INTRODUCTION
There is no consensus in the literature regarding the most appropriate choice of dialysis method. Hemodialysis (HD) and peritoneal dialysis (PD) are interchangeable and complementary renal replacement therapy (RRT) modalities.1 Although there are advantages and disadvantages of both treatment methods, it is recommended to start the treatment with PD as the first-line renal replacement modality in the absence of special conditions (contraindications) and later switch to hemodialysis.1,2
It was reported that PD was advantageous in terms of survival compared to HD in the first 2-3 years of treatment and afterwards the survival with PD was equal or worse than with HD.3,4 The studies reported a better duration and quality of life in patients who were transferred to HD following initiation with PD and receiving integrated care strategy, due to the complications such as further development of ultrafiltration problems, insufficient dialysis and/or peritonitis.1
A much smaller proportion of patients change modality from HD to PD, predominantly due to vascular access problems, cardiac disease or patient preference. There are few data about the survival in this patient population.5,6
The purpose of this study was to identify the predictors of mortality and to evaluate the clinical outcome in peritoneal dialysis patients who were transferred to PD from HD due to various causes such as vascular access problems compared to patients receiving PD as first-line therapy.
MATERIAL AND METHOD
The records of 322 patients with end stage renal disease (ESRD) receiving PD therapy in our PD unit between 2001–2010 were evaluated retrospectively. Patients, younger than 18 years, had data missing, patients switching to another clinic, patients on PD for less than 90 days and patients who recovered renal function and no longer required dialysis were excluded. The data of the remaining 299 patients were evaluated.
The age, gender, educational levels of the patients and socio-demographic characteristics such as who helped administer the PD (by themselves, their children or other persons like health carers) and the nature of the decision to PD (patient preference, his/her own decision or other compulsory choice) were investigated in-depth from patient records.
In our coutry and unit, patients have the right to choose the appropriate treatment method after they are informed about renal replacement therapies. PD preference means; preffering of PD treatment by patients themselves or as a result of mandatory indication because of many causes (vascular problems, cardiac problems, attainability of the center, etc.).
Follow-up time of PD therapy, type of PD modality (CAPD, APD), presence of HD history before PD therapy and duration of the therapies were recorded. Duration of icodextrin and hypertonic solution usages during follow-up time were recorded. Additional systemic diseases (hypertension, coronary artery disease, cerebrovascular events, malignancy etc.) and information about ESRD etiologies of all patients were recorded.
Systolic and diastolic blood pressure measurements, daily urine volumes, daily mean ultrafiltration amounts, cardiothoracic indices all of patients were recorded at the beginning of the treatment and during the last visits of PD therapy. Serum urea, creatinine, calcium, phosphorus, albumin, parathormone, hemoglobin, transferrin saturation and ferritin values were recorded at the beginning of the treatment and during the last monitoring. Infectious complications such as peritonitis, catheter exit site/tunnel infections were recorded and their incidences were calculated.
Patients were divided into two groups. Group 1 consisted of patients who received PD treatment following hemodialysis (group 1: patients with HD history) and group 2 consisted of patients who received PD as first-line threapy (group 2: patients without HD history). Socio-demographic data, clinical courses and the infectious complications (peritonitis and catheter exit site/tunnel infections) of the two groups were compared, and the reasons for PD withdrawal were obtained. Survival analysis of all patients was performed and the effect of HD on mortality was investigated.
We performed statistical analyses with the Scientific Package for Social Science (version 11.0; SPSS Inc,Chicago, IL, USA). Chi-square and Mann-Withney U test were used for nonparametric variables. Independent-samples T test for analyzing clinical and biochemical parameters between beginning and the last visit values. The Kaplan–Meier method for measuring patient survival rate was applied and a comparison of outcomes was based on the log rank test. We also analyzed the risk factors and calculated their hazard ratio (HR) for patient mortality using Cox proportional hazard model backward stepwise LR(Likelihood Ratio) method. Differences were considered statistically significant for p values less than 0.05.
RESULTS
The data of 322 patients were evaluated. Twenty three of them (13 patients have switched to another PD unit, 10 patients have been followed up for less than 90 days) were excluded. A total of 299 patients with a follow-up period of 10160 patient-months were evaluated. 167 of them were female, mean age at the onset of PD was 44.7±15.9 years and mean PD duration was 38.5±26.8 months.
A total of 48 patients, 31 of whom were female, had hemodialysis history before PD treatment (group 1), the mean age of the patients was 49.3±15.8 years, mean follow-up time 34.6±30.5 month and mean duration of hemodialysis before PD 32,8±34 (3-144) month.
Remain 251 patients, 136 of whom were females, had been assigned to PD treatment as first-line therapy without a hemodialysis history (group 2). Mean age was 43.8±15.8 years and mean follow-up time was 39.4±26 month in this group.
Group 1 patients were observed to be older (p=0.028). The reason for switching to PD from HD in 35 patients (70%) in group 1 was found to be mandatory due to vascular reasons and for the remaining 13 patients it was due to patient decision or social problems. It was found that 37 patients (74%) in this group were performing their own PD treatment by themselves. In group 2, only 25 patients (9.3%) were found to have mandatory choices due to vascular reasons and 222 patients (88.4%) were detected to perform their own treatments by themselves.
There were significantly different according preference of PD (compulsory or own decision) and who helped administer the PD therapy (by themselves or other) between two groups (p<0.001 and 0.016 respectively).
The major educational status of patients in both groups was a primary school (69% and 60.4% respectively). There was no significant difference between two groups (p=0.69).
It was found that 42 patients (87.5%) in group 1 and 217 patients (86.4%) in group 2 started treatment with CAPD. Between the two groups no significant difference was found with regard to the type of PD modality (p=0. 274).
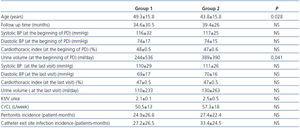
Socio-demographic characteristics of group 1 and 2 patients are shown in Table 1. At start of PD treatment, 18 patients in group 1 (37.5%) and 196 patients in group 2 (78%) had urine and mean urine volumes were 244±536 ml/day and 389±390 ml/day in group 1 and 2, retrospectively. Urine volume was significantly lower in group 1 patients at start of PD therapy (p=0.041). Ten patients (20.8%) in group 1 had diabetes as the etiologic cause of ESRD, while there were 73 diabetic patients (29%) in group 2, and no statistically significant difference was found between the two groups in terms of diabetes (p=0.70).
The biochemical and hemogram data are shown in Table 2 for both groups at the start of PD therapy and the last visit of all patients. The hemoglobin level was significantly higher in group 1 (p=0.013) at the start of PD, however this significance disappeared in time.
Peritonitis incidences and catheter exit site/tunnel infection attacks were 24.9±26.8 patient-months and 27.2±26.5 patient-months in group 1, respectively. Peritonitis incidences and catheter exit site/tunnel infection attacks were 27.4±22.4 patient-months and 33.4±24.5 patient-months in group 2, respectively. The frequency of peritonitis and catheter exit site infections were not significantly different between the two groups (p=0.50 and p=0.12, respectively).
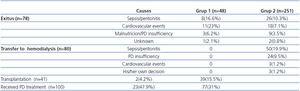
The last status data and causes of them are shown in Table 3 for both groups. During the follow-up period 25 patients were withdrawn PD therapy, 23 of them had died and 2 patients were transplanted in group 1. Interestingly, no patient was re-transferred to HD in group 1. During the follow-up period 174 patients were withdrawn PD therapy, 55 of them had died, 80 of them were transferred to HD and 39 patients were transplanted in group 2. There was a significant difference between two groups with respect to the last status of patients (p<0.001).
The most common causes of death were cardiovascular diseases (47.8%) and peritonitis and/or sepsis (34.7%) in group 1 and peritonitis and/or sepsis (47.2%) and cardiovascular diseases (32.7%) in group 2.
Mean patient survival time was 49.9±2.6 months in Kaplan–Meier analyses in patients transferred from HD to PD. The patient survival rates by Kaplan–Meier analyses were 50%, 40.9%, 27.3% and 9.1% at 1, 2, 3 and 4 years in group 1, respectively. Mean patient survival time was 55.5±2.8 months in group 2. The estimation of patient survival by Kaplan–Meier analyses was 90.9%, 81.6%, 73.9%, 64.9% and 53.1% at 1, 2, 3, 4 and 5 years, respectively in group 2. The mortality rate was found higher in patients with HD history before PD compared to patients without HD history (log rank: <0.001) (Figure 1).
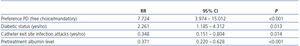
Age, preference of PD, who helped to administer the PD exchange, diabetic status, urine volume (>100ml/day or <100ml/day), pretreatment serum albumin levels, peritonitis and catheter exit site/tunnel infection attacks were analyzed using Cox proportional hazard model backward stepwise LR (Likelihood Ratio) to identify independent risk factors of mortality. Preference of PD, diabetic status, pretreatment serum albumin and catheter exit site/tunnel infection attacks were found to predict patient survival (Table 4). For each mg/dl decreases of albumin morlatity risk was elevated 3,3 times (RR: 3,376, 95% CI: 1,451-7,855, p=0,003).
DISCUSSION
HD and PD are interchangeable and complementary renal replacement therapy modalities besides transplantation. In many PD programmes, a significant percentage of patients, ranging from 15 to 25%, have been transferred from HD due to problems experienced during this therapy or patient choice.3,7,8 Another study from our country established that 12.2% of patients begin with PD as a second-line renal replacement therapy modality.9 16% of the patients evaluated in our clinic are subjects transferred from HD to PD.
Many mortality studies have been published worldwide on both treatment modalities.3,4,10,11 According to these studies, PD is known in general to have a survival advantage in the first years.3,4 Nevertheless, there are less mortality studies investigating the effects of the interchange between the therapies and they are mostly related to patients transferred from PD to HD.12,13 Studies analyzing patients transferred from HD to PD are even scarcer.5,6,14
The majority of the published studies with patients who switched to PD from HD indicate that the mortality was found worse in patients transferred from HD,15-17 although there are some studies indicating similar mortality with those who primarily started with PD.6 In our study, mortality was found worse in patients transferred to PD from HD treatment, compared with the patients initially starting with PD.
Many studies, like ours, show that a previous history of hemodialysis has a negative impact on survival,3,5,7,9,15,17 while some studies detect no influence on this parameter.6 Regarding the peritoneal dialysis, there are differences between the overall survival rates.
In peritoneal dialysis, overall survival rates show differences and this may be multifactorial reasons. Some evidences were shown to reflect the differences in mortality (particularly due to cardiovascular reasons) in general population of different countries.18,19 This discrepancy may also be the result of the demographic features (i.e. advanced age, diabetes, comorbidities, malnutrition, low residual kidney function, race, genetic factors, patient preference, etc.) of the study populations.20-25 It is well known, that the presence of diabetes and the serum albumin level at the onset of the therapy are factors influencing patient survival.9,26-28 Similar to the data of other studies we determined in our patients that advanced age, baseline serum albumin levels, presence of diabetes and frequent catheter exit site infections also increased the mortality.
The patient’s preference should be taken into account as the primary factor, since patient satisfaction, compliance with therapy and quality of life are better if the patient has been given the opportunity to make his/her own informed choice. The mandatory PD was associated with worse mortality rates among our patients. The main reasons for such transfers are vascular access problems or complications experienced during HD like intra- or postdialytic hypotension related predominantly to fluid loss during the procedure and aggravated by heart failure or cardiovascular neuropathy.5,8,15 Another study shows that most of the patients are transferred from HD to PD as a result of vascular problems.9 We found vascular problems as the cause of transfer to PD from HD in 70% of our patients. In other words, the vascular problems of patients treated with HD cause both mandatory transfer to PD and an increase in mortality because of continuing current cardiovascular problems.
Patients can be transferred from one modality to the other for various reasons and the reason of this transfer may closely affect the outcome.1 Cardiac and vascular problems are the most important causes for switching to PD from HD. In our unit, the most frequent causes of death were cardiovascular problems in patients transferred to PD from HD, while it was peritonitis/sepsis in patients without a history of HD.
RRF is very important in peritoneal dialysis, at least at the start of dialysis, because it directly affects the required dialysis dose. PD preserves residual renal function better than HD,29-31 and a clear correlation is known to exist between residual renal function and outcome.32-33 Re-analysis of the CANUSA data showed that the predictive power lays exclusively in the RRF, not in the peritoneal component, and each 250ml of daily urine output conferred a 36% reduction in mortality.34 Diaz-Buxo et al. analyzed the outcome of 1600 patients in the Fresenius database and reported that RRF, but not the dose of PD, predicted mortality.35 Van Biesen et al. discussed that HD patients which were transferred to PD usually had no RRF left and sufficient PD adequacy was more difficult to obtain in those patients.12,36 Urine outputs of patients transferred from HD to PD treatment in our unit were found to be significantly lower compared to the group that primarily initiated with PD treatment.
The initial haemoglobin level at the start of PD therapy was significantly lower in group 2. The primary reason for this difference may be the efficient erythropoietin therapy during HD treatment in group 1 and an inadequate erythropoietin substitution during predialysis period in the other group. This difference can be resolved by further erythropoietin use.
The main limitations of the present study are the retrospective design. Analysis of other factors that have also been associated with mortality, such as inflammation, renal clearance and peritoneal permeability. The presence of residual renal function were assessed by daily urine volume. Renal clearance was not calculated.
In conclusion, the mortality of patients transferred to PD from HD was found higher than of PD patients without prior HD history. The most common causes of increased mortality in patients transferred to PD from HD were compulsory choice due to vascular access problems and social reasons. The most important cause of death in patients transferred to PD from HD were cardiovascular events, whereas infectious complications were the most important cause of death in patients for whom PD was the first-line modality.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Table 1. Socio-demografic features of all patients
Table 2. Laboratory datas of two groups
Table 3. The last status data and causes of death of all patients
Table 4. Multivariate cox proportional hazards model for patient survival
Figure 1. Mortality rates of both groups