Aim: To evaluate the prevalence of cardiovascular disease (CVD) and its association with cardiovascular risk factors, as well as their control in end-stage renal disease (ESRD) patients under maintenance hemodialysis (HD). Patients and methods: A total of 265 patients with ESRD on maintenance HD from a University Hospital and 4 dialysis units were included in this multicenter and cross-sectional study that analyzed the prevalence of CVD and the possible association with classic and new cardiovascular risk factors. Usual biochemical and haemathological parameters were analyzed, as well as plasma levels of homocysteine, troponin-I, BNP, lipoprotein(a), C reactive protein, IL-6, fibrinogen, asymmetrical dimethylarginine (ADMA), advanced oxidation protein products (AOPP), malondialdehyde, adiponectin, osteoprotegerin, and fetuin. In a subset of patients an echocardiography and carotid artery Doppler echography were also performed. Results: The prevalence of CVD was 52.8%. Factors positively associated with prevalent CVD were age, BMI, left ventricular hypertrophy, hypertension, dyslipidemia and diabetes mellitus, dialysis vintage, Charlson´s comorbility index, levels of fibrinogen, osteoprotegerin, BNP and CRP, as well as carotid intima-media thickness, left ventricular mass and pulse pressure. Factors negatively associated with prevalent CVD were: previous renal transplant, ejection fraction or levels of LDL-c and phosphorous. In the multivariate analysis dyslipidemia, left ventricular hypertrophy, age and LDL-c (negatively) were associated with CVD. Conclusions: In HD patients the prevalence of CVD is high and is associated with the presence of cardiovascular risk factors and subclinical CVD.
Objetivo: Evaluar la prevalencia de ECV y su asociación con FRCV clásicos y nuevos, así como el control de los mismos en pacientes con IRCT en programa de HD. Pacientes y métodos: Se incluyeron 265 enfermos prevalentes con IRCT en HD de un hospital universitario y cuatro centros de diálisis. Estudio multicéntrico y transversal que analizó la prevalencia de ECV y su posible asociación con FRCV clásicos y nuevos. Se analizaron parámetros bioquímicos y hematológicos habituales, así como niveles de homocisteína, troponina-I, BNP, Lp(a), PCR, IL-6, fibrinógeno, ADMA, AOPP, malondialdehído, adiponectina, osteoprotegerina y fetuína. En un subgrupo de enfermos también se realizaron ecocardiografía y ecografía Doppler carotídea. Resultados: La prevalencia de ECV fue del 52,8%. Los factores asociados positivamente a ECV prevalente fueron la edad, el índice de masa corporal, los antecedentes de HVI, la HTA, la dislipemia y la diabetes mellitus, el tiempo en diálisis, el índice de comorbilidad de Charlson, los niveles elevados de fibrinógeno, la osteoprotegerina, el BNP y la PCR, así como el grosor del complejo íntima-media carotídeo, la masa ventricular izquierda o la presión de pulso. Se asociaron negativamente: los antecedentes de trasplante previo, la fracción de eyección cardíaca y los niveles de cLDL o fósforo. En el análisis multivariante, los factores asociados con ECV fueron la dislipemia, la presencia de HVI, la edad y los niveles de cLDL (negativamente). Conclusiones: En los pacientes con IRCT en HD, la prevalencia de ECV es elevada y se asocia con la presencia de FRCV clásicos y ECV subclínica.
INTRODUCTION
Cardiovascular (CV) pathology represents the leading cause of death in patients on haemodialysis (HD) (about half of all deaths)1-4 and causes about 30% of hospitalisations.5 The CV mortality rate in these patients is 10 to 20 times higher than the general population.1
The increased prevalence of CV disease (CVD) and of classic (Framingham) cardiovascular risk factors (CVRF) in uraemic patients, as well as of hypertension (HBP), diabetes, tobacco use, hyperlipidaemia, sedentary lifestyle, or left ventricular hypertrophy (LVH), do not fully explain the increased CV mortality in these patients.5,6 In fact, several studies have shown that the Framingham score underestimates CV risk in renal patients.7,8 On the other hand, the use of medications that have been shown to reduce CV risk in the general population, such as statins and reninangiotensin- aldosterone system (RAAS) inhibitors, has not demonstrated efficacy in these patients9,10 and these medications are furthermore underutilised in this population.
It has been postulated that new CVRF or uraemia specific factors may also be involved in the development of accelerated atherosclerosis and arteriosclerosis in these patients.11 Furthermore, the possible role of dialysis12 to increase CV risk in these patients has not been clarified. The prevalence of new or non-traditional CVRF (hyperhomocysteinaemia, lipoprotein [a] (Lp[a]), hyperfibrinogenaemia, inflammation, oxidative stress13,14) is also very high in these patients. Furthermore, the conditions associated with end-stage renal disease (ESRD) (bone-mineral disease, valvular calcification, hypervolaemia, anaemia, malnutrition, etc.) may also contribute to the increased CV morbidity and mortality in these patients.10,15-19
The aim of this study was to study the prevalence of CVD and associated CVRF in a sample of patients with ESRD on renal replacement therapy with HD.
PATIENTS AND METHODS
Design
We conducted a cross-sectional multicentre study, which included 265 adult patients with ESRD on HD for at least 6 months. They were clinically stable, without evidence of clinical heart failure at the time of inclusion (defined as dyspnoea plus two of the following conditions: increased jugular venous pressure, bibasilar rales, pulmonary venous hypertension, interstitial oedema requiring admission, extra ultrafiltration, or an ejection fraction < 35%), of both sexes, aged 18 and over, and agreed to participate in the study. Written informed consent was obtained from all patients and the study was approved by the Ethics Committee of Hospital Clínic.
METHODS
Demographic characteristics were collected (age, sex, time on dialysis) as well as the presence of CVD of cardiac origin, defined by the existence of ischaemic coronary artery disease, vascular disease, history of episodes of heart failure or arrhythmia, the presence of CVD of non-cardiac origin: cerebral (cerebral vascular accident or transient ischaemic attack) or peripheral (peripheral vasculopathy of the lower extremities, amputation due to ischaemia, intestinal ischaemia, etc.), diabetes, history of hypertension, dyslipidaemia, tobacco use, and characteristics of HD (cellulose or synthetic membranes, type of vascular access, dialysis dose).
Blood pressure (BP) measurement was taken before each of the three HD sessions during the evaluation week, all after 10 minutes of rest in a supine decubitus position. Blood draws were taken before the second or third HD session of the week, after 20-30 minutes of rest in a supine decubitus position. Laboratory testing for clinical follow-up was performed for these patients (blood urea nitrogen [BUN], calcium, phosphate, albumin, PTHi, haemoglobin, ferritin, C reactive protein [PCR], Kt/V), and additional special testing included: lipoprotein(a), homocysteine, asymmetric dimethylarginine (ADMA), advanced oxidation protein products (AOPP), malondialdehyde (MDA), troponin-I, brain natriuretic peptide (BNP), osteoprotegerin, fetuin, and adiponectin. A subgroup of 120 unselected patients also underwent an echocardiogram, and 87 underwent a Doppler ultrasound of the supra-aortic trunks.
The echocardiogram measured the telediastolic and telesystolic sizes of the ventricles in order to calculate the ejection fraction and measured wall thickness in order to calculate the left ventricular mass, based on the Penn convention, and it was normalised for body surface area. The Doppler ultrasound of the supra-aortic trunks evaluated the primitive carotid, the carotid bifurcation, and the origin of the internal carotid bilaterally. In addition, the prebifurcation carotid intima-media thickness was measured; four measurements were obtained and the mean was calculated. A normal value of ≤ 0.9mm was used, based on the 2007 Consensus Hypertension Guidelines from the ESH/ESC.20
Homocysteine was determined by immunoassay in an Advia-Centaur autoanalyser (Siemens Spain, Barcelona), using reactants from the manufacturer. CRP was quantified by nephelometry (BNII Siemens Spain, Barcelona), and troponin-I by chemiluminescence immunoassay (TnI Ultra, Siemens Spain, Barcelona) in an Advia-Centaur autoanalyser (Siemens). BNP levels were also determined through chemiluminescence immunoassay (BNP, Siemens Spain, Barcelona) in an Advia-Centaur autoanalyser (Siemens).
Lipoprotein(a) was determined with immunoturbidimetry (Dia-Sorin, Barcelona, Spain), and the levels of ADMA by HPLC. Levels of adiponectin were determined by radioimmunoassay (Linco Research Inc., St. Charles, MO, USA) and levels of AOPP by a colorimetry technique.21 Levels of osteoprotegerin were established through ELISA (Biomedica Medizinprodukte GmbH, Vienna, Austria) and levels of fetuin through an ELISA kit supplied by Epitope Diagnostics (Epitope Diagnostics, San Diego, California, USA).
Statistical analysis
SPSS 15.0 was used for the statistical analysis. The data are expressed as mean ± SD. The comparison between patients with and without CVD was analysed using a Student’s t-test for unpaired data in continuous quantitative variables or the Chi square test for the qualitative variables.
If the quantitative variables did not show a normal distribution, they were analysed using the Mann-Whitney U test. A p-value < 0.05 was considered significant.
RESULTS
In the sample of 265 patients, 68.3% were male, the mean age was 60.7 ± 16.17 years and the mean time on HD was 60.85 ± 72.5 months. The mean of Charlson comorbidity index was 5.67 ± 2.47 points and 25.66% of patients had a history of a previous renal transplant.
The most common etiologies of renal failure were vascular and diabetic, with 17.7% of cases for each one, followed by glomerulonephritis in 17.4%, unknown cause in 16.2%, polycystic kidneys in 12.8%, chronic interstitial nephropathy in 9.4%, and other causes in 8.7% of cases.
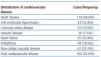
The prevalence of CVD was 52.8%. 44.9% percent of patients had cardiac pathology and 25.3% had non-cardiac vascular disease (cerebrovascular disease or peripheral vasculopathy), as shown in Table 1. On analysis of the presence of classic CVRF, tobacco use (active and exsmokers) was present in 41.5% of cases (16.6 and 24.9%, respectively). 26.8% of patients had a history of diabetes mellitus and 35.8% had a history of dyslipidaemia. The high prevalence of hypertension in 86.8% of subjects is notable. When the average weekly pre-dialysis blood pressure was analysed, 31.4% had a systolic pressure > 140mmHg and 3.8% had a diastolic pressure > 90mmHg. Pulse pressure was > 60mmHg in 42.3% of cases. 19.9% of patients received treatment with angiotensin converting enzyme inhibitors (ACE-I) or with angiotensin II receptor blockers (ARB) and the same percentage received beta-blocker treatment. In the subgroup of patients with coronary disease, 13.7% received ACE-I/ARB treatment while 35.3% received beta-blockers. In the global population, 26.8% received antiplatelet therapy and 6.9% received anticoagulant therapy. Of those patients with coronary disease, 41.4% received antiplatelet therapy and 10% received anticoagulants. Among diabetic patients, 38% received antiplatelet treatment and 7% received anticoagulants.
Among the classic risk factors (table 2), 12.9% had elevated cholesterol levels (> 200mg/dl), 29.5% had cLDL > 100mg/dl, 43.5% had cHDL < 40mg/dl, and 30.5% had TG > 150mg/dl. 24.1% of patients received statin therapy but among those with cLDL > 100mg/dl, only 33.8% received that treatment. Only 38.4% of patients with diabetes mellitus and cLDL > 100mg/dl received statins and 57.69% of those with a history of CVD and cLDL > 100mg/dl received them. The presence of high levels of new CVRF was also common in the patients, as seen in table 2. Markers of inflammation and malnutrition, such as CRP (> 0.8mg/dl), were elevated in 40.7% of patients, IL-6 (> 5pg/ml) in 82.3%, albumin (< 40g/l) in 39.1%, fibrinogen (> 4.5g/l) in 43%, lipoprotein(a) (> 30mg/dl) in 36%, troponin-I (> 0.1ng/ml) in 6.3%, and homocysteine (> 15mmol/l) in 89.4%. 23.2% had haemoglobin levels < 11g/l and 30.9% had a Ca x P product greater than 55mg2/dl2, with calcium and phosphate levels elevated at 34.6 and 65.6%, respectively, based on criteria from the KDOQI guidelines.
In assessing the prevalence of subclinical CVD, we observed that 74% of the patients with an echocardiogram had LVH and that 7.6% had an ejection fraction of < 40%. Of the patients with carotid Doppler ultrasounds, 25.3% had increased carotid intima-media thickness (> 0.9mm). In the univariate analysis, the factors associated with CVD, as seen in tables 3 and 4, were age, body mass index, history of hypertension, dyslipidaemia, and diabetes mellitus, previous time on HD, Charlson’s comorbidity index, elevated levels of fibrinogen and BNP, carotid intima-media thickness, left ventricular mass, and pulse pressure. The following factors were negatively associated with the presence of CVD: history of previous renal transplant, cardiac ejection fraction, and low levels of cLDL and phosphate.
In the multivariate analysis, the factors associated with CVD were age, dyslipidaemia, LVH, and negatively the level of cLDL, as shown in Table 5. By ROC analysis, these factors predicted CVD prevalence with a value of 0.736 (95% CI: 0.675-0.797). (Figure 1).
DISCUSSION
The results of this study, carried out in a population of patients with CKD on HD, emphasize the high prevalence of CVD, which is consistent with results from other similar series. This would explain, in part, the high incidence of fatal and non-fatal cardiovascular pathology in these patients. Furthermore, the prevalence of subclinical CVD (LVH or increased carotid intima-media thickness), as well as of classic and new CVRF is high in this unselected population of patients on HD.
The elevated cardiovascular risk in patients on HD is much higher to that of the general population, and even to other groups of patients recognised to have high cardiovascular risk (e.g., diabetics or hypertensives). This is in part explained by the high prevalence of CVD, both clinical and subclinical. In the univariate analysis, the factors associated with the presence of CVD were age, the presence of subclinical CVD or classic CVRF, markers of inflammationmalnutrition, or markers of cardiac disease, such as BNP. In the multivariate analysis, only some classic CVRF and LVH maintained their predictive value.
The apparent discrepancy between the predictive value of dyslipidaemia and the lowest levels of cLDL may be explained in several ways. The clinical history of dyslipidaemia included hypercholesterolaemia, but also low levels of cLDL or hypertriglyceridaemia (the latter two being more common in kidney patients); on the other hand, patients with CVD were more often given statins and, lastly, low levels of cLDL may be associated with inflammation-malnutrition (another recognised CVRF in this population).
These data reinforce the predictive role of classic CVRF for the prediction of CVD in patients on HD. An interesting finding in the univariate analysis was that patients with CVD had significantly higher levels of osteoprotegerin. In recent years there has been a growing interest in the possible role of abnormalities in mineral metabolism, in its markers (e.g., osteoprotegerin, fetuin, or FGF-23), or in the vascular calcifications on cardiovascular morbidity and mortality in patients on HD. Therefore, a relationship between elevated levels of osteoprotegerin and vascular calcification and mortality has been described in these patients.22 Although the predictive role of OPG was lost in the multivariate analysis, our results add to the association between this marker and CVD in these patients.
Another aspect of our study that is important to draw attention is the poor CVRF control and scarce use of treatments with demonstrated CV protective effects in the non-uraemic population (RAAS inhibitors, statins, antiplatelet agents) in our population even among patients with diabetes or CVD, similar to what has been described in the literature.23 This low CVRF control and a certain “therapeutic nihilism” that is detected in our study may contribute to elevated morbidity and mortality in patients on HD. This may be due, in part, to polypharmacy, which hinders therapeutic compliance and facilitates therapeutic inertia, in addition to the scant evidence of the beneficial effects of the aforementioned treatments in reducing the risk of events in patients on HD.9,10,24
To conclude, the prevalence of clinical and subclinical CVD is very high in our population of patients on HD. Furthermore, the prevalence of classic and new CVRF is also high. The factors predictive of clinical CVD in our population were age and the presence of subclinical CVD (LVH) and classic CVRF. Furthermore, controlling CVRF and using cardioprotective medications in this general population is not sufficient, according to recommendations from the various clinical practice guidelines for these patients. Efforts must be made for early and aggressive treatment (in the pre-dialysis stage) of the CVRF in these patients in order to try to reduce their high CV morbidity and mortality.
Table 1. Distribution of cardiovascular pathology in the population
Table 2. Classic and non-traditional cardiovascular risk factors in the study population
Table 3. Comparison of patients with and without cardiovascular disease
Table 4. Comparison of analytic parameters between patients with and without cardiovascular disease
Table 5. Associated factors in the multivariate analysis
Figure 1. Analysis of ROC curves.