Los hospitales de día son una alternativa en la atención hospitalaria que mejora la eficiencia de la asistencia sanitaria. La nefrología es una especialidad que, por sus características técnicas, se beneficiaría ampliamente de un mayor desarrollo de esta modalidad de atención. Los objetivos del presente trabajo son presentar el proceso de desarrollo del Hospital de Día Médico de Nefrología en el Hospital Universitario Puerto Real (Cádiz). Para este proyecto hemos seguido la metodología del ciclo continua de mejora de la calidad, seleccionando las oportunidades de mejora, analizar las causas, escoger las intervenciones, implantarlas y monitorizar resultados. El plan de intervención consta de los siguientes puntos básicos: 1) definir la disposición física y organizativa de nuestra unidad de gestión clínica y el lugar que ocupa el hospital de día dentro de la misma; 2) definir su manual de organización y funcionamiento; 3) definir los recursos estructurales y de equipamiento; 4) definir la cartera de servicios; 5) normas de los procesos asistenciales, protocolos y vías clínicas, y 6) sistema de información, registro y evaluación. En los primeros ocho meses de funcionamiento se han realizado casi 2.000 procedimientos, lo que corresponde a una media de unos 10 procedimientos/día, creciendo éstos conforme la implantación es mayor, y destacando aquellos relacionados con hemodiálisis en pacientes inestables, críticos o agudos, los procedimientos de nefrología intervencionista, nefrología clínica y los relacionados con la diálisis peritoneal. El desarrollo del hospital de día en la nefrología puede contribuir a potenciar su autonomía, su presencia en los centros, recuperar actividad asistencial y paliar así la pérdida progresiva de competencias diagnósticas y terapéuticas que se han podido producir en beneficio de otras especialidades. También contribuye a incentivar y desarrollar la nefrología diagnóstica e intervencionista, potenciar la gestión por procesos y la continuidad de la asistencia interniveles; impulsar la docencia e investigación; colaborar en la sostenibilidad del sistema, y por último, para hacer más atractiva e ilusionante la especialidad, tanto para los nefrólogos como para los especialistas en formación.
Day Care Units are an alternative to hospital care that improves more efficiency. The Nephrology, by its technical characteristics, would be benefit greatly from further development of this care modality. The objectives of this study are to present the process we have developed the Nephrology Day Care Unit in the Puerto Real University Hospital (Cádiz, Spain). For this project we followed the Deming Management Method of Quality improvement, selecting opportunities, analyzing causes, select interventions, implement and monitor results. The intervention plan includes the following points: 1) Define the place of the Day Care Unit in the organization of our Clinical Department of Nephrology, 2) Define the Manual of organization, 3) Define the structural and equipment resources, 4) Define the Catalogue of services and procedures, 5) Standards of Care Processes. Protocols and Clinical Pathways; and 6) Information and Registration System. In the first 8 months we have been performed nearly 2000 procedures, which corresponds to an average of about 10 procedures per day, and essentially related to Hemodialysis in critical or acute patients, the Interventional Nephrology, the Clinical Nephrology and Peritoneal Dialysis. The development of the Nephrology Day Care Units can help to increase our autonomy, our presence in Hospitals, recover the progressive loss of clinical activity (diagnostic and therapeutic skills) in the past to the benefit of other Specialties. It also contributes to: Promote and develop the Diagnostic and Interventional Nephrology; improve the clinical management of patients with Primary Health Level, promote the Health Education and Investigation, collaborate in the Resources Management, and finally, to make more attractive and exciting our Specialty, both for nephrologists to training specialists.
INTRODUCTION AND OBJECTIVES. FOCUSING ON THE CURRENT SITUATION
“Day hospital” (DH) care is the one is provided for a few hours, including diagnosis, clinical tests, and/or multiple examinations, as well as treatments that cannot be provided in the outpatient setting, but done in situations that do not require complete hospitalisation.1
The dissemination and consolidation of DH, the diversity of organisational, structural, and functional configurations that this health care mode can adopt, and its repercussions in terms of quality of care and patient safety all prioritise its inclusion in the fields covered by the Quality Plan for the Spanish National Health System,2 along with the elaboration of quality and safety criteria and the promotion of its evaluation as a support to clinical management and decision-making, since it has been clearly shown that DH are an alternative to hospitalisation that improve the efficiency of health care.3
Although this mode of health care is widely used in surgical specialties (outpatient surgery), it is increasingly being incorporated into more medical specialties.4,5
Few medical specialties boast as many special techniques and procedures as nephrology, making it possible and probably recommendable or even necessary to develop DH and day care hospitals (DCH) in our specialty. This should have a direct impact on cultural changes occurring in our hospitals,6,7 where organisation and rationalisation should be a priority, within the framework of better evidence and clinical management units (CMU), and not within a conventional rigid hospital structure.8,9
Additionally, nephrology DCH would aid in improving some issues that have been highly debated by the Spanish Society of Nephrology (SEN),10 such as professional incentives, or returning to certain abandoned topics (acute renal failure, renal biopsy, etc.) that have in many cases been taken up by other medical specialties; designing a platform for the implementation and development of interventional nephrology11; establishing greater clinical independence, primarily in the processes related to vascular and peritoneal access and ultrasound and diagnosis techniques; developing clinical management; prioritise outpatient or minimal hospitalisation techniques, condition-specific patient management, and cooperation with system sustainability.12 Furthermore, this could primarily make our specialty more attractive, both for current nephrologists and those in training to become specialists.13,14
The objectives of our study were to present the process that we have developed in the nephrology DCH at the Puerto Real University Hospital (Cadiz) as a continuous improvement project, presenting our strategic lines, the resources and structure we have designed, the services provided, rules for functioning, the registry and information storage system, etc., as well as to present our results from the first 8 months of functioning.
IMPROVEMENT PROJECT FOR THE NEPHROLOGY DAY CARE HOSPITAL. THE CYCLE OF CONTINUOUS QUALITY IMPROVEMENT
One of the principles of excellence in health care is the continuous improvement of quality.15,16 One of the key concepts to continuous quality improvement is that health care quality can always be improved.17
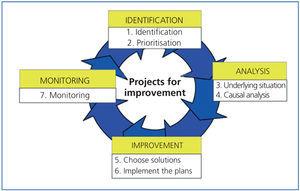
The Deming method of quality improvement is the methodological tool that provides the opportunity to increase the quality of these processes.18,19 The following phases make up the system which was used in our nephrology DCH project (Figure 1):
1. Selection of opportunities for improvement (problem identification)
a) Choose a group for improvement
b) Focus the process
c) Analyse the causes
d) Choose the actions that can be improved (interventions)
e) Monitor (evaluate the intervention)
First phase. Identification of opportunities for improvement
In order to improve, one must identify the situations that can in fact be improved. That is to say, identify errors, which leads to understanding and consequent improvement.
Our institution included an acute nephrology unit, which later became the current nephrology DCH. It had a series of problems which were identified using an analysis of communications and suggestions from the health care professionals that made up the unit, as well as through direct observation of the daily difficulties that arose. After ordering these problems in matrices, they were prioritised in the manner illustrated in Table 1, and which we will summarise later. These results are surely applicable to the majority of acute nephrology units in Spain, and we can use them to define the fundamental steps for identifying the need for a nephrology DCH after establishing our department as a clinical management unit (CMU):
Lack of independence from units such as emergency departments and hospitalisation for patient stabilisation; lack of self-sufficiency in specialty interventional procedures, such as kidney biopsy, insertion of tunnelled vascular catheters or peritoneal catheters, excessive dedication of the acute nephrology unit to problems associated with the chronic haemodialysis (HD) programme, inexistence of a digital registry of health activities, and others.
Second phase. Cause analysis
The majority of opportunities for improvement require a more in depth analysis.
Once they have been identified and selected, the problems pass on to the second phase, which corresponds to analysis. This phase could be further subdivided into two sub-phases: the selection of the improvement team and an analysis of the causes of the problem.
The improvement of health care processes relies crucially on the involvement of the health professionals that are most familiar with the issues. This group of professionals is referred to as the improvement team, which must be multi-disciplinary and all its members should have the necessary attitude and aptitude. The improvement team, following these conditions, was made up of nephrologists, including the CMU director and a university expert nephrologist representing health care institutions, as well as nursing staff from the CMU, and advice and support from the hospital management (especially from the general department assistant director), and by the department of clinical information and documentation.
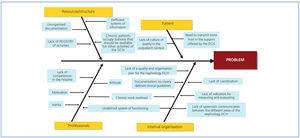
Different tools can be used to search for the causes of deficient functioning, as demonstrated using the Ishikawa (fishbone) cause and effect diagram for our particular case (Figure 2). The following questions must be answered: what is failing? where?, and how do we know? Following this methodology, we could distinguish different issues:
Staff-dependent causes. These can be due to two different deficits: attitude, and competence (lack of knowledge or skills).
Organisation-dependent causes. Internal strategies, established procedures and protocols, distribution of functions and responsibilities, organisational pathways, schedules and adaptation of the available services to the needs of the population.
Lack of structure and resources. These are causes due to deficient structure, material resources, etc. Sometimes, supposedly structural deficits are, in fact, due to an inefficient use of existing resources that is caused by organisational problems, inadequacy, or poor quality of the resources.
Patient-dependent causes. Failure to adapt to the outpatient system, lack of trust in the resolution of a condition without hospitalisation in a day hospital, etc.
Third and fourth phases. Choose the actions that can be improved (interventions) and monitored (evaluate the intervention)
Once the causes have been identified, a course of action must be chosen to neutralise or resolve the issue. For this purpose, all different solutions and alternatives must be considered, implemented, and tested, preventing breakdowns, and evaluating the support of and resistance to change.
In order to implement these actions, all of the health care personnel implicated in the transition must be involved in the process, whether or not they make up part of the improvement team, the necessary amount of time must be dedicated to the process, concentration must be maintained throughout, and those involved must work in close contact with the team director(s).
It is also important that the changes incurred by the teams generate stable processes that reduce variability and produce improved results.
We will develop these last phases in the following section, where we will describe the planning and implementation of the nephrology DCH at our CMU.
INTERVENTION PLAN FOR THE IMPLEMENTATION, ORGANISATION, AND MANAGEMENT OF THE NEPHROLOGY DAY CARE HOSPITAL
Physical and organisational layout of the nephrology day care hospital within our clinical management unit. The role of the coordinating doctor and nursing staff
The Puerto Real University Hospital in Cadiz provides specialised health care to an assigned population of 330 000 inhabitants (according to data from the National Institute of Statistics [INE] from 2008), a value that is tripled during the high tourism season, in a territory of 2100km2 and approximately 100km at its greatest radius. This is a general specialty university hospital, classified as a group II hospital by the Andalusian health department, with 9 basic health areas, 13 health centres, and 10 clinics. The hospital boasts approximately 450 beds in five different areas: medical, surgical, maternal/neonatal, intensive care and emergency, and diagnostic support departments. The hospital discharged 15 629 patients in 2009.
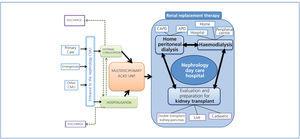
The nephrology CMU of the hospital is organised around the strategic processes that are essential to our specialty, and in accordance with the catalogue of services we provide. Its structure and complexity are detailed here, and also graphically represented in Figure 3:
1. Entrance to the nephrology CMU: primary care, emergency care, and inter-consultations from other CMU.
2. Outpatient care: general outpatient clinic nephrology and a specific unit for glomerular diseases.
3. Hospitalisations: clinical nephrology in the context of hospitalisation.
4. Multi-disciplinary unit for advanced chronic kidney disease (ACKD): Integrated health care process for chronic kidney disease, dialysis, and kidney transplant (ICP CKDDT).
5. HD unit: ICP CKDDT.
6. Home peritoneal dialysis (PD) unit: ICP CKDDT
7. Evaluation and preparation for kidney transplant: cadaveric, live, and double transplant techniques. Our hospital is not a transplant centre, and so the transplant competencies within our CMU are limited to those described.
8. Continuous 24h treatment.
The nephrology DCH is composed of a central and a transverse unit within the CMU, which offers health care and organisational support to other units, such as outpatient care, hospitalisation, and the ACKD unit, as well as the HD and PD units, and the 24h shift in the specialty. The DCH is coordinated and managed by a nephrologist who is also responsible for the PD programme, and by a nurse from the CMU. These people are not exclusively dedicated to this area, as they have other responsibilities in the CMU. They coordinate and help all other health care professionals in the unit that, together with them, perform the different procedures of the DCH, each one within their own area of responsibility.
Manual for organisation and functioning
The DCH has its own organisational and functioning manual in which the following points are made (which we will expand in the following sections):
1. The composition and physical organisation of the unit (previously described and illustrated in Figure 3).
2. The structural resources and equipment available.
3. Catalogue of services.
4. Organisation and regulations for the health care process. Clinical pathways and protocols.
5. Information, registry, and evaluation systems.
The general requisites for organising the CMU described here will be respected in the manual. It must be open and easily updated, according to the modifications produced in the list of services or when structural or functional changes to the unit require it.
Structural resources and equipment
In addition to the normal waiting rooms, reception, toilets, access for beds and carts, storage, etc., here we will focus primarily on the health care zone of the DCH, which consists of the physical spaces in which direct patient care takes place. This is an area of internal circulation, reserved exclusively for patients and health care staff. Its flexible design allows the admission of a wide range of cases, treatment facilities, and even unscheduled patients, and, in consequence, is adapted to the multiple structural and functional requirements that they imply. This area is made up of consultation rooms, an interventional nephrology room, and multipurpose rooms with chairs and beds:
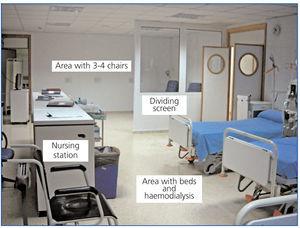
Multipurpose room with beds and chairs (Figure 4 and Figure 5)
The treatment stations can take on many forms, but generally use treatment chairs or beds as the primary support, according to the characteristics of each treatment. Given the wide range of techniques available, the design should, as in previous cases, allow for flexible structures that can be easily adapted to changing patient needs.
Taking into account this premise of flexibility, the initial layout of a multipurpose room involves four beds and three or four chairs. All are equipped with oxygen and suction equipment. The four beds have outlets for treated water and outputs for HD machines to facilitate their use, as well as for administering treatment or stabilising patients, and to offer HD to acute or chronic unstable patients (previously known as acute nephrology). Each station, bed or chair has all electrical connections needed for illumination and the use of electrical medical equipment needed for treatment.
The area of chairs and beds is separated by a fixed screen with transparent glass that allows the nursing staff to observe at all times the patients in each station. This glass can be covered with blinds as needed for privacy.
The room also has a cardiopulmonary resuscitation (CPR) cart, vital signs monitors, television, medicine cabinets, etc.
The DCH multipurpose room is configured such that health care personnel can access the patients in the simplest manner possible from a nursing control point that looks over both areas, located in a central zone of the unit with easy access to all stations, beds and chairs, open on all sides to minimise distances and facilitate observation of patients during treatment and recuperation, with support elements for the administration of each treatment and type of patient recovery. This site also serves for the planning of patient care and administrative tasks for the nursing staff, as well as a clinical station for digital access to patient management applications.
Consultation rooms
In the DCH, patient care prior to treatment often requires examination, diagnosis, patient selection following a clinical evaluation, and indications for treatment regimens. The patient must also be provided with necessary information and consent must be obtained, which takes place in a multipurpose room that can also be used for examining patients after being discharged from a hospital or the DCH, nursing consultations, etc.
Advanced chronic kidney disease unit
Multidisciplinary care of ACKD is an essential component of our CMU and has also been integrated into the nephrology DCH, since it facilitates better training for patients and family members regarding techniques used, singular treatment actions such as the administration of intravenous iron, care given to vascular and peritoneal access points, and the stabilisation of decompensated patients.
Peritoneal dialysis unit
The structure of the DCH has also maintained this unit for the administration of intravenous drugs, the stabilisation of decompensated patients, treatment of complications and peritoneal infections, and patient training. The close proximity to the ACKD unit allows for close relations between these two departments, which facilitate training ACKD patients regarding these techniques and mutual support (between patients). The PD unit has, within the DCH, an examination room with places for a doctor and a nurse, a home teaching unit for CAPD and APD, and a room for treating complications and peritonitis (Figure 6).
Interventional nephrology unit (Figure 7)
Finally, the DCH includes the interventional nephrology unit, where renal biopsies, ultrasound procedures, vascular accesses (temporary and tunnelled), and peritoneal catheters are implemented and monitored, along with other techniques (as we will see in the catalogue of services). Its placement within the structure of the DCH permits patients to recover in the multipurpose room.
The available equipment includes a hydraulic stretcher, surgical sink, monitors, tensiometers, ultrasound scanners, etc.
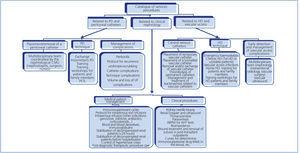
Catalogue of services (Figure 8)
The selection of procedures and treatments to be included in the DCH defines its catalogue of services (Figure 8), which has been arranged according to the fundamental areas supported:
Procedures related to peritoneal dialysis and catheters
Dialysis exchange, dealing with complications of the technique or catheter, percutaneous placement and removal of the peritoneal catheter, managing peritoneal infections, and intermittent peritoneal dialysis with a cycler, etc.
Procedures related to haemodialysis and vascular accesses
Haemodialysis sessions in acute patients and unstable chronic patients. First sessions before inclusion in chronic programmes (at peripheral centres or hospitals), early detection of complications with the vascular access point (Doppler ultrasound), insertion and removal of temporary and permanent tunnelled vascular catheters, managing infections related to vascular accesses, etc.
Procedures related to clinical nephrology
Administration of intravenous drugs: iron, immunosuppressive drugs, corticosteroids, etc. Blood and haemoderivatives. Immunoglobulins. Stabilisation without hospitalisation of decompensated patients that seek treatment in our consultation or the emergency room (hypertensive crises), and stabilisation prior to hospitalisation (if hospital stay exceeds 24 hours). Procedures such as kidney biopsy, bioelectrical impedance tests, ambulatory blood pressure monitoring (ABPM), thoracocentesis or paracentesis, renal Doppler ultrasound, etc.
At our centre we do not perform kidney transplants, but we do indicate in the catalogue of services some procedures that could be carried out at a nephrology DCH in transplant centres such as wound treatment and suture removal in post-kidney transplant outpatients, double J catheter removal, determining curves for immunosuppressive drug levels in the blood, administering ganciclovir or cidofovir, antibiotics, etc., and all activities considered in involved services.
Organisation and regulations in the development of the health care process. Protocols and clinical guidelines
In addition to the basic regulations for administrative management (clinical histories and documentation, data protection, etc.), the DCH is governed by regulations that are adjusted to the organisational requirements of the health care provided, which sequentially describe the actions to be taken in health situations, the necessary protocols, and the responsibilities of each health care professional for all activities. They include the following actions:
Patient reception and general preparation
1. Confirmation of the appointment, identity of the patient, and process.
2. Confirmation of compliance with previous instructions, as well as confirmation of the information received and informed consent.
3. Assignment of the resources to be used in caring for the patient.
4. Preparation of the procedure (confirmation).
Development of the procedure according to clinical guidelines and/or protocols.
By monitoring health care plans that are multi-disciplinary (nephrologists, nurses, nursing assistants) and structured (ordered description of the sequence of actions to be taken), detailing the essential steps and key points for patient care in each specific procedure or problem.
In a similar manner, these plans define the sequence, duration, and optimal responsibility of the different health care professionals for a particular procedure or diagnosis, minimising delays, improving the use of resources and health care quality.20-23
Clinical pathways have been developed as an instrument for each procedure, and are composed of24:
1. A temporal matrix detailing the activities of all health care professionals involved in each step of the process, specifying other important aspects such as complementary tests, diet, and medication.
2. Deviations sheet. Any deviation from the pathway or action taken and their justification are recorded here.
3. Information sheet for the patient and family members. This includes a series of illustrations that inform the patient as to the most common progression of the process and the steps to be taken before and after the procedure.
Recovery, discharge process, and continuity of health care
1. Pre-discharge safety protocol;
2. Decision for discharge or hospitalisation;
3. Evaluation by the attending doctor;
4. Criteria for discharge;
5. Discharge report;
6. Post-discharge instructions;
7. Definition of the post-discharge follow-up plan and continuity of health care (follow-up appointment or appointment for a second session of treatment, submission of documents and referral notes for laboratory tests, or recommendations for the attending doctor and nursing staff at the institution if there will be a joint follow-up or discharge to primary health care provider).
Information, registration, and evaluation system
In addition to the clinical stations at each of the units of the nephrology DCH that store the electronic copy of the patient’s clinical history and departmental information (laboratory results, imaging diagnostics, etc.), there must be a system for registering information that will be integrated into the general hospital system and connected to the department of documentation and health information. The goal is to have all activities carried out registered and communicated to the department of hospital information, such as DH activity for annual reports, compliance with objectives, lists of responsibilities, etc.
In contrast to conventional hospitalisation and protocols for major outpatient surgery, there is no universal coding system established within the national health system for the processes attended to at DH units.1 For this reason, at our centre, the department of clinical documentation and information, along with our own CMU, has designed a database stored on the hospital server, with direct access to each nephrology DCH station in order to register all activity.
This is a simple application designed in Access (Figure 9), made up of the following components:
1. Personal information. Patient first and last name, social security (SS) number, regional digital clinical history number, date of birth, and sex.
2. Primary and secondary diagnosis, using drop-down menus classified according to the International Classification of Diseases ninth revision (ICD-9).
3. Procedures performed, also using drop-down menus coded using the ICD-9.
4. The data collection table is structured for exporting the minimum basic data set (MBDS) defined by the support services of the Andalusian Health Care Service.
In a similar manner, the database will be communicated to the department of health information and documentation that will allow for periodical evaluations of activity, quality, and performance indicators. Currently, we are designing the most appropriate indicators for measuring each of these areas, since no specific quality indicators exist for these units overall.
According to the manual developed by the Ministry of Health in 2008 for DH units1 and other publications on health care quality, at least three different indicator areas should be configured for DH, in addition to the specific indicators for each process or procedure of the specialty (e.g., the Andalusian health department quality regulations for the integrated health process of treating chronic kidney disease, dialysis, and transplant25):
1. Scientific and technical quality and efficiency of the DH unit, such as:
a) Indicator for cancelling sessions,
b) Indicators for adverse events.
2. Efficiency of the system, such as an index of transfer to outpatient care (percentage of sessions in DH/hospitalisations in a conventional institution).
3. Perceived quality by patients in the DCH26: indices of satisfaction obtained through a satisfaction survey.
RESULTS FROM 8 MONTHS OF FUNCTIONING OF THE NEPHROLOGY DAY CARE HOSPITAL AT THE PUERTO REAL UNIVERSITY HOSPITAL
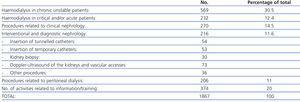
Table 2 shows the distribution of procedures performed during the first 8 months of the functioning of the DCH.
We would like to highlight that 1867 procedures were performed in this time period, an average of 10 procedures/day. Logically, the use of the DCH continues to grow as its implementation has come into effect, such that the mean daily number of procedures performed in the last three months of the trial period was practically double the initial rate.
The HD sessions of critical and/or acute patients and those performed with unstable patients also stand out. It is also important to note the number of interventional nephrology (catheter insertion, biopsy, etc.), clinical nephrology, and PD-related procedures. We also will point out that the DCH is an ideal space for education and training for patients and families.
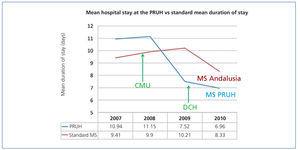
Other results showing the impact of the implementation of the nephrology DCH are the good mid-term evolution of the mean duration of hospital stay (Figure 10), which were better than the standard in the same hospital group (6.96 vs 8.37, respectively) since our constitution as a CMU, or the index of hospital use (true rate of hospital stays compared with expected rates based on patient conditions, with desirable values between 0 and 1), which is below the group mean (0.78 vs 0.94, respectively). This has all been achieved while maintaining complexity superior to the group mean.27 The DCH is not excessively used to the detriment of more simple forms of outpatient care.
DISCUSSION
HD is a treatment alternative to classic hospitalisation units, which is the consequence of a health care need. This provides an intensive, integrated, and very specific treatment approach in our specialty. This therapeutic specificity is determined by the existence of a concrete protocol directed towards these pathologies, from a heterogeneous model integrating spaces within a framework of special, emergency, and minimal stay techniques in nephrology. As such, DCH is an efficient health care alternative to conventional hospitalisation, since it favours accessibility and continuity of health care. It also promotes coordinated, agile, and outpatient health care without the downsides of hospitalisation or the prolongation of hospital stay, thus rationing health care resources.
The nephrology CMU project at the Puerto Real University Hospital (Cadiz), included the design and development of a DCH for the our specialty, with the goal of responding to specific needs with a specific range of services, with defined structure, resources, and organisation, with a system of information and registry and a methodology of periodical evaluation.
What can nephrology day care hospitals add to our specialty in Spain?
Recover the health care activity, presence, and development of nephrology
The past several years have witnessed a serious problem in our specialty, which has even been discussed in the “Libro Blanco de la Nefrología” (White Book of Nephrology),28 the progressive loss of both diagnostic and therapeutic competences, in benefit of other specialties.
Since its inception, nephrology has increasingly focused on chronic kidney failure, with very specific diagnostic and therapeutic programmes. However, this has led us to abandon our role in the treatment of other pathologies originating or associated with renal diseases that require our intervention. The reasons for this trend are varied, such as hospital work overload as a primary cause, but also the loss of certain techniques due to a level of disenchantment and apathy in the fight for developing the realm of nephrology or due to the interest by other specialties to continue to develop their competencies and spheres of activity.
The development of specific areas of nephrology, such as DCH, could favour the recovery of these lost techniques, since we are capable of offering day treatments and high-resolution procedures for these entities that fall within competencies shared with other specialties, such as immunosuppressive drugs in primary or secondary autoimmune pathologies (such as lupus nephritis), arterial hypertension, diabetic nephropathy, urinary infections, metabolic studies in renal lithiasis, acute renal failure, kidney biopsy (as we will see in the section on interventional nephrology), etc.
The consequences of the recovery of this activity by nephrology are clear: an increase in the perspectives regarding presence, identity, and future development of the specialty within the hospital environment, by “redefining” its own competencies, and in the extra-hospital environment, i.e., the relationships with primary health care providers, as we will see farther ahead, and placing value on those things that, due to their routine nature, do not receive their due importance, as well as redefining available spaces in order to increase internal functioning and organisation efficiency.
Promote and develop diagnostic and interventional nephrology
As described by Rivera and Quereda,11 as the dialysis treatment process was generalised, nephrologists abandoned the practice of interventional treatment of their patients to the benefit of other specialties (mainly surgeons and radiologists), which we consider to be a strategic error by our specialty.
We are currently working to correct this tendency, although in Europe there is still greater interest in the diagnostic realm than in the interventional one. Furthermore, Spain is producing interventional nephrologists, although as the mentioned authors have pointed out, only a few have published articles on their experiences.29-31
The implementation of an DCH in nephrology units, with access to a room for ultrasound diagnostics and interventional nephrology, could facilitate the development of this area of knowledge and competence32 for nephrology, with a nephrologist in charge of the DCH that can coordinate ultrasound and interventional techniques performed by the rest of the nephrologists on staff, regardless of whether they are also responsible for the interventional area of nephrology (peritoneal and vascular catheters, clinical nephrology, etc.), with specific clinical pathways and protocols for avoiding variability and increasing safety.
In this manner, the inclusion in our units of ultrasound techniques, kidney biopsies, the insertion of peritoneal or permanent vascular catheters, among others, can allow us to offer integrated and rapid treatment for patients with renal problems. Moreover, it is an opportunity for specialists to recover those diagnostic and treatment techniques that we may have lost, along with increased control of the programmed start of dialysis treatment, as we could place tunnelled catheters for HD, peritoneal catheters for PD,11 and evaluating vascular risk in patients with chronic kidney disease.33,34
We would also pursue self-sufficiency in the stabilisation of decompensated patients with no need for hospitalisation or aid from emergency services, as well as the evaluation of patients upon discharge and before their follow-up in regular visits or primary care.
The DCH multipurpose room has beds available that, as well as offering HD for acute and unstable patients, can be used to stabilise patients that do not need hospitalisation, whether in ACKD, PD, or general nephrology patients, etc., in the form of a specific nephrological observation unit, where nursing staff can provide the necessary treatment or health care during a maximum time span of 24 hours, and under the supervision of a nephrologist. After 24h, the patient will be discharged and health care continuity will start at the corresponding unit.
At times, this multipurpose room can also be used for stabilising patients before hospitalisation if they need closer monitoring or initial care.
In a similar manner, the nephrologist responsible for hospitalisations at our CMU attempts to favour early discharge and adequate indices of hospital use and mean duration of stay, and avoid rehospitalisation by programming one or two short evaluations (within one week) before the patient is referred to nephrological consultations or primary care, in order to verify the level of recovery and prevent early complications. These short evaluations are performed in the consultation rooms of the DCH.
Respond to the emergencies derived from renal replacement therapy programmes (dialysis and transplant)
The nephrology DCH does not lose the functions of the old acute nephrology unit, but rather integrates them into its varied activities.
In this manner, the DCH always saves some stations for emergencies that can develop in chronic HD programmes at the hospital or peripheral centre, as well as those derived from PD programmes or kidney transplants.
Promote condition-specific health care management
Andalusia utilises an integrated health care process for renal replacement therapy in chronic kidney failure (dialysis and kidney transplant), whose primary objective is to standardise the actions taken in patients affected with terminal chronic kidney disease that are eligible for dialysis and/or a transplant, establishing quality guidelines and criteria for correct functioning.25
The nephrology DCH is established as a key link in the health care process, and contributes to improve compliance with quality controls with regard to accessibility, delay in patient assistance, continuity of health care, response times for vascular or peritoneal accesses, management of complications, preparation for chronic dialysis, first dialysis, etc., as well as favour the resolution of problems in a single action (high resolution).
At the heart of this process, Andalusia is also currently developing a strategy for the development of PD, and our centre has been selected for training stays, with the DCH having an active participation.
Support the conservative advanced chronic kidney disease programme
One of the objectives of this programme for ACKD patients not undergoing renal replacement therapy is better home care. The administration of hospital medications such as subcutaneous EPO or intravenous iron can be performed at home, as long as agreements are established between the unit and primary care. However, in those cases in which the administration of intravenous iron at home presents problems, the patient needs a transfusion of blood derivatives, or stabilisation of hydrosaline decompensation, the DCH is an excellent alternative to frequent travelling to the emergency room, which would be the only alternative in the absence of this option.35
The DCH is also an important space for the training/information of ACKD patients.
Promote outpatient activity and the management of shared cases with primary care, including the conservative advanced chronic kidney disease programme
As a short stay unit in our department, the DCH is also a key link with primary care. From this standpoint, joint activities should be coordinated with primary care, both to resolve doubts about responsibilities and liabilities and for planning multi-level patient follow-up, including the conservative ACKD programme, making this issue closely related to the previous one. This coordination can be directed by the nephrologist in charge of the DCH, who will also coordinate the collaboration with the reference centre and corresponding health institutions.34
Make the specialty more attractive and interesting, both for current nephrologists and those in training. Promote teaching and research
In the issue number 2 of the journal Nefrología from the year 2011, there are two references that comment heavily on the progressive loss of interest towards nephrology in recent years on the part of recently graduated doctors that choose a specialty, which is progressively loosing attractiveness, choice of this internal medicine resident programme by students with worse results, etc.13,14
The factors that have been put forth to explain this situation vary, although in our opinion, the primary factor is a very limited job market with low expectations after finishing the specialty training programme, with inadequate compensation, few opportunities for private practice (without considering peripheral HD centres, which provide substantial workload), and a scarcity of professional opportunities in hospital departments that facilitate a more complete performance of this activity. If continuity is accomplished at a hospital, it is often through shift contracts, and in some cases, unfortunately, they have little effective connection with the hospital departments.
There are other causes as well, such as the content and environment for developing the specialty, the structure of the teaching programme, the lack of independence with respect to other departments (radiology, vascular surgery, etc.), and the loss of pathologies to be treated (covered by internal medicine, rheumatology, etc.)
In order to change the situation, we must not shift our attention away from the fact that the primary goal is to be a source of job opportunities and professional development for young nephrologists, which would require an adjustment of the number of quality positions available to demand. Even so, we must not forget that working habits, areas of activity, techniques and skills developed, and the pathologies attended to are also elements for stimulus.
The progressive implementation of nephrology DCH can aid in applying professional and training programmes with a greater level of innovation, enthusiasm, and intensity in our specialty.36 As we have already mentioned, they could provide a greater level of clinical independence, a recovery of some abandoned health conditions (acute renal failure, autoimmune diseases, kidney biopsy, etc.), a greater level of coordination with primary care providers, opportunities to promote new training techniques and develop interventional nephrology, which has produced interesting studies relating the learning process to results obtained,37-39 as well as generate enthusiasm, new opportunities, new lines of research, and a greater level of professional expectation and job opportunities.
Collaborate to guarantee the quality and sustainability of the national health system
We must be aware of the need to collaborate with all other sectors in the struggle to maintain the sustainability of our health system, especially in the current situation of an economic crisis, recognising for a start that the health care we provide within the health system could be greatly improved without affecting quality40: inappropriate services, variability in clinical practice, duplicity in consultations or complementary tests, inadequate coordination between health care levels, etc.
Our specialty is promoting the development of important sustainability strategies for the health system, such as the facilitation of living-donor kidney transplants and increased use of PD in the integrated treatment of terminal CKD, among others.41,42 However, we also wish to send the message that implementing nephrology DCH can favour these and other sustainability initiatives, since they allow for greater outpatient resolution of health issues, shorter hospitalisation times and improved indices and criteria for hospitalisations,43 meaning greater savings in health costs as compared to conventional hospitalisation.4 They also provide a high level of coordination between nursing staff and nephrologists, higher indeed than any other joint effort carried out in any other area of the hospital, with significant advantages in terms of treatment provided and economic costs.44 Additionally, they provide greater independence, reduced use of surgical resources and diagnostic tests in other specialties, and an overall increase in the effectiveness and efficiency of our units.
Table 1. Identification of the primary problems at acute nephrology units and the need for a nephrology day care hospital
Table 2. Procedures carried out at a day hospital during the first 8 months of functioning
Figure 1. The cycle of continuous quality improvement
Figure 10. Evolution of the mean duration (MD) of hospital stay at the nephrology clinical management unit at the Puerto Real University Hospital (HUPR) as compared to the standard MD for Andalusia and the same hospital group
Figure 2. Identification of the causes of problems. Ishikawa diagram
Figure 3. Organisational placement of the nephrology day care hospital within the clinical management unit
Figure 4. Multipurpose room with beds and chairs
Figure 5. Multipurpose room with beds and chairs (2)
Figure 6. Peritoneal dialysis unit integrated in the day care hospital
Figure 7. Interventional nephrology unit
Figure 8. Catalogue of services: procedures
Figure 9. Application for the registry of activities