creatinine (CrMTC), dialysate to plasma ratio of creatinine (D/PCr), UF capacity and sieving of sodium at 60 minutes (difNa60). Results: The mean values were: CrMTC: 9.1 ± 4.5 ml/min, D/PCr: 0.71 ± 0.09, UF 759 ± 233 ml/4 h and difNa60: 4.7 ± 2.3. The best multivariate model that predicts the UF capacity included: difNa60, CrMTC, age and time on PD (r = 0.57; p >0.0001). In patients with UF lower than 600 ml/4 h (Percentil 25) the correlation between UF and CrMTC was lost, but remains the correlation with difNa60 (r = 0.48). The patients with previous peritonitis (n = 38) showed no differences in UF, CrMTC or D/Pcr, but the had lower difNa60 (3.7 ± 2.8 vs. 4.9 ± 2.1; p = 0.002) than the remaning patients. Conclusions: The peritoneal kinetic study performed with hypertonic glucose allows to standarize the UF capacity and by determination of sieving of sodium, the early detection of water transport alterations, before the UF capacity and small solutes permeability alteration develops.
Introducción: La utilización de soluciones con glucosa al 3,86%/4,25% se ha postulado como el método ideal para estudiar la función peritoneal, ya que permite evaluar mejor la capacidad de ultrafiltración (UF). Objetivo: El objetivo del estudio es analizar la UF y sus relaciones con la permeabilidad peritoneal y el cribado de sodio mediante la realización de cinéticas peritoneales con glucosa hipertónica. Pacientes y métodos: Realizamos 184 cinéticas con glucosa hipertónica en pacientes estables en diálisis peritoneal (DP), con un tiempo medio en DP de 16 ± 22 meses. Se midieron el coeficiente de transferencia de masa de creatinina (MTCcr), el cociente dializado/plasma de creatinina (D/Pcr), la UF y el cribado de sodio a los 60 minutos (difNa60). Resultados: Los valores medios fueron: MTC-Cr: 9,1 ± 4,5 ml/min, D/Pcr: 0,71 ± 0,09, UF 759 ± 233 ml/4 h y difNa60: 4,7 ± 2,3. El modelo que mejor explica la UF es el que incluye difNa60, MTCcr, edad y tiempo en DP (r = 0,57; p >0,0001). En los pacientes con UF menor de 600 ml (percentil 25) se pierde la correlación entre la UF y el MTCcr, pero se mantiene con difNa60 (r = 0,48). Los 38 pacientes con antecedentes de peritonitis no presentaron diferencias en UF, MTCcr o D/Pcr, pero tienen menor difNa60 (3,7 ± 2,8 frente a 4,9 ± 2,1; p = 0,002) que el resto de pacientes. Conclusiones: La cinética peritoneal realizada con glucosa hipertónica permite no sólo hacer una medida estandarizada de la UF sino también determinar el cribado de sodio, que es el parámetro más sensible para detectar alteraciones del transporte de agua.
INTRODUCTION
The peritoneal equilibrium test (PET), first described by Twardowski et al. in 1987,1 is performed with a four-hour exchange with a 2.27 or 2.5% glucose solution. This test provides good information about the peritoneum’s permeability to small molecules, but does not provide early detection of abnormalities in water transport. Ultrafiltration (UF) failure develops over time in 20% to 30% of all patients on peritoneal dialysis (PD)2 and it is one of the main causes of PD failure.3 It is therefore necessary to find tools allowing us to identify it in early stages and further our knowledge of its causes. The International Society for Peritoneal Dialysis (ISPD), through its Ultrafiltration Committee (UF), recommends performing the peritoneal kinetic study with a hypertonic glucose solution (3.86% or 4.25%) which allows us to measure the peritoneum’s fluid transport capacity under extreme conditions, standardise UF measurements and define ultrafiltration failure (UFF).4 Past preliminary studies of hypertonic glucose kinetics showed results that are similar to those from kinetic studies with 2.27% or 2.5% glucose with respect to small molecule transport (creatinine and urea D/P),5 and have also contributed further information about transcellular water transport through sodium sieving measurements.5-7 During the first hour or two of a hypertonic glucose exchange, we observed a decrease in sodium concentration in the dialysate. This phenomenon, known as sodium sieving, is explained by the passage of free water through transcellular channels that are impermeable to other solutes (aquaporin-1). A decrease in transcellular water transport (TWT) though aquaporins is currently accepted as yet another cause of UF failure,6 which is why the ISPD recommends measuring sodium sieving after 60 minutes or while performing the kinetic studies. On the other hand, we know that in initial PD phases, the correlation between peritoneal permeability and UF is lower than that described for patients who have spent more than a year on PD,8 which indicates that factors other than permeability may lead to UF in early stages. The purpose of this study is to analyse the UF capacity and its relationship with peritoneal permeability and sodium transport in patients treated with PD, using kinetic studies with hypertonic solutions. An additional objective is to confirm that the relationship between UF capacity and peritoneal permeability is different in early stages of PD.
PATIENTS AND METHODS
We performed 184 peritoneal studies in 184 stable patients on PD with a mean age of 50.7 ± 15.9. Of these patients, 75 were treated with continuous ambulatory peritoneal dialysis (CAPD) and 109 with automatic peritoneal dialysis (APD). All of the patients used standard solutions with glucose as the osmotic agent and lactate as a buffer. Mean time on PD was 15.7 ± 22 (1-122 months), 53% of patients were male and 15% were diabetic. Thirty-eight patients had previously experienced an episode of peritonitis. The peritoneal kinetic study was performed while the patient was stable and after resolution of any episodes of peritonitis, haemoperitoneum or an abdominal surgical procedure, where applicable. It was performed according to standard protocol, using a two-litre bag of hypertonic glucose (3.86%/4.25%) with a four-hour dwell. During the peritoneal function study, patients fasted and received no medication except for low doses of insulin subcutaneously where necessary. To measure diffusive function, we collected six peritoneal effluent samples (at minutes 0, 30, 60, 120, 180 and 240) and a baseline blood sample. After making these measurements, we calculated the creatinine dialysate to plasma ratio at 240 minutes (D/P Cr) and the urea and creatinine mass transfer-area coefficients (Urea and creatinine MTACs), according to the previously described mathematical model.2 Standard UF was calculated as the difference between the drained and filled volumes after weighing the bags. Failure (UFF) is considered when UF after a four-hour dwell with a 3.86% glucose exchange is less than 400ml, according to data described by Krediet.9 We measured the percentage of decrease in the sodium concentration against the baseline concentration at 60 minutes (difNa60 min = [baseline dialysate sodium – dialysate sodium level after 60 min) * 100/[baseline dialysate sodium]). Patients were categorised in four groups according to UF quartiles, and each group was subjected to an independent analysis of the correlations between permeability, UF and sodium sieving. Kinetic studies carried out during the first 5 months were also subjected to a later analysis in order to check whether the factors that may lead to UF and their relationships with permeability or water transport are different in early stages. Likewise, we performed a separate analysis of kinetic studies from patients whose history included an episode of peritonitis.
Statistical analysis
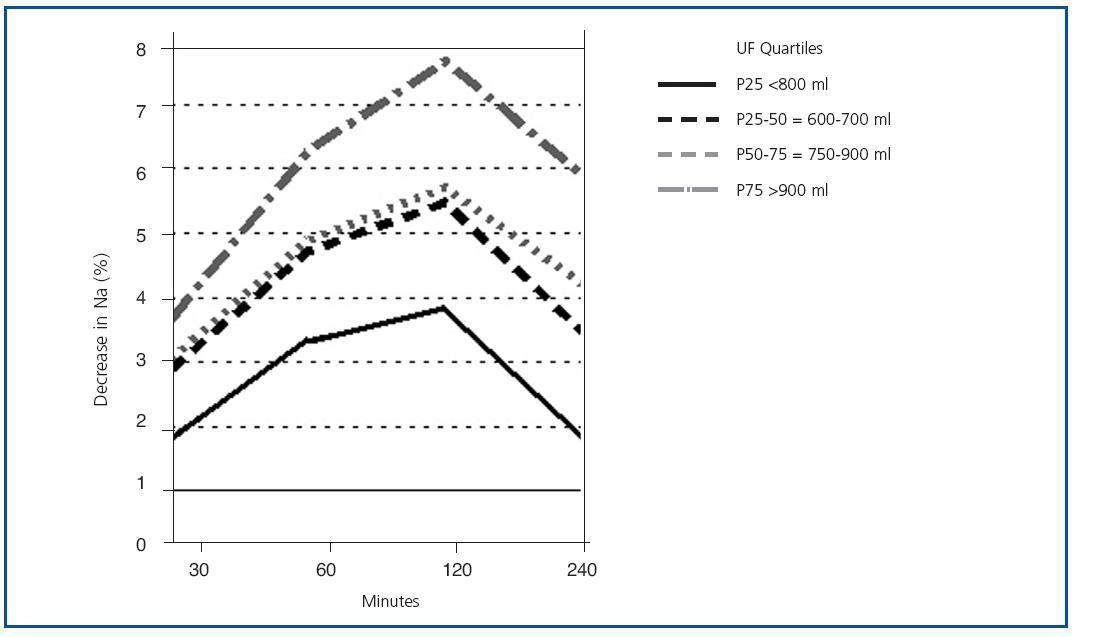
Statistical analysis was carried out using SPSS software version 11.0. Values were expressed as percentages or the mean ± standard deviation (SD). P-values < 0.05 were considered to be statistically significant. Student’s t-test was used to compare means, and the Pearson test was used to establish linear correlation coefficients. Spearman’s test was used for ordinal variables or those without a normal distribution. To establish what variables had an independent association with sodium sieving or UF, we performed a stepwise linear regression analysis, using variables that correlated with these parameters.
RESULTS
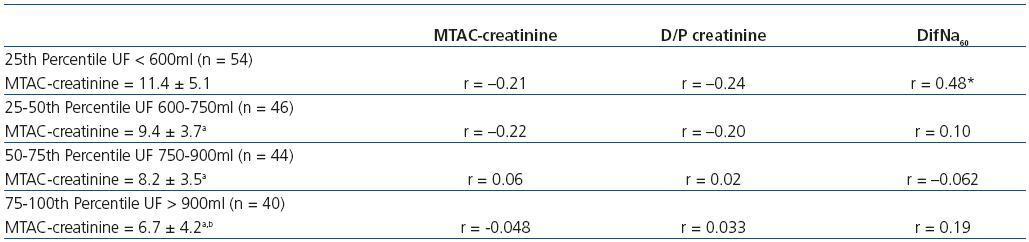
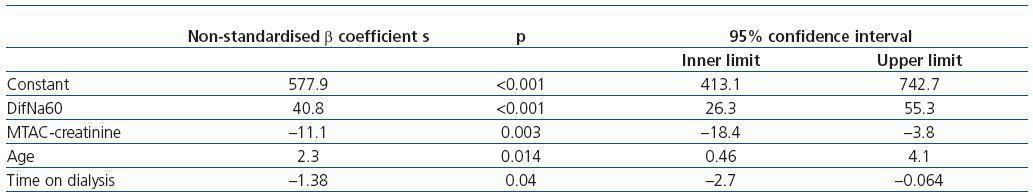
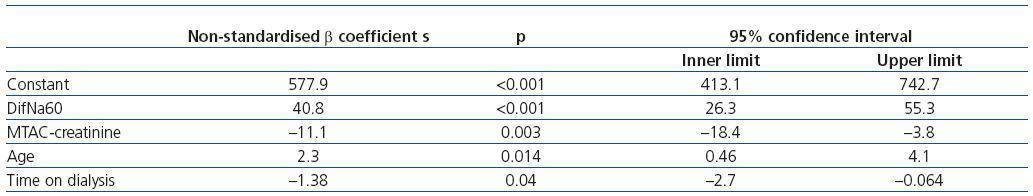
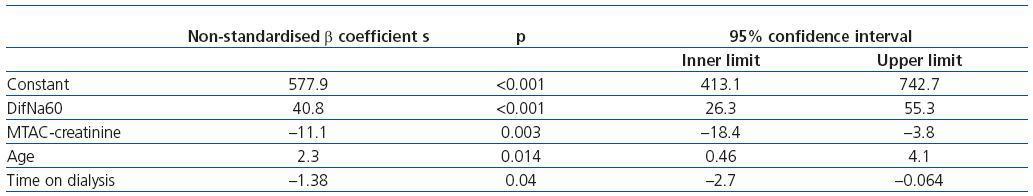
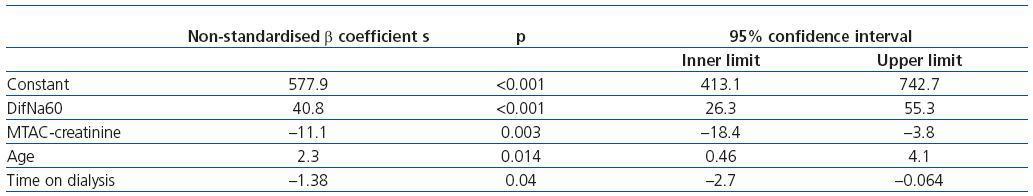
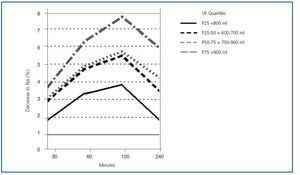
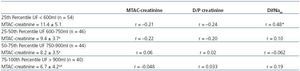
No adverse effects were observed during the test procedure, except for some mild symptoms of volume depletion in patients with residual diuresis and high UF which did not require extraordinary measures to be taken. Table 1 shows the results of the peritoneal kinetic study, expressed as means, range and D/P Cr, MTAC-creatinine, MTAC-urea, UF and percentage of decrease in sodium concentration after 60 minutes (difNa60). We observed a strong correlation between MTAC-creatinine and D/P Cr (r = 0.86; p = 0.000). There were no differences in MTACcreatinine or MTAC-urea, D/P Cr, UF or difNa60 at any time between patients dialysed with CAPD and those on APD. Patients on APD were younger (45 ± 14 vs. 58 ± 14 years) and they had spent more time on PD (12 ± 16 vs. 20 ± 27 months). Thirty-eight patients had presented an episode of peritonitis prior to the kinetic studies (one episode in 17 cases, two in 14 cases, and seven patients had experienced three or more). As shown in Table 2, there were no differences in UF, MTAC-Creatinine or D/P Cr between these patients and the rest. However, patients with a history of peritonitis had a significantly lower difNa60 (3.7 ± 2.8 vs. 4.9 ± 2.1; p = 0.002). In the whole group, difNa60 maintained a very close correlation to UF (r = 0.49) and permeability, measured using both MTAC-Cr (r = –0.45) and by D/P Cr (r = –0.49). It also correlated to a patient’s having had a previous episode of peritonitis (r = –0.22; p = 0.002). The model which best explains sodium sieving (r = 0.61; r2 = 0.38; p < 0.0001) is the model which includes UF, MTAC-creatinine, peritonitis and age, shown in Table 3. Figure 1 shows the evolution of sodium sieving at 30, 60 and 120 minutes, according to the UF quartiles. Patients in the lower percentile for UF (< 600ml/4 h) were clearly differentiated from the rest by the difNa. A difNa greater than or equal to 5% would rule out an UF failure. UF is fundamentally correlated to difNa60 (r = 0.49; p = 0.00), peritoneal permeability of small solutes, measured using either MTAC-creatinine (r = –0.39; p = 0.00) or D/P Cr (r = –0.32; p = 0.00), and time on PD (r = –0.17; p = 0.019). The model which best explains UF (r = 0.57; p < 0.0001) is the one including difNa60,MTAC-creatinine, age and time on PD, shown in Table 4. The peritonitis episodes are not included. When we categorise patients in four groups according to UF quartiles, we observe that although MTAC-creatinine was significantly higher in subgroups with less UF, the correlations between UF and permeability within each of the groups disappear (Table 5). Correlations between UF and difNa60 also disappear in the three groups with the highest UF, but in the patient group with UF < 600ml/4 h (P25), a good correlation between UF and difNa60 remains (r = 0.48; p < 0.001) (Table 5). Lastly, we compared the 72 kinetic studies performed in patients who had been on dialysis during less than six months with the other studies. There were no significant differences for UF (753 ± 232ml/4 h, < 6 months vs. 763 ± 237ml/4 h > 6 months), difNa60 (4.6 ± 2.3 vs. 4.7 ± 2.3), D/P Cr (0.72 ± 0.1 vs. 0.71 ± 0.1) or MTAC-creatinine (9.3 ± 4.5 vs. 8.9 ± 4.5ml/min). The correlation between UF and MTAC-creatinine is less pronounced in kinetic studies performed before six months on dialysis (r = –0.33 vs. r = –0.43; p < 0.05).
DISCUSSION
UF deficit, whether inherent or developing over time on PD, is currently one of the main factors determining patient and technique survival.3 For that reason, it is crucial to measure UF in a standardised way at baseline and on a regular basis afterward to further our knowledge of the causes of UF failure. In our unit, the peritoneal kinetic studies have been performed with 3.86%/4.25% hypertonic glucose since 1999. The first thing we notice in the present study is that the prevalence of UF failure (4.9%, 9/184 patients) is lower than that reported by other authors.7-10 This may be due to the low values for both mean time on dialysis (15.6 months) and the incidence rate of previous peritonitis episodes, both of which are considered to be principal determining factors for UF loss.3 However, the definition of UF failure as UF below 400ml/4 h does not imply that smaller decreases or progressive losses of UF are not pathological. Milla et al.11 studied 95 incident patients on PD with kinetic studies using 3.86% glucose by taking baseline and yearly measurements. They observed that a decrease in UF occurs over time on PD, and this decrease is significant beginning at the threeyear mark. It is only preceded by changes in sodium sieving; the rest of the peritoneal transport parameters (D/P Cr and D/P glucose) remain stable over time. As our group has already stated, peritonitis is one of the main factors determining loss of UF.3,12 According to the present study, difNa60 is very likely to be the earliest parameter to change following peritoneal inflammation in patients with a history of peritonitis. According to our results and those generated by Milla et al., it is recommended to carry out kinetic studies with hypertonic glucose following peritonitis episodes. By doing so, we can predict which patients are at risk of developing UF failure at an early stage, and evaluate the need for therapeutic measures such as peritoneal rest. Carrying out kinetic studies with hypertonic glucose enables us to measure not only diffusive transport (with results showing similar small molecule permeability to those obtained with 2.27% glucose) but also the maximum peritoneal water transport capacity, as well as to analyse the relationship between permeability and UF. The latter is attained in PD thanks to glucose’s osmotic capacity, which disappears rapidly if the peritoneum is very permeable. It is therefore logical that the UF after a four-hour exchange would depend on peritoneal permeability. In our study, we have found a correlation between peritoneal permeability and UF, but it is not as high as that found by other authors.10 Furthermore, as found by other preliminary studies done by our group,8 this correlation is smaller in kinetic studies performed before the first six months, which indicates that factors other than peritoneal permeability determine the UF, especially in initial stages of PD. This lower correlation between permeability and UF can be observed most of all in groups of patients with high transport rates or a low UF.8 An interesting finding from this study is that patients with a UF below 600ml/4 h (P25) lose the correlation between UF and MTAC-creatinine or D/P Cr, but maintain the correlation between UF and difNa60 (r = 0.48; p < 0.001). This is a very important finding, since in these patients, performing the kinetic study with 3.86% glucose enables us to detect and quantify UF failures that the D/P Cr and MTAC-creatinine readings may not identify properly. Therefore, in extreme situations, such as high peritoneal transport rate or UF failure, a kinetic study with 3.86% glucose, standardised UF measurement and sodium sieving becomes a highly useful and more sensitive tool for detecting abnormalities in transcellular water transport. In conclusion, kinetic studies performed with hypertonic glucose are well-tolerated. Furthermore, thanks to standardised UF and sodium sieving measurements, they allow us to detect and offer a better definition of alterations in peritoneal water transport that are not solely caused by an increase in peritoneal permeability, particularly after peritonitis episodes or in patients with a low UF.
Figure 1. DifNa according to ultrafiltration quartiles.
Table 1. Overall results from the five peritoneal kinetic studies
Table 2. Results from the peritoneal kinetic studies in patients with and without a history of peritonitis
Table 3. Multivariate analysis of the factors associated with difNa60 60
Table 4. Multivariate analysis of the factors associated with ultrafiltration
Table 5. Correlations between ultrafiltration and MTAC-creatinine, D/P creatinine and sodium sieving according to ultrafiltration quartiles